- Department of Orthopaedic Surgery, Eastern Chiba Medical Center, Togane, Japan.
- Department of Orthopaedic Surgery, University of Tsukuba, Tsukuba, Japan.
- Department of Orthopaedic Surgery, Toho University Sakura Medical Center, Sakura, Japan.
- Department of Orthopaedic Surgery, Chiba University, Chiba, Japan.
Correspondence Address:
Yasuchika Aoki, Department of Orthopaedic Surgery, Eastern Chiba Medical Center, Togane, Japan.
DOI:10.25259/SNI_138_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kosuke Takeda1, Yasuchika Aoki1, Takayuki Nakajima1, Yusuke Sato1, Masashi Sato1, Satoshi Yoh1, Hiroshi Takahashi2, Arata Nakajima3, Yawara Eguchi4, Sumihisa Orita4, Kazuhide Inage4, Yasuhiro Shiga4, Koichi Nakagawa3, Seiji Ohtori4. Postoperative loss of correction after combined posterior and anterior spinal fusion surgeries in a lumbar burst fracture patient with Class II obesity. 20-May-2022;13:210
How to cite this URL: Kosuke Takeda1, Yasuchika Aoki1, Takayuki Nakajima1, Yusuke Sato1, Masashi Sato1, Satoshi Yoh1, Hiroshi Takahashi2, Arata Nakajima3, Yawara Eguchi4, Sumihisa Orita4, Kazuhide Inage4, Yasuhiro Shiga4, Koichi Nakagawa3, Seiji Ohtori4. Postoperative loss of correction after combined posterior and anterior spinal fusion surgeries in a lumbar burst fracture patient with Class II obesity. 20-May-2022;13:210. Available from: https://surgicalneurologyint.com/surgicalint-articles/11606/
Abstract
Background: When treating thoracolumbar fractures with severe cranial endplate injury but no or slight caudal endplate injury, it is debatable whether anterior fusion should be performed only for the injured cranial level, or for both cranial and caudal levels. We report an unexpected postoperative correction loss after combined multilevel posterior and single-level anterior fusion surgery in a patient with obesity.
Case Description: A 28-year-old male with Class II obesity was brought to the emergency room with an L1 burst fracture with spinal canal involvement. Cranial endplate injury was severe, whereas caudal endplate injury was mild. The first surgery with 1-above 1-below posterior fixation failed to achieve sufficient stability; thus, additional surgeries (3-above 3-below posterior fixation and single-level T12-L1 anterior fusion) were performed. Postoperatively, the local kyphosis angle (LKA) between T12 and L2 was 22° in the lateral lying position and 29° in the standing position. Twenty-one-month post surgery, bony fusion between T12 and L1 was observed, and the LKA was 28° in both the lateral lying and standing positions. After posterior implants were removed 24 months after the surgery, significant correction loss both at the T12-L1 segment (6°) and L1-L2 segment (6°) occurred, and LKA was 40° at the final follow-up.
Conclusion: In this patient, an intense axial load due to excessive body weight was at least one of the causes of postoperative correction loss. Postural differences in LKA may be useful to evaluate the stability of thoracolumbar fractures after fusion surgery and to predict postoperative correction loss.
Keywords: Anterior fusion, Correction loss, Kyphosis, Obesity, Thoracolumbar fracture
INTRODUCTION
Thoracolumbar fractures and dislocations, particularly those with spinal cord or cauda equina injuries, are often treated with spinal decompression and fusion surgery. Recently, the safety and efficacy of posterior short-segment instrumentation for the treatment of thoracolumbar fractures have been reported; thus, posterior pedicle screw fixation is recommended by many surgeons.[
When treating such patients with spinal fusion surgery, it is debatable whether anterior fusion should be performed only for the injured cranial level (single-level) or for cranial and caudal levels (two levels).[
The increase of patients with obesity, which is associated with adverse health consequences throughout the life course, is a common problem in countries worldwide.[
Previously, it was reported that obesity is a risk factor for correction loss after spinal fusion surgery for thoracolumbar fractures.[
CASE REPORT
History, examination, and first surgery
A 28-year-old man who worked as a steeplejack was brought to the emergency room with a lumbar burst fracture at the L1 level caused by a fall from a 6-m height. He had no comorbidities except Class II obesity (height, 178 cm; weight, 117 kg; and BMI, 36.9 kg/m2). On arrival, the patient was alert and oriented, but complained of severe back pain, bilateral lower-extremity pain, and numbness. Although accurate neurological evaluation was difficult because of severe back and lower extremity pain, the weakness of the bilateral lower extremities (Medical Research Council grade 3–4) and no sensory decline by the pin-prick test was observed.
