- Department of Spine Surgery, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
DOI:10.25259/SNI_567_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: G. Sudhir, Vignesh Jayabalan, T. H. Manohar, Saikrishna Gadde, Venkatesh Kumar, Karthik Kailash. Posttraumatic thoracic epidural capillary hemangioma – A rare case report. 11-Jul-2020;11:179
How to cite this URL: G. Sudhir, Vignesh Jayabalan, T. H. Manohar, Saikrishna Gadde, Venkatesh Kumar, Karthik Kailash. Posttraumatic thoracic epidural capillary hemangioma – A rare case report. 11-Jul-2020;11:179. Available from: https://surgicalneurologyint.com/surgicalint-articles/10121/
Abstract
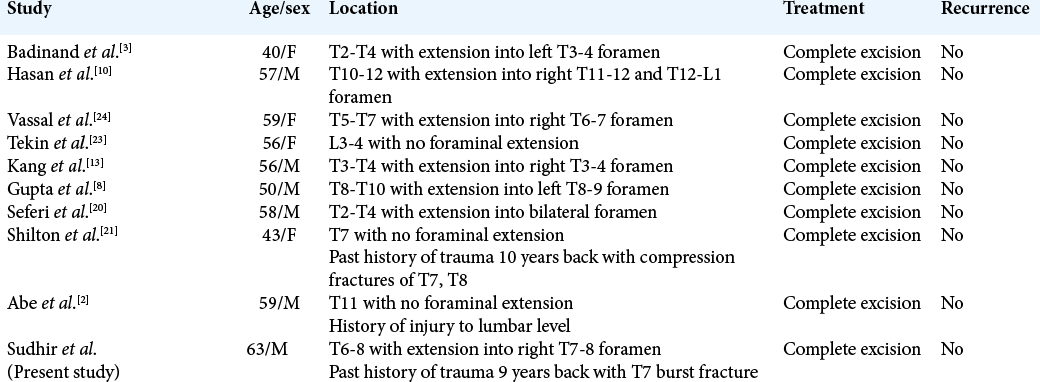
Background: Capillary hemangiomas are benign vascular lesions commonly seen in subcutaneous tissues. The most common site of origin is from the vertebral body, and only a few cases of isolated lesions in thoracic epidural space, especially after trauma, have been reported in the literature.
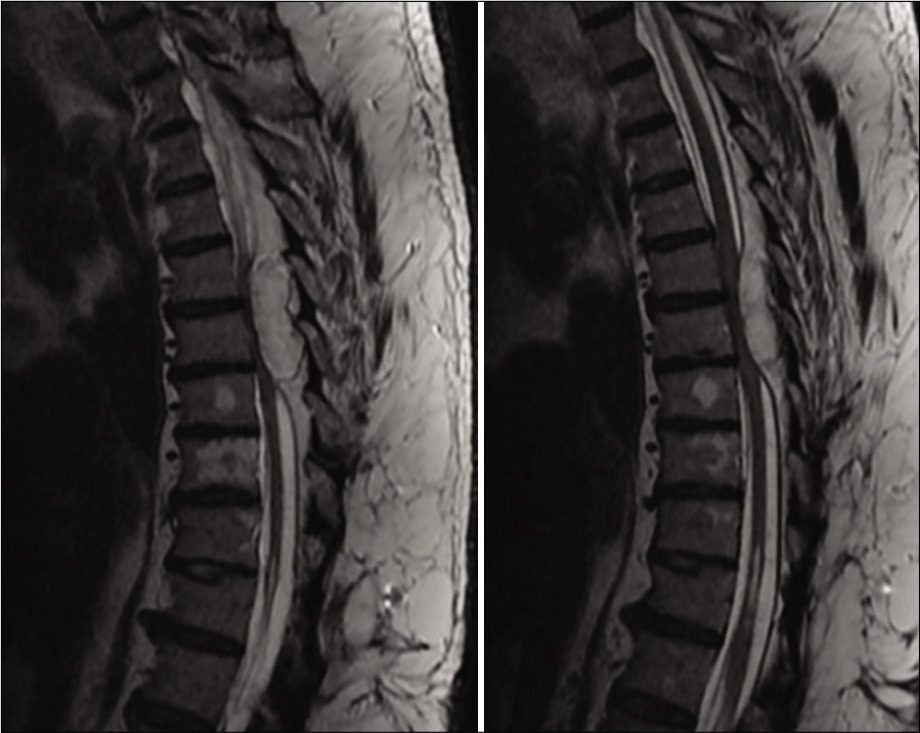
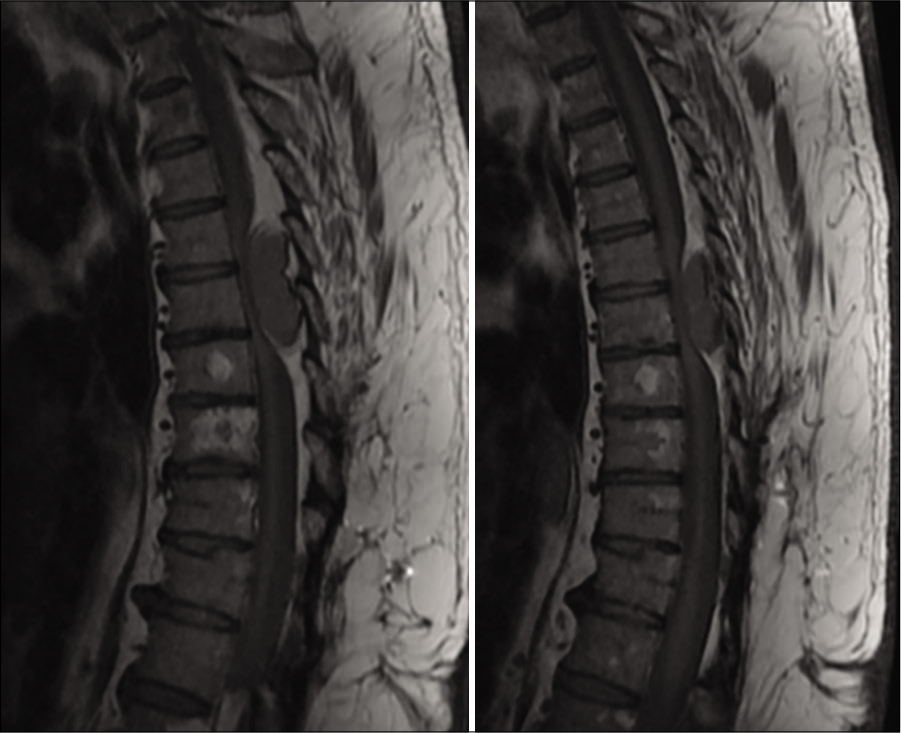
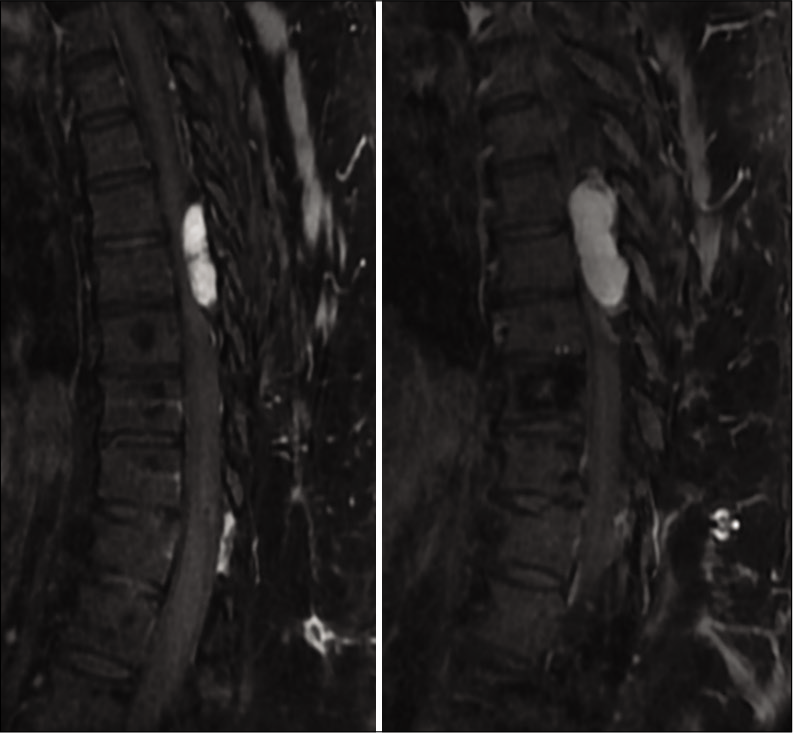
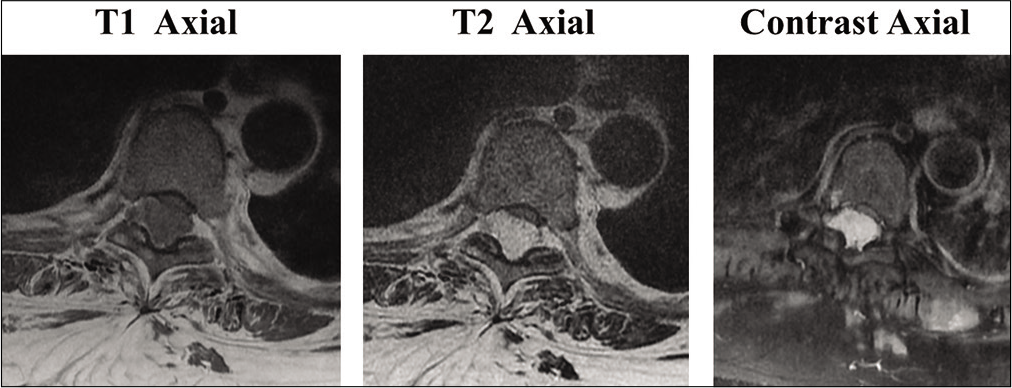
Case Description: We report a case of 63-year-old male with progressive bilateral lower limb weakness and exaggerated lower limb deep tendon reflexes without bowel and bladder involvement. His history revealed T7 fracture with paraparesis which was treated surgically, and implants were removed a year later. MRI showed an epidural lesion from T6-T8 extending into the right T7-8 foramen which showed hypointensity on T1, hyperintensity on T2, and homogenous enhancement in contrast images with severe cord compression. Laminectomy was done and the lesion was removed en bloc. Histopathological examination revealed it to be capillary hemangioma. The neurology came back to normal after 3 months.
