- Department of Spine Surgery, Indore Spine Centre, Indore, Madhya Pradesh, India.
Correspondence Address:
Sagar Kishor Kokate, Department of Spine Surgery, Indore Spine Centre, Indore, Madhya Pradesh, India.
DOI:10.25259/SNI_892_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Prasad R. Patgaonkar, Sagar Kishor Kokate, S. Subith, Pushkar S. Borole. Postoperative discal pseudocyst: Report of A case with an unusual complication after microlumbar discectomy and successful treatment by transforaminal endoscopic lumbar decompression. 23-Feb-2024;15:56
How to cite this URL: Prasad R. Patgaonkar, Sagar Kishor Kokate, S. Subith, Pushkar S. Borole. Postoperative discal pseudocyst: Report of A case with an unusual complication after microlumbar discectomy and successful treatment by transforaminal endoscopic lumbar decompression. 23-Feb-2024;15:56. Available from: https://surgicalneurologyint.com/surgicalint-articles/12764/
Abstract
Background: Lumbar discal pseudocysts are uncommon complications that can arise following lumbar spine surgery. It manifests as a fluid-filled sac near the intervertebral disc, causing pain and discomfort. Understanding its causes, symptoms, and management is crucial for patients and healthcare professionals involved in postoperative spinal care.
Case Description: A35-year-old female developed a discal pseudocyst after undergoing laminectomy and discectomy for lumbar disc herniation. The patient presented with recurrent lower back pain, radiculopathy, and neurological deficit two months post-surgery. Imaging revealed a discal pseudo cyst causing compression of the traversing right L5 nerve root. Given the refractory nature of her symptoms, an endoscopic procedure was offered. Using the transforaminal endoscopic technique, the pseudo cyst was identified and removed, leading to immediate symptomatic relief.
Conclusion: This article reports the rare occurrence of discal pseudocyst and highlights the use of endoscopic techniques in its surgical management. Surgeons should be aware of the minimally invasive techniques, as they can offer less morbidity, shorter recovery times, and reduced healthcare costs compared to traditional open surgery.
Keywords: Endoscopic spine surgery, Failed back surgery syndrome, Lumbar spine, Postoperative discal pseudocyst, Radiculopathy, Transforaminal endoscopic lumbar decompression
INTRODUCTION
The field of spine surgery has advanced, improving patient’s lives by addressing issues like herniated discs. Yet, there is a rare complication, postoperative discal pseudocyst, causing pain and neurological deficits, spurring the exploration of innovative treatment approaches, including minimally invasive methods. Discal pseudocysts, although rare, can significantly affect postoperative outcomes and patient quality of life. This case underscores the importance of considering minimally invasive endoscopic techniques in diagnosing and managing such complications. Early recognition and intervention are crucial in achieving favorable outcomes, reducing patient discomfort, and minimizing the risk of additional surgical procedures.
CASE PRESENTATION
A 35-year-old homemaker presented with low back pain with the right lower limb radiculopathy two months after lumbar discectomy. Initially, she was diagnosed with lumbar disc herniation at L4–L5 and underwent laminectomy and discectomy for the same at some other center. During that procedure, no nerve root or dural injuries were reported. The symptoms were relieved immediately after the procedure. The patient was discharged on the 3rd postoperative day without any residual symptoms. Within two weeks after surgery, she started experiencing lower back pain, which partially subsided with medication and physiotherapy. However, five weeks after surgery, the patient had right lower limb radiculopathy with some gait disturbances along with low back pain. The patient presented to us eight weeks after surgery with failed conservative management. She described her pain as originating from the lower back and radiating down to the dorsum of the foot. Walking, prolonged standing, and forward bending aggravated the pain. There was no history of bladder or bowel dysfunction.
On examination, she had difficulty walking on the right heel. Right L5 Gore’s sign,[
The patient underwent a comprehensive panel of hematological and serological assessments to exclude the potential presence of infection.