Initial radiographic examination including computed tomography (CT) scan and magnetic resonance imaging showed burst fracture at the L1 level with spinal cord and cauda equina compression, which was classified as AO type B2 with spinous process fracture at L1 and L2 [
Figure 1:
Preoperative CT images: sagittal view (a) and axial views (b and c). Lines (b) and (c) indicate axial slices shown in b and c, respectively (a). Preoperative magnetic resonance images: sagittal view (d) and axial views (e and f). Lines (e) and (f) indicate axial slices shown in (e) and (f), respectively (d).
The patient was temporarily immobilized with a bedrest and the first surgery was performed 2 days after the trauma. During the surgery, pedicle screws (Universal Spine System II, Depuy Synthes, Zuchwil, Switzerland) were inserted bilaterally to the T12 and L2 levels after partial laminectomy at the T12 and L1 vertebrae for decompression were performed [
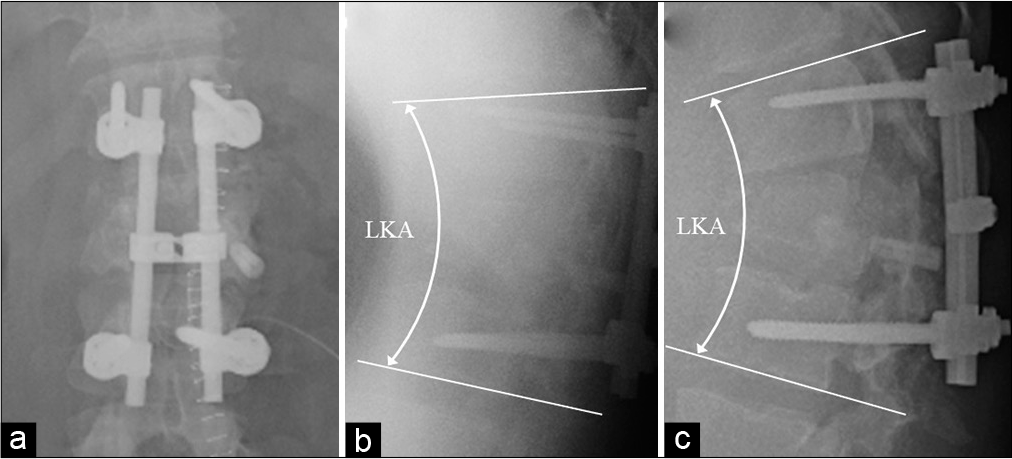
Figure 2:
Postoperative radiographs taken in operating theatre in lying position (anteroposterior view in supine position: a, and lateral view in prone position: b), and taken in standing position 14 days after the first surgery (c). Local kyphosis angle (LKA) between T12 and L2 was 16° in prone position (b) and 32° in standing position (c).