Conclusion: Although capillary hemangiomas are rare lesions, it has to be considered in the differential diagnosis of epidural space-occupying lesions which require early surgical removal to prevent a progressive and permanent neurological deficit.
Keywords: Epidural capillary hemangioma, Posttraumatic, Thoracic hemangioma
INTRODUCTION
Capillary hemangiomas are benign tumors of endothelial cell origin arising most commonly from the soft tissues of head and neck.[
CASE DESCRIPTION
A 63-year-old South Asian male presented with pain over the upper and mid-back with progressive weakness of bilateral lower limbs for 2 months. The pain was insidious in onset and gradually progressive which aggravated on walking and relieved on rest. He had a history of T7 fracture with paraparesis 9 years back, for which he underwent posterior stabilization and instrumentation followed by a complete recovery of his neurological deficit and implant removal a year later. Neurological examination revealed spastic paraparesis with Grade 2 power (MRC grading) and exaggerated knee and ankle reflexes in both lower limbs. His bowel and bladder functions were normal. MRI showed an extradural lesion measuring 4.2 × 1.6 × 1.9 cm (CC × AP × Trans), which was mildly hypointense on T1- and hyperintense on T2-weighted images with strong relatively homogenous enhancement following contrast administration within the posterior aspect of the spinal canal at the T6-T8 vertebral level, causing severe compression and anterior displacement of the cord [
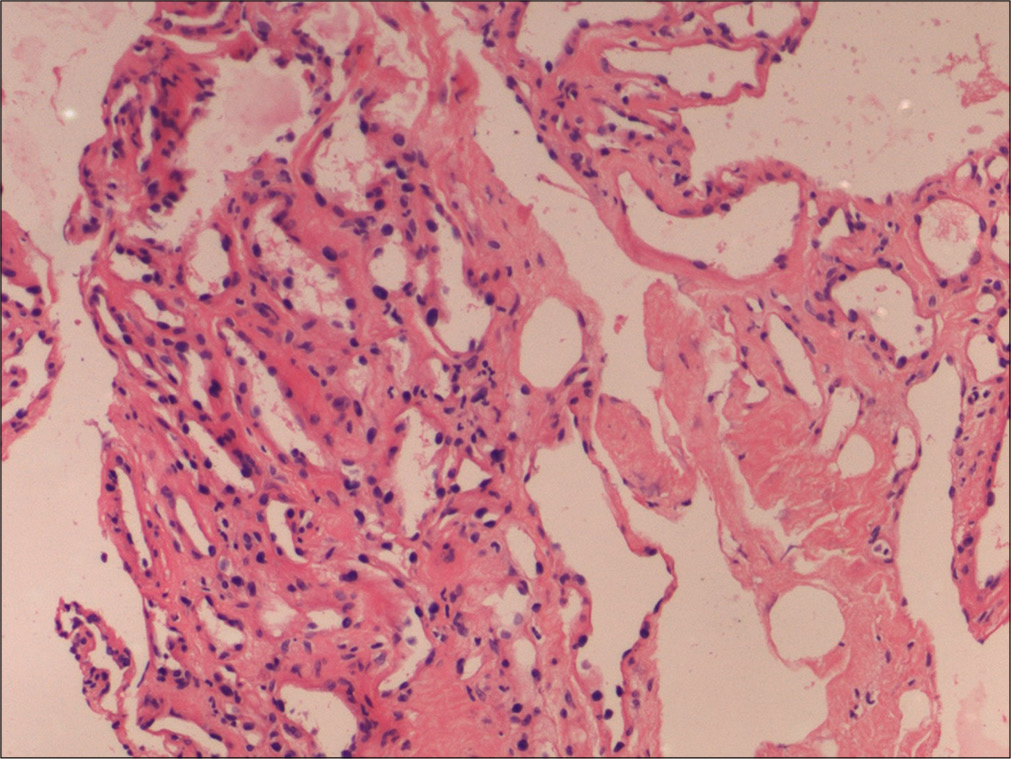