Imaging
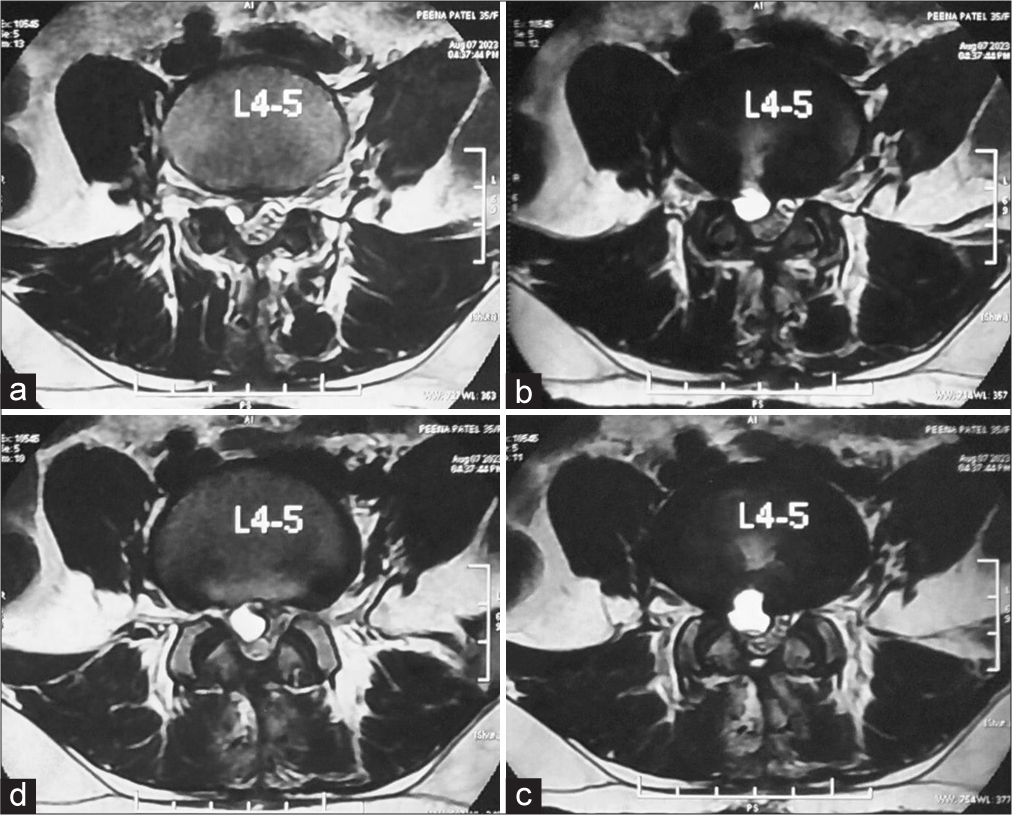
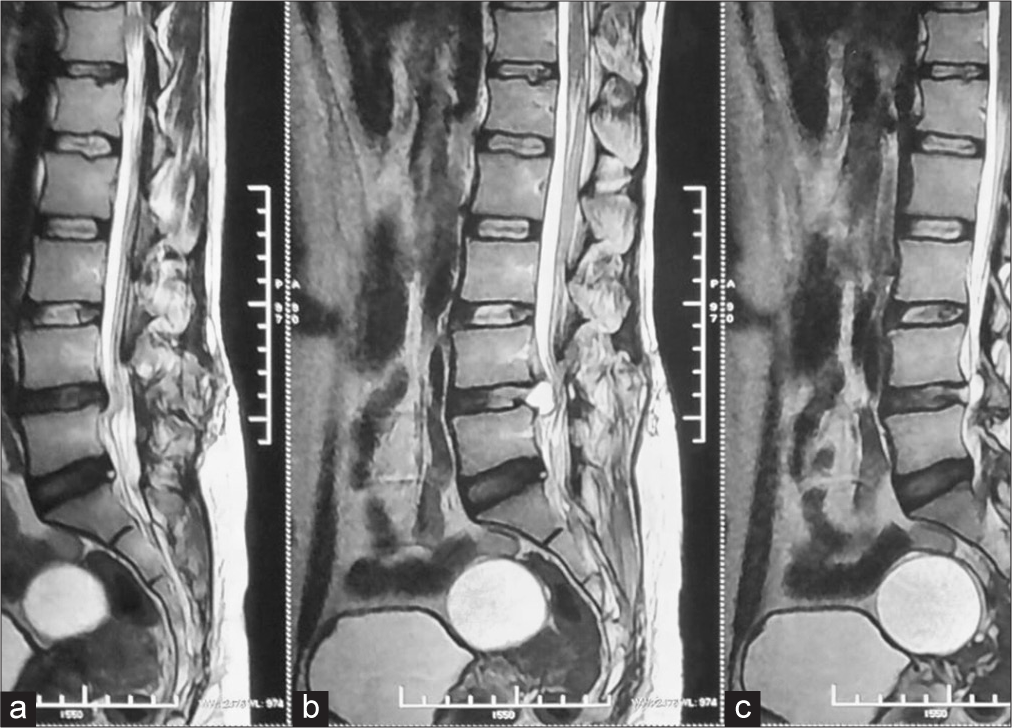
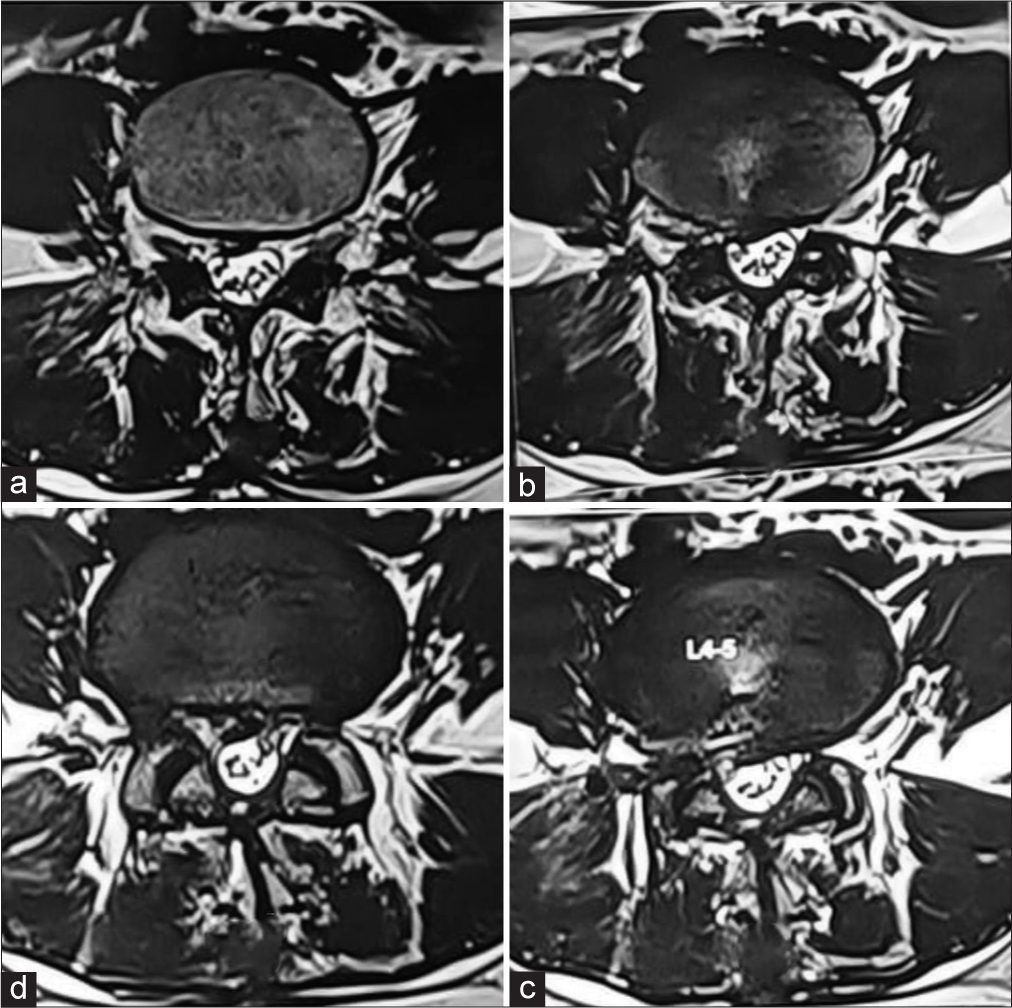
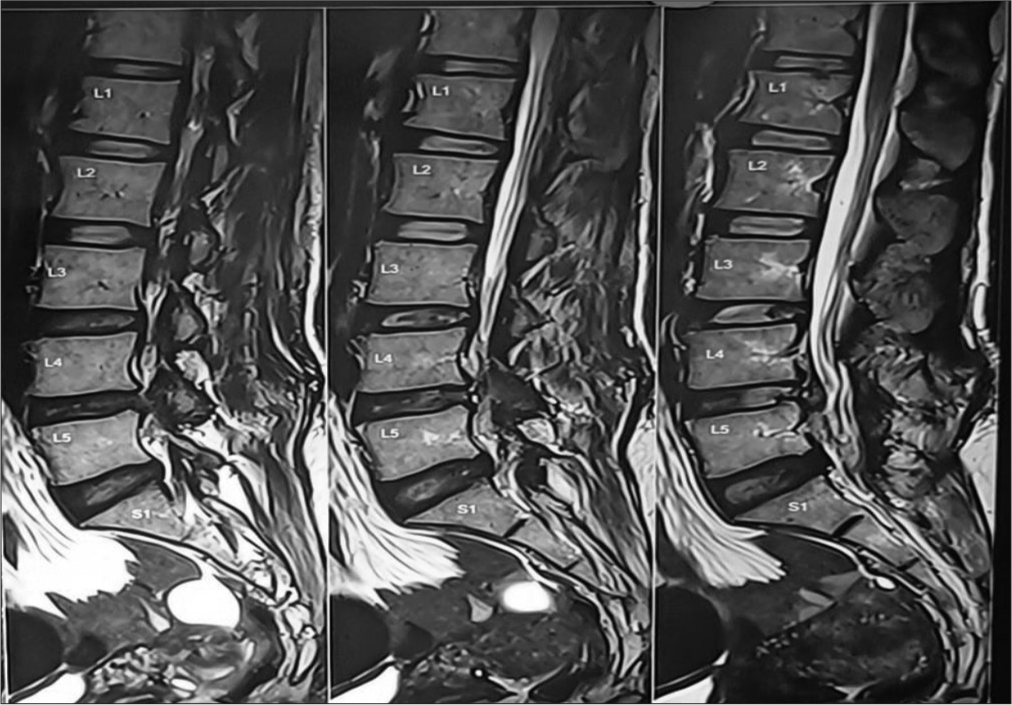
Given the new-onset pain and the weakness, a magnetic resonance imaging (MRI) scan was done [
Diagnosis
The patient’s history, clinical presentation, and radiological findings were suggestive of a possibility of the right-sided postoperative discal pseudocyst at the L4–L5 level.