Postoperatively, the patient’s back and lower extremity symptoms improved when compared with preoperatively; however, the patient was unable to stand because of severe back pain in the standing position. Eight days after surgery, the patient was able to stand; thus, radiographs of the thoracolumbar spine were taken in the standing position 14 days after the surgery. LKA was 32° in the standing position [
Second and third surgery
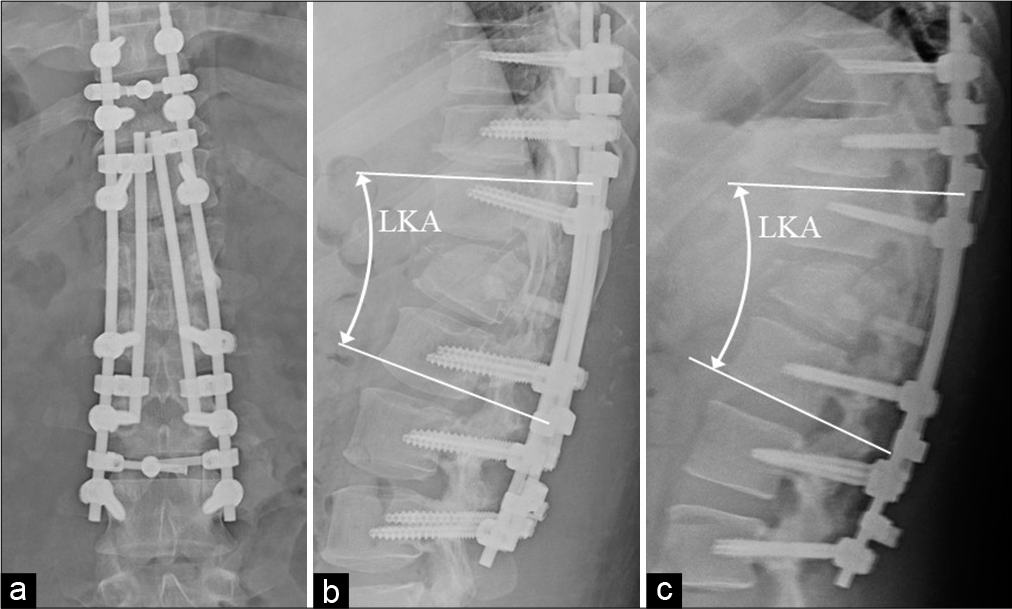
Twenty-two days after the first surgery, a second surgery was performed. All implants, including pedicle screws inserted at the first surgery, were removed, and pedicle screws of other systems (Expedium Spine System, Depuy Synthes, Zuchwil, Switzerland) were inserted at the T10, T11, T12, L2, L3, and L4 levels. On each side, the pedicle screws from T10 to L4 levels were connected by two rods to reinforce the stability of the screw-rod system [
Forty-four days after the second surgery, a third surgery was performed. At the third surgery, the left eleventh rib was harvested, and the left lateral aspect of the