In view of neurological deficit, the patient underwent T6–T8 wide laminectomy and facetectomy. The lesion appeared as a well-circumscribed spongy, purple hemorrhagic epidural mass over the dura extending into the T7/T8 neural foramen, which was removed in toto by carefully detaching it from dura. Histopathology examination revealed a highly vascular tumor with innumerable thin-walled capillary vessels of varying sizes, lined by flattened endothelium, and embedded within a fibro-fatty tissue with a total lack of smooth muscular elements suggestive of capillary hemangioma [
Postoperative period was uneventful and the neurology improved significantly to Grade 4 within 2 weeks and to Grade 5 at the end of 3 months.
DISCUSSION
Capillary hemangiomas are benign vascular lesions commonly seen in the skin and subcutaneous tissues.[
Posttraumatic capillary hemangiomas, also known as pyogenic granulomas, have been reported in skin and mucous membranes.[
Although few authors have suggested a conservative approach considering the benign nature of these lesions,[
CONCLUSION
Epidural capillary hemangiomas are rare tumors that have to be differentiated from other vascular lesions of the spine. Although posttraumatic capillary hemangiomas are common in subcutaneous tissues, it is not uncommon for its occurrence in the spine. Early and prompt diagnosis by MRI and histopathological examination is vital. Surgical excision after one careful preoperative workup is the treatment of choice to prevent a progressive and permanent neurological deficit.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abdullah DC, Raghuram K, Phillips CD, Jane JA, Miller B. Thoracic intraduralextramedullary capillary hemangioma. AJNR Am J Neuroradiol. 2004. 25: 1294-6
