- Department of Translational Research and of New Surgical and Medical Technologies, University of Pisa, Pisa,
- Department of Human Neurosciences, Neurosurgery, UOD Emergency Orthopaedic Traumatology, Sapienza University of Rome, Piazzale Aldo Moro, Roma,
- Department of Neurosurgery, Azienda Ospedaliera Universitaria Pisana, Pisa, Italy.
Correspondence Address:
Nicola Montemurro
Department of Neurosurgery, Azienda Ospedaliera Universitaria Pisana, Pisa, Italy.
DOI:10.25259/SNI_697_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nicola Montemurro1, Giorgio Santoro2, Walter Marani3, Giandomenico Petrella3. Posttraumatic synchronous double acute epidural hematomas: Two craniotomies, single skin incision. 11-Dec-2020;11:435
How to cite this URL: Nicola Montemurro1, Giorgio Santoro2, Walter Marani3, Giandomenico Petrella3. Posttraumatic synchronous double acute epidural hematomas: Two craniotomies, single skin incision. 11-Dec-2020;11:435. Available from: https://surgicalneurologyint.com/surgicalint-articles/10441/
Abstract
Background: Double epidural hematomas (EDHs) have a higher mortality rate compared to single EDHs and same Glasgow Coma Scale (GCS), although double EDHs incidence is less common.
Case Description: We present the case of a 34-year-old female who underwent single skin incision and frontotemporal and suboccipital craniotomies for fatal traumatic double acute EDHs, then, a literature review was performed.