T12-L1 vertebra was exposed through the retropleural approach. Subsequently, the T12-L1 disc and a part of the injured L1 vertebra were removed, and autologous rib strut grafts were inserted [
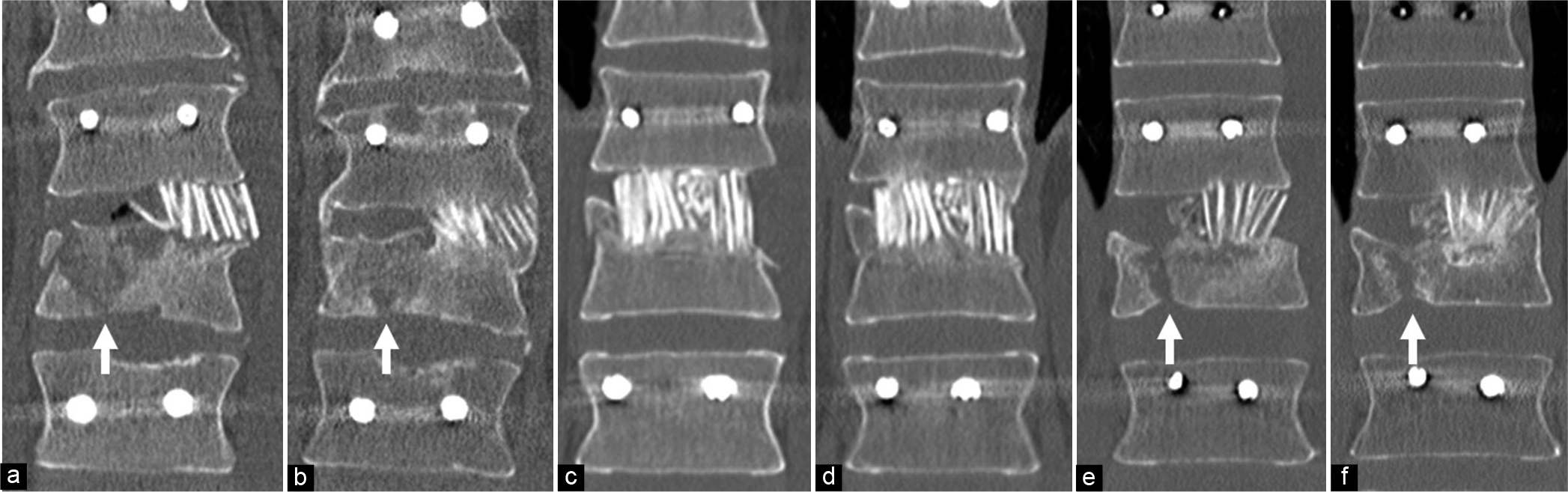
Figure 4:
Coronal reconstruction CT images showing location of rib graft bone and caudal endplate injury. CT images of this patients (Case 1) taken a week (a) and 21 months (b) after anterior fusion surgery, showing mild caudal endplate injury (white arrows in a and b) and unilaterally located graft bones (a, b). The continuity of trabecular bone between T12 and L1 vertebrae were observed 21 months after the surgery (b). CT images of Case 2 in Table 1 taken a week (a) and 14 months (b) after anterior fusion surgery, showing no injury at the caudal endplate and graft bones widely located at the fractured site (c, d), and bony fusion was observed 14 months after the surgery (d). CT images of Case 3 in Table 1 taken a week (e) and 21 months (f) after anterior fusion surgery, showing radiologic findings similar to Case 1 (mild caudal endplate injury [white arrows in e and f] and unilaterally located graft bones). The continuity of trabecular bone at the fractured site was observed 21 months after the surgery (f).