2. Abe M, Tabuchi K, Tanaka S, Hodozuka A, Kunishio K, Kubo N. Capillary hemangioma of the central nervoussystem. J Neurosurg. 2004. 101: 73-81
3. Badinand B, Morel C, Kopp N, Tran Min VA, Cotton F. Dumbbell-shaped epidural capillary hemangioma. AJNR Am J Neuroradiol. 2003. 24: 190-2
4. Barr KL, Vincek V. Subcutaneous intravascular pyogenic granuloma: A case report and review of the literature. Cutis. 2010. 86: 130-2
5. Behne K, Robertson I, Weedon D. Disseminated lobular capillary haemangioma. Australas J Dermatol. 2002. 43: 297-300
6. Ben-Menachem Y, Epstein MJ. Post-traumatic capillary hemangioma of the hand. A case report. J Bone Joint Surg Am. 1974. 56: 1741-3
7. Feider HK, Yuille DL. An epidural cavernous hemangioma of the spine. AJNR Am J Neuroradiol. 1991. 12: 243-4
8. Gupta S, Kumar S, Banerji D, Pandey R, Gujral R. Magnetic resonance imaging features of an epidural spinal haemangioma. Australas Radiol. 1996. 40: 342-4
9. Hanakita J, Suwa H, Nagayasu S, Suzuki H. Capillary hemangioma in the caudaequina: Neuroradiological findings. Neuroradiology. 1991. 33: 458-61
10. Hasan A, Guiot MC, Torres C, Marcoux J. A case of a spinal epidural capillary hemangioma: Case report. Neurosurgery. 2011. 68: E850-3
11. Holtzman RN, Brisson PM, Pearl RE, Gruber ML. Lobular capillary hemangioma of the cauda equina. Case report. J Neurosurg. 1999. 90: 239-41
12. Kaneko Y, Yamabe K, Abe M. Rapid regrowth of a capillary hemangioma of the thoracic spinal cord. Neurol Med Chir (Tokyo). 2012. 52: 665-9
13. Kang JS, Lillehei KO, Kleinschmidt-Demasters BK. Proximal nerve root capillary hemangioma presenting as a lung mass with bandlike chest pain: Case report and review of literature. Surg Neurol. 2006. 65: 584-9