Conclusion: Double EDHs in association with low GCS at presentation and traumatic diastasis of cranial sutures or other maxillofacial injuries are associated to an unfavorable outcome.
Keywords: Epidural hematoma, Neurotrauma, Traumatic brain injury
Double epidural hematomas (EDHs) have an overall incidence of 2–9% of all EDHs.[
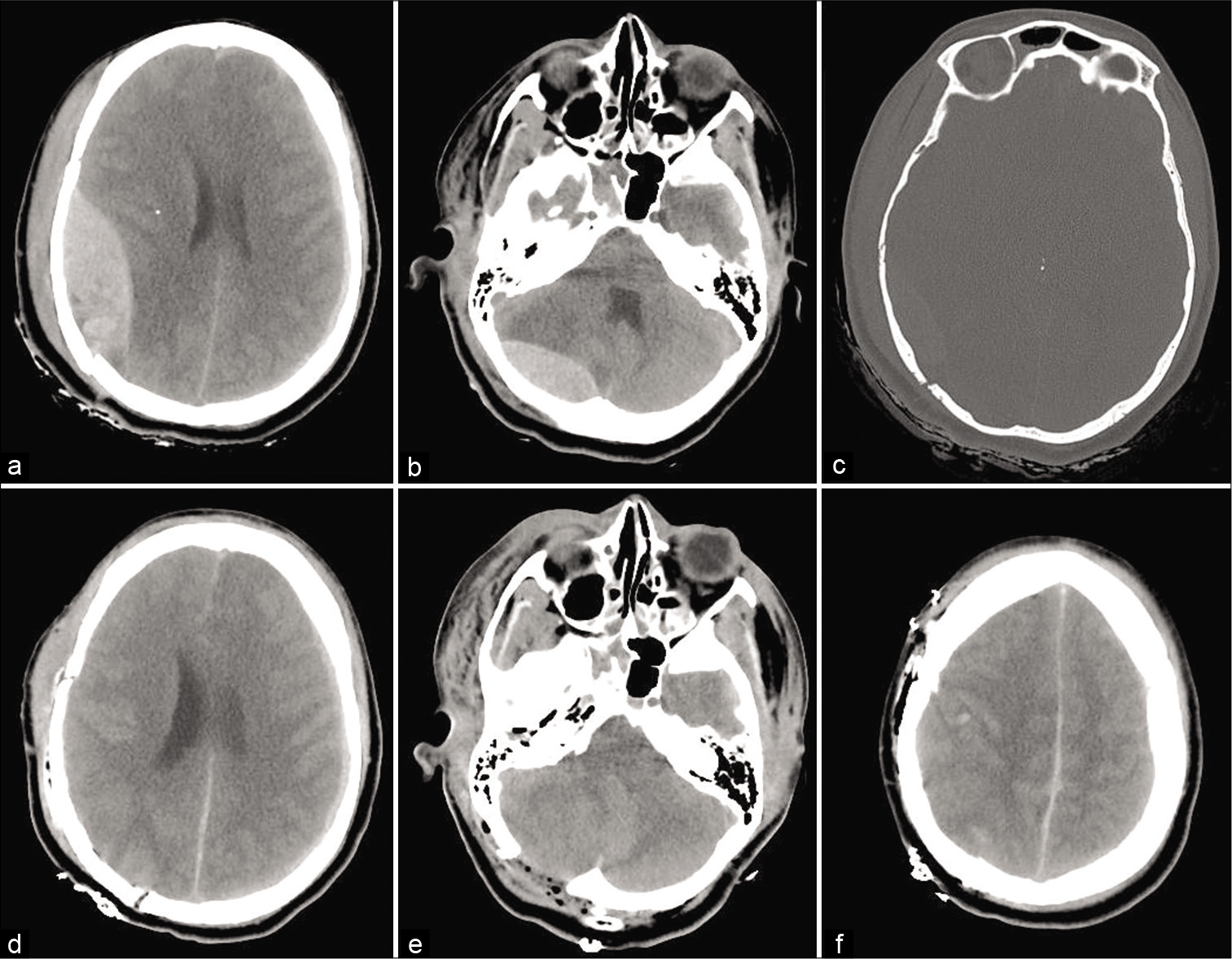
We present the case of a 34-year-old female who underwent single skin incision and frontotemporal and suboccipital craniotomies for fatal traumatic double acute EDHs. Her neurological examination on admission was poor (GCS 7). Computed tomography (CT) scans [
Figure 1:
Preoperative noncontrast CT head scans show a right temporal epidural hematomas (EDHs) (a), a right posterior cranial fossa EDH (b), and a temporal bone fracture with diastasis of the lambdoid suture (c). Postoperative CT head scans (d-f) show evacuation of EDHs and resolution of the downward herniation.
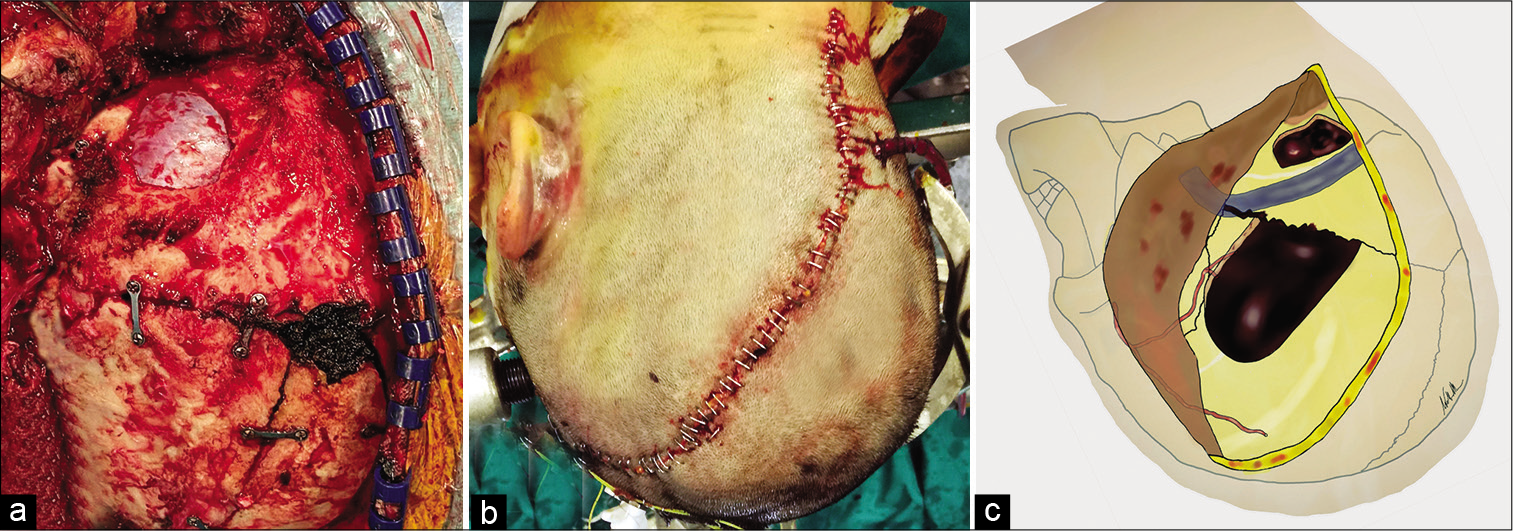
Figure 2:
Intraoperative (a) and postoperative (b) pictures show two different craniotomies and a single C-shaped skin incision starting from the right frontal region and ending to C1 level. Illustration depicting (c) shows the middle meningeal artery, transverse and sigmoid sinuses, and the craniotomies performed during surgery.