Postoperative course after the third surgery
The postoperative course after the third surgery was favorable, with no postoperative complications. Back pain gradually decreased postoperatively, and the muscle weakness of the lower extremities returned to normal; however, slight residual back pain and foot numbness remained after the third surgery.
Bony fusion was evaluated on reconstructed sagittal and coronal CT images. The full integration of a bone graft at both adjacent levels was considered as complete bony fusion.[
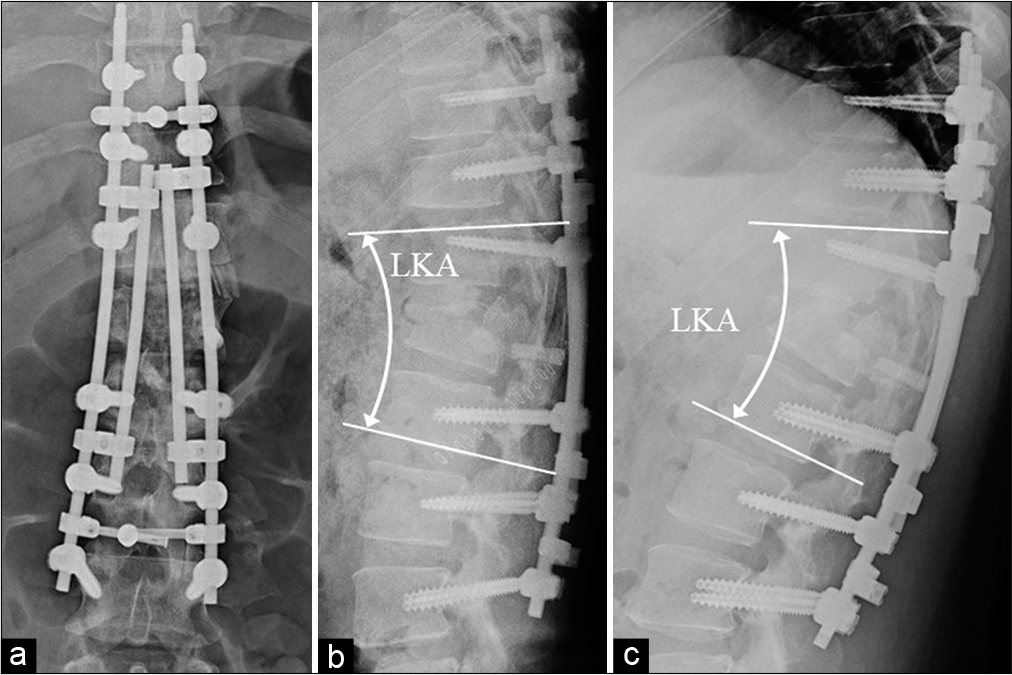
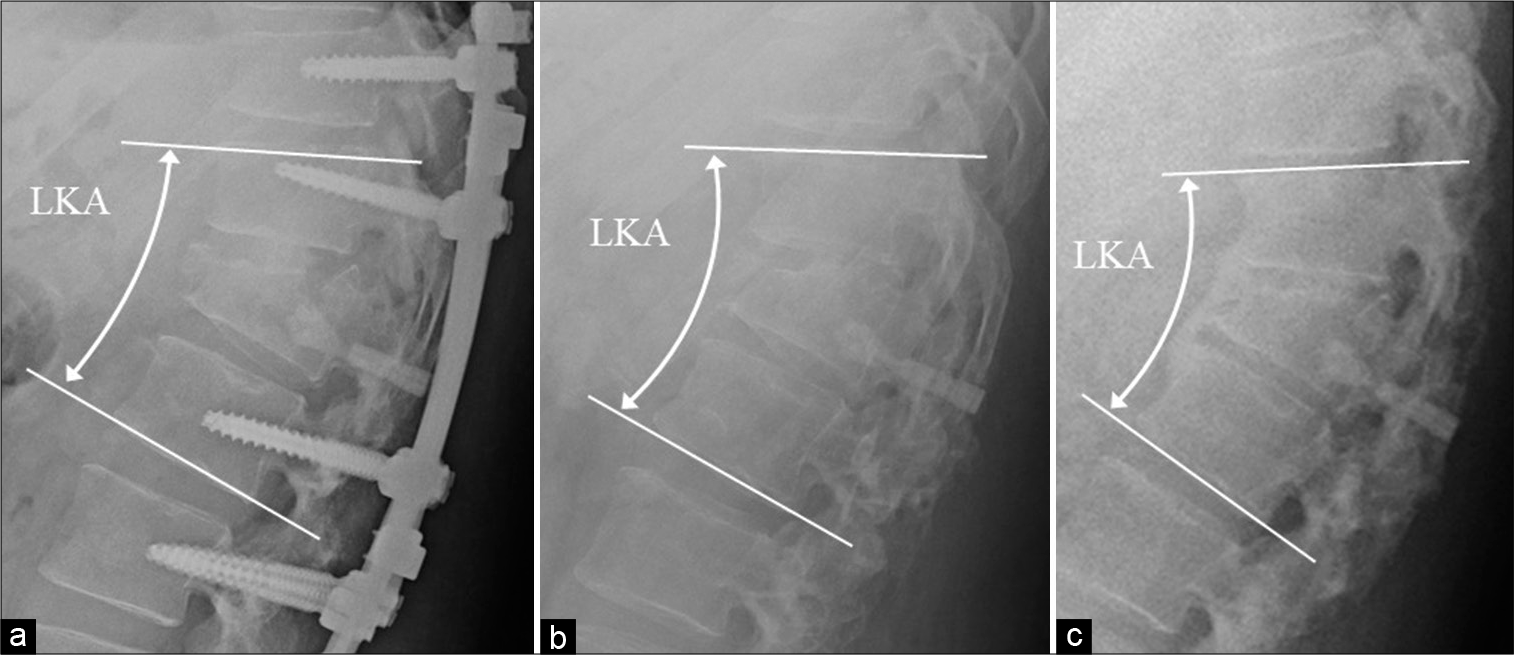
Figure 6:
Lateral radiographs taken in standing position 21 months (before removal, a), 24 months (after removal, b), and 51 months (final follow-up, c) after the anterior fusion surgery. Local kyphosis angle (LKA) between T12 and L2 was 28° before removal (a), 30° after removal (b), and 40° at the final follow-up (c).