TREATMENT
Planning
Given the failed conservative management, surgical option was offered to the patient. Only decompression was planned as there was no obvious radiological instability. Considering the more sagittal orientation of the facet joints, the compressive pathology being ventral to the thecal sac, and the possibility of encountering a laminectomy membrane in the interlaminar window, the transforaminal approach was planned. The FAPDIS score for the pathology was TF: IL 4.5:4.[
Procedure
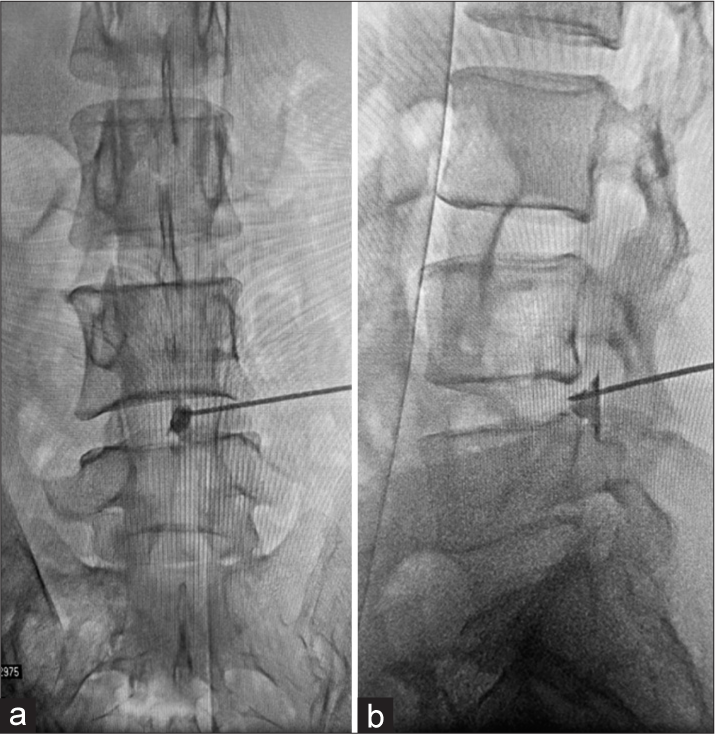
The procedure was performed in a prone position under epidural analgesia. Using an image intensifier, PL entry was marked using the YESS geometric method,[
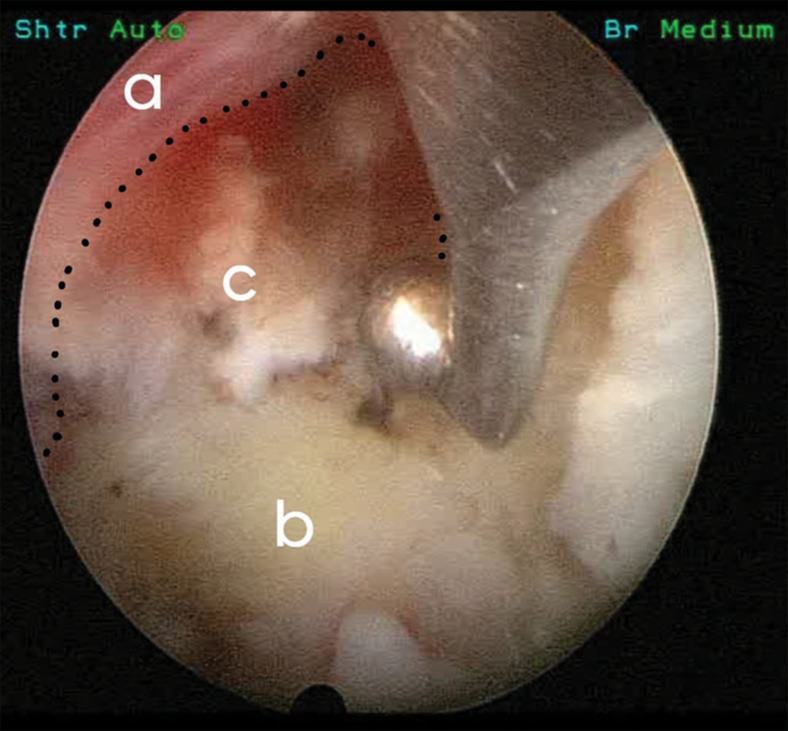
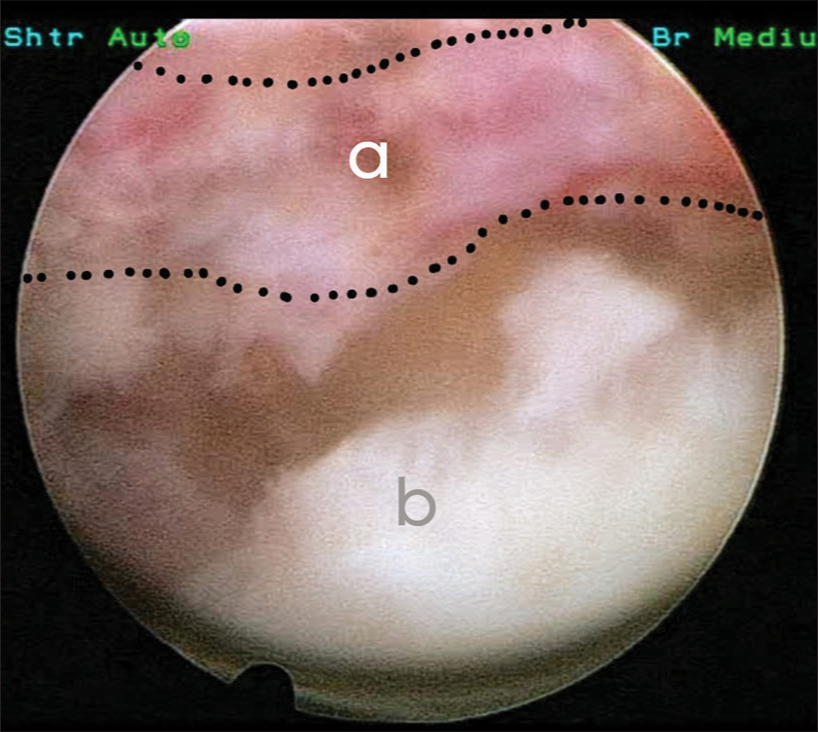
The guide wire was then placed, and the cannula was inserted. A 4.3 mm working channel endoscope was then inserted. Primary foraminotomy was performed using a RIWO tip control burr. The cyst was found to compress the thecal sac and the traversing nerve root [
Cytology
Cytological examination of aspirated fluid from the discal pseudocysts reveals the predominant presence of serous fluid, sparse erythrocytes, and the absence of epithelial cells.