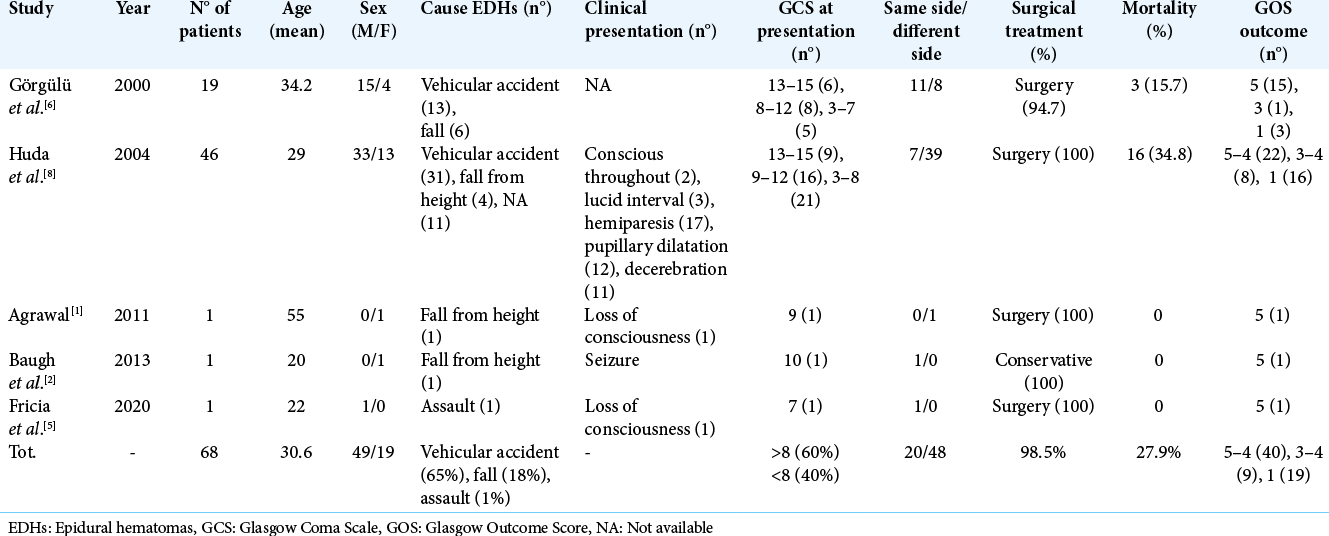
From a literature review, 68 cases were found with double EDHs.[
EDHs arise from injury to the MMA or from its terminal arterial branches in about 55% of the patients, from the middle meningeal vein in 30% of cases and from diploic veins or a torn dural venous sinus in the remaining 15% of cases.[
The authors hope this case report and literature review could increase the awareness of the fatal consequences of double EDH associated with diastasis of the lambdoid suture. Double EDHs in association with low GCS at presentation and traumatic diastasis of cranial sutures or other maxillofacial injuries lead to a poor prognosis. This paper confirms what it is strongly recommended, that is, surgical evacuation as soon as possible in patients with acute single or double EDHs with a GCS score <9.[
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Agrawal A. Bilateral symmetrical parietal extradural hematoma. J Surg Tech Case Rep. 2011. 3: 34-6
2. Baugh AD, Baugh RF, Atallah JN, Gaudin D, Williams M. Craniofacial trauma and double epidural hematomas from horse training. Int J Surg Case Rep. 2013. 4: 1149-52
3. Benedetto N, Gambacciani C, Montemurro N, Morganti R, Perrini P. Surgical management of acute subdural haematomas in elderly: Report of a single center experience. Br J Neurosurg. 2017. 31: 244-8
4. Bullock MR, Chesnut R, Ghajar J, Gordon D, Hartl R, Newell DW. Surgical management of acute epidural hematomas. Neurosurgery. 2006. 58: S7-15
5. Fricia M, Umana GE, Scalia G, Raudino G, Passanisi M, Spitaleri A. Posttraumatic triple acute epidural hematomas: First report of bilateral synchronous epidural hematoma and a third delayed. World Neurosurg. 2020. 133: 212-5
6. Görgülü A, Cobanoglu S, Armagan S, Karabagli H, Tevrüz M. Bilateral epidural hematoma. Neurosurg Rev. 2000. 23: 30-3
7. Holzschuh M, Schuknecht B. Traumatic epidural haematomas of the posterior fossa: 20 new cases and a review of the literature since 1961. Br J Neurosurg. 1989. 3: 171-80
8. Huda MF, Mohanty S, Sharma V, Tiwari Y, Choudhary A, Singh VP. Double extradural hematoma: An analysis of 46 cases. Neurol India. 2004. 52: 450-2
9. Montemurro N, Murrone D, Romanelli B, Ierardi A. Postoperative textiloma mimicking intracranial rebleeding in a patient with spontaneous hemorrhage: Case report and review of the literature. Case Rep Neurol. 2020. 12: 7-12
10. Ng SY, Lee AY. Traumatic brain injuries: Pathophysiology and potential therapeutic targets. Front Cell Neurosci. 2019. 13: 528