At the final follow-up (27 months after the removal), the patient was able to walk and jog without any support; however, slight back pain and slight left foot numbness were reported. He did not return to work as a steeplejack as he was hesitant to work from heights again; however, his activities of daily life had returned to normal and started work in the construction industry.
DISCUSSION
A favorable surgical outcome of single-level anterior fusion was reported in patients with thoracolumbar burst fracture in which the cranial endplate is mainly involved and the caudal endplate has no or slight injury.[
In our institution, thoracolumbar fracture patients requiring surgical intervention are usually treated with posterior fusion surgery using pedicle screws at an early post trauma period, particularly when they have multiple traumas. After the first surgery, additional anterior fusion surgery can be considered as an elective surgery. In cases where the caudal endplate has no or slight injury, we usually performed single-level anterior fusion at the cranial level. However, it is still debatable whether single-level or two-level anterior fusion is better when treating such patients.[
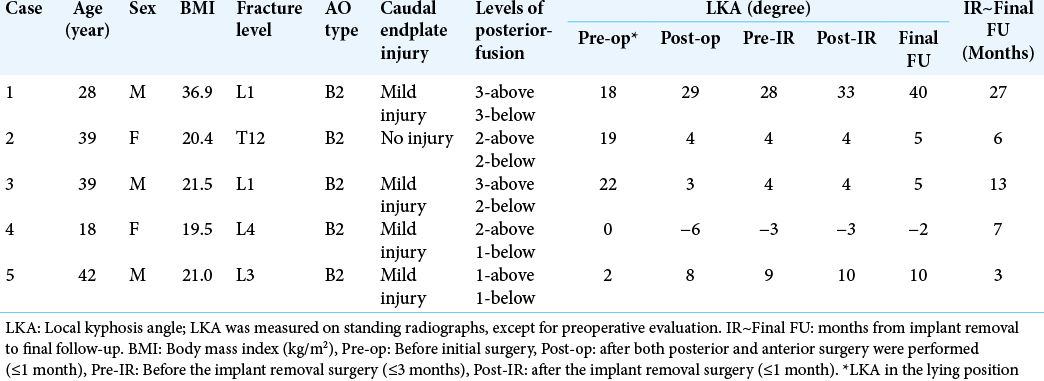
Except for this patient, we have several thoracolumbar or lumbar burst fracture patients with cranial endplate injury but no or slight injury at the caudal endplate. Among these patients, four were treated with the same surgical strategy and followed up until their posterior implants were removed. All four patients had posterior ligamentous complex injury and were classified as having an AO type B2 injury, were not obese, and showed no obvious correction loss even after implant removal [
At present, the cutoff value of a patient’s BMI (or body weight) for predicting postoperative significant correction loss is unclear. Thus, to predict the possibility of postoperative correction loss, we focused on the difference in LKA between the lying and standing positions after posterior fusion surgery without anterior support. In our patient, LKA was obviously larger in the standing position than in the supine position after the first posterior fusion, suggesting that the 1-above 1-below posterior pedicle screw fixation was insufficient to stabilize the injured thoracolumbar spine in the patient. Moreover, even after 3-above 3-below posterior fixation using four rods, LKA in the standing position was considerably larger than that in the lying position. These findings suggest that sufficient stability was not obtained even by 3-above 3-below posterior fusion surgery, possibly due to the patient’s body weight and severity of fracture. In this patient, such insufficient stability may cause subsidence of the graft bone to the fractured vertebra after anterior fusion surgery. In the early postoperative period after the third surgery, LKA was 22° in the lateral position and 29° in the standing position. However, the LKA was 28° both in the lateral lying and standing positions before implant removal, suggesting that the final LKA before implant removal is predicted by postoperative standing radiographs.