Follow-up
The patient was reviewed in the outpatient department at two weeks, six weeks, and three months. Good healing of the surgical wound and a total absence of pain symptoms were noted. The postoperative MRI scan does not demonstrate any residual compressive element [
DISCUSSION
Lumbar discal pseudocysts, a rare but clinically significant complication of spine surgery, have gained recognition in recent years for their potential to cause persistent pain and neurologic deficits in postoperative patients. The clinical symptoms result from the mass effect produced by the growth of the pseudocyst, mimicking that of a recurring disc extrusion.
The precise pathogenesis of postoperative discal pseudocysts (PDP) remains undetermined; however, the existing literature posits three primary hypotheses to elucidate this phenomenon: response to epidural hematoma, pseudomembrane formation after local annulus fibrosus tear and disc degeneration; and inflammatory response to protruding nucleus pulposus. The epidural hematoma hypothesis by Chiba et al. states that epidural venous plexus hemorrhage followed by reactive inflammation leads to cyst formation. Hemosiderin deposits found in the cyst wall support this hypothesis.[
The difference between PDP and intervertebral disc cysts is that the cyst wall of PDP is incomplete, hence the name “pseudocyst.” Histologically, the wall of PDP mainly consists of dense fibrous connective tissue without epithelial lining, with serous or mucinous fluid inside.[
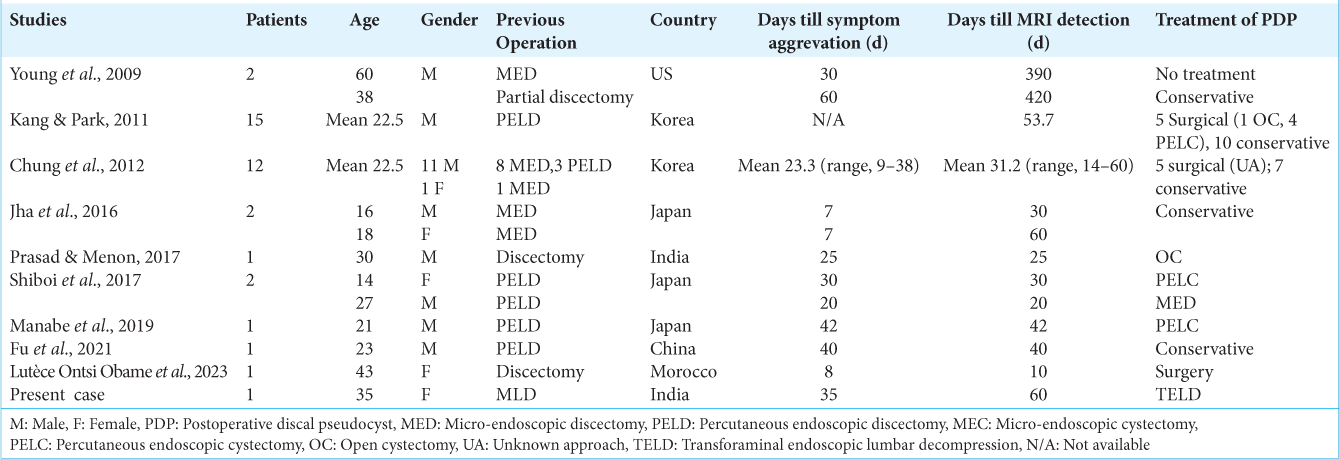
Till now, 37 cases of PDP are shown in[
The management of PDP typically involves a combination of conservative and surgical approaches, depending on the severity of the condition and the patient’s symptoms. In cases of small, asymptomatic pseudocysts, observation with regular monitoring through imaging may be a suitable approach. Non-steroidal anti-inflammatory drugs and analgesics can be prescribed to manage pain and discomfort. Physical therapy and rehabilitation exercises can help improve mobility and alleviate symptoms. Epidural steroid injections can provide temporary relief from pain and inflammation. For larger pseudocysts, percutaneous aspiration can be considered. This is typically followed by the injection of a corticosteroid to reduce inflammation.