14. Kapadia SB, Heffner DK. Pitfalls in the histopathologic diagnosis of pyogenic granuloma. Eur Arch Otorhinolaryngol. 1992. 249: 195-200
15. Kasukurthi R, Ray WZ, Blackburn SL, Lusis EA, Santiago P. Intramedullary capillary hemangioma of the thoracic spine: Case report and review of the literature. Rare Tumors. 2009. 1: e10-
16. Kim KJ, Lee JY, Lee SH. Spinal intradural capillary hemangioma. Surg Neurol. 2006. 66: 212-4
17. Nowak DA, Gumprecht H, Stölzle A, Lumenta CB. Intraneural growth of a capillary haemangioma of the cauda equina. Acta Neurochir (Wien). 2000. 142: 463-7
18. Padolecchia R, Acerbi G, Puglioli M, Collavoli PL, Ravelli V, Caciagli P. Epidural spinal cavernous hemangioma. Spine (Phila Pa 1976). 1998. 23: 1136-40
19. Roncaroli F, Scheithauer BW, Krauss WE. Capillary hemangioma of the spinal cord. Report of four cases. J Neurosurg. 2000. 93: 148-51
20. Seferi A, Alimehmeti R, Vyshka G, Bushati T, Petrela M. Case study of a spinal epidural capillary hemangioma: A 4-year postoperative follow-up. Global Spine J. 2014. 4: 55-8
21. Shilton H, Goldschlager T, Kelman A, Xenos C. Delayed post-traumatic capillary haemangioma of the spine. J Clin Neurosci. 2011. 18: 1546-7
22. Shin JH, Lee HK, Jeon SR, Park SH. Spinal intradural capillary hemangioma: MR findings. AJNR Am J Neuroradiol. 2000. 21: 954-6
23. Tekin T, Bayrakli F, Simsek H, Colak A, Kutlay M, Demircan MN. Lumbar epidural capillary hemangioma presenting as lumbar disc herniation disease: Case report. Spine (Phila Pa 1976). 2008. 33: E795-7
24. Vassal F, Péoc’h M, Nuti C. Epidural capillary hemangioma of the thoracic spine with proximal nerve root involvement and extraforaminal extension. Acta Neurochir (Wien). 2011. 153: 2279-81