Moreover, correction loss occurred after implant removal at both fractured and caudal discs. As reviewed by Kweh et al., in younger patients with thoracolumbar burst fractures treated by posterior stabilization, planned implant removal induced superior functional outcomes without a significant difference in correction loss compared to implant retention.[
Previously, it was reported that there is a difference in lumbar sagittal alignment depending on posture.[
CONCLUSION
When treating thoracolumbar burst fracture with cranial endplate injury but no or slight injury at the caudal disc by two-stage posterior and anterior fusion surgery, comparison of local alignment between standing and lying positions after posterior fusion surgery is recommended to evaluate the postoperative stability of the injured spine, particularly in obese patients. In cases where stability is insufficient, surgeons should consider additional longer levels of posterior fixation and/or two-level anterior fusion surgery, including an intact caudal disc, to prevent postoperative correction loss.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Acaroglu ER, Schwab FJ, Farcy JP. Simultaneous anterior and posterior approaches for correction of late deformity due to thoracolumbar fractures. Eur Spine J. 1996. 5: 56-62
2. Antoni M, Charles YP, Walter A, Schuller S, Steib JP. Fusion rates of different anterior grafts in thoracolumbar fractures. J Spinal Disord Tech. 2015. 28: E528-33
3. Aoki Y, Inoue M, Takahashi H, Nakajima A, Sonobe M, Terajima F. Postoperative change in lumbopelvic alignment after short-segment transforaminal lumbar interbody fusion is related to preoperative postural difference in lumbar lordosis. J Orthop Sci. 2021. p.
4. Aoki Y, Iwakura N, Sugioka K, Ikeda O, Tokunaga M, Maruta T. Magnetic resonance imaging of intervertebral discs in elderly patients with vertebral compression fractures due to minor trauma. Internet J Spine Surg. 2006. 2: 1-7
5. Chevillotte T, Coudert P, Cawley D, Bouloussa H, Mazas S, Boissière L. Influence of posture on relationships between pelvic parameters and lumbar lordosis: Comparison of the standing, seated, and supine positions. A preliminary study. Orthop Traumatol Surg Res. 2018. 104: 565-8
6. Cimatti M, Forcato S, Polli F, Miscusi M, Frati A, Raco A. Pure percutaneous pedicle screw fixation without arthrodesis of 32 thoraco-lumbar fractures: Clinical and radiological outcome with 36-month follow-up. Eur Spine J. 2013. 22: S925-32
7. Formica M, Cavagnaro L, Basso M, Zanirato A, Felli L, Formica C. Which patients risk segmental kyphosis after short segment thoracolumbar fracture fixation with intermediate screws?. Injury. 2016. 47: S29-34
8. Fukuda K, Katoh H, Takahashi Y, Kitamura K, Ikeda D. Minimally invasive anteroposterior combined surgery using lateral lumbar interbody fusion without corpectomy for treatment of lumbar spinal canal stenosis associated with osteoporotic vertebral collapse. J Neurosurg Spine. 2021. p.