In some cases, microdiscectomy may be necessary to remove the pseudocyst and decompress the affected nerve roots. In centers equipped with endoscopic instrumentation, the decompression can be performed using either an interlaminar or transforaminal approach. In severe cases, removal of the pseudocyst with fixation and fusion may be considered.
CONCLUSION
This article highlights the rarity but importance of discal pseudocysts, advocating for endoscopic techniques due to their ability to reduce morbidity, hasten recovery, and lower healthcare costs compared to open surgery. Embracing these advances can improve patient care and optimize healthcare resource utilization.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Aydin S, Abuzayed B, Yildirim H, Bozkus H, Vural M. Discal cysts of the lumbar spine: Report of five cases and review of the literature. Eur Spine J. 2010. 19: 1621-6
2. Chiba K, Toyama Y, Matsumoto M, Maruiwa H, Watanabe M, Nishizawa T. Intraspinal cyst communicating with the intervertebral disc in the lumbar spine: Discal cyst. Spine. 2001. 26: 2112-8
3. Chung D, Cho DC, Sung JK, Choi E, Bae KJ, Park SY. Retrospective report of symptomatic postoperative discal pseudocyst after lumbar discectomy. Acta Neurochir (Wien). 2012. 154: 715-22
4. Fu CF, Tian ZS, Yao LY, Yao JH, Jin YZ, Liu Y. Postoperative discal pseudocyst and its similarities to discal cyst: A case report. World J Clin Cases. 2021. 9: 1439-45
5. Gore S, Nadkarni S. Sciatica: Detection and confirmation by new method. Int J Spine Surg. 2014. 8: 15
6. Jha SC, Tonogai I, Higashino K, Sakai T, Takata Y, Goda Y. Postoperative discal cyst: An unusual complication after microendoscopic discectomy in teenagers. Asian J Endosc Surg. 2016. 9: 89-92
7. Kang SH, Park SW. Symptomatic post-discectomy pseudocyst after endoscopic lumbar discectomy. J Korean Neurosurg Soc. 2011. 49: 31
8. Kono K, Nakamura H, Inoue Y, Okamura T, Shakudo M, Yamada R. Intraspinal extradural cysts communicating with adjacent herniated disks: imaging characteristics and possible pathogenesis. AJNR Am J Neuroradiol. 1999. 20: 1373-7
9. Lutèce Ontsi Obame F, El Kacemi I, Diakité Y, El Asri AC, Gazzaz M. Postoperative discal pseudocyst: A case report and literature review. Interdiscip Neurosurg. 2023. 31: 101696
10. Manabe H, Higashino K, Sugiura K. A rare case of a discal cyst following percutaneous endoscopic lumbar discectomy via a transforaminal approach. Int J Spine Surg. 2019. 13: 92-4
11. Patgaonkar P, Goyal V, Agrawal U, Marathe N, Patel V. Impact of body weight, height, and obesity on selection of skin entry point for transforaminal endoscopic lumbar discectomy. Asian J Neurosurg. 2022. 17: 262-7
12. Patgaonkar P, Goyal V, Patel P, Dhole K, Ravi A, Patel V. An algorithm for selection of full endoscopic approach for symptomatic nerve root decompression. North Am Spine Soc J. 2023. 15: 100244
13. Prasad GL, Menon GR. Post-discectomy annular pseudocyst: A rare cause of failed back syndrome. Neurol India. 2017. 65: 650-2
14. Shiboi R, Oshima Y, Kaneko T, Takano Y, Inanami H, Koga H. Different operative findings of cases predicted to be symptomatic discal pseudocysts after percutaneous endoscopic lumbar discectomy. J Spine Surg Hong Kong. 2017. 3: 233-7
15. Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome, and complications in 307 consecutive cases. Spine. 2002. 27: 722-31
16. Young PM, Fenton DS, Czervionke LF. Postoperative annular pseudocyst: Report of two cases with an unusual complication after microdiscectomy, and successful treatment by percutaneous aspiration and steroid injection. Spine J. 2009. 9: e9-15