9. Kweh BT, Tan T, Lee HQ, Hunn M, Liew S, Tee JW. Implant removal versus implant retention following posterior surgical stabilization of thoracolumbar burst fractures: A systematic review and meta-analysis. Global Spine J. 2022. 12: 700-18
10. Machino M, Yukawa Y, Ito K, Nakashima H, Kato F. Posterior/anterior combined surgery for thoracolumbar burst fractures--posterior instrumentation with pedicle screws and laminar hooks, anterior decompression and strut grafting. Spinal Cord. 2011. 49: 573-9
11. McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976). 1994. 19: 1741-4
12. Miyakoshi N, Abe E, Shimada Y, Hongo M, Chiba M, Sato K. Anterior decompression with single segmental spinal interbody fusion for lumbar burst fracture. Spine (Phila Pa 1976). 1999. 24: 67-73
13. Nakano S, Inoue M, Takahashi H, Kubota G, Saito J, Norimoto M. Effects of the difference between lumbar lordosis in the supine and standing positions on the clinical outcomes of decompression surgery for lumbar spinal stenosis. J Neurosurg Spine. 2022. 36: 542-8
14. 15. Ohyama S, Aoki Y, Inoue M, Nakajima T, Sato Y, Watanabe A. Predictors of spontaneous restoration of lumbar lordosis after single-level transforaminal lumbar interbody fusion for degenerative lumbar diseases. Spine Surg Relat Res. 2021. 5: 397-404 16. Oner FC, van der Rijt RR, Ramos LM, Dhert WJ, Verbout AJ. Changes in the disc space after fractures of the thoracolumbar spine. J Bone Joint Surg Br. 1998. 80: 833-9 17. Pan XM, Li W, Huang X, Deng SL, Qu B, Fan L. Single level anterior interbody fusion and fixation in the treatment of thoracolumbar fractures. J Back Musculoskelet Rehabil. 2014. 27: 499-505 18. Park SA, Kwak DS, Cho HJ, Min DU. Changes of spinopelvic parameters in different positions. Arch Orthop Trauma Surg. 2017. 137: 1223-32 19. Sander AL, Laurer H, Lehnert T, El Saman A, Eichler K, Vogl TJ. A clinically useful classification of traumatic intervertebral disk lesions. AJR Am J Roentgenol. 2013. 200: 618-23 20. Sanli I, Spoor A, Muijs SPJ, Öner FC. Less invasive surgery is feasible in the management of traumatic thoracolumbar fractures in isolated and polytrauma injury. Int J Spine Surg. 2019. 13: 561-7 21. Tang J, Liu Y, Hu Y, Cao Z, Lu X, Lin B. Anterior decompression with single segmental spinal interbody fusion for Denis Type B thoracolumbar burst fracture: A midterm follow-up study. Int Orthop. 2013. 37: 2205-9 22. Tian F, Tu LY, Gu WF, Zhang EF, Wang ZB, Chu G. Percutaneous versus open pedicle screw instrumentation in treatment of thoracic and lumbar spine fractures: A systematic review and meta-analysis. Medicine (Baltimore). 2018. 97: e12535 23. Vaccaro AR, Lim MR, Hurlbert RJ, Lehman RA, Harrop J, Fisher DC. Surgical decision making for unstable thoracolumbar spine injuries: Results of a consensus panel review by the Spine Trauma Study Group. J Spinal Disord Tech. 2006. 19: 1-10 24. Whang PG, Vaccaro AR. Thoracolumbar fractures: anterior decompression and interbody fusion. J Am Acad Orthop Surg. 2008. 16: 424-31 25. Wood KB, Li W, Lebl DR, Ploumis A. Management of thoracolumbar spine fractures. Spine J. 2014. 14: 145-64 26. 27. Wu AM, Zheng YJ, Lin Y, Wu YS, Mao FM, Ni WF. Transforaminal decompression and interbody fusion in the treatment of thoracolumbar fracture and dislocation with spinal cord injury. PLoS One. 2014. 9: e105625 28. Wu H, Zhao DX, Jiang R, Zhou XY. Surgical treatment of Denis Type B thoracolumbar burst fracture with neurological deficiency by paraspinal approach. Braz J Med Biol Res. 2016. 49: e5599 29. Zhu C, Wang B, Yin J, Liu XH. A comparison of three different surgery approaches and methods for neurologically intact thoracolumbar fractures: A retrospective study. J Orthop Surg Res. 2021. 16: 306