- Department of Neurological Surgery, Montefiore Medical Center/Albert Einstein School of Medicine, Bronx, New York, USA
- Department of Neurological Surgery, Rush University Medical Center, Chicago, Illinois, USA
- Department of Neurological Surgery, University of Texas Southwestern Medical Center, Dallas, Texas, USA
- Department of Neurosurgery, Duke University Medical Center, Durham, North Carolina, USA
- Department of Neurosurgery, Baylor College of Medicine Medical Center, Houston, Texas, USA
Correspondence Address:
Merritt D. Kinon
Department of Neurological Surgery, Montefiore Medical Center/Albert Einstein School of Medicine, Bronx, New York, USA
DOI:10.4103/2152-7806.192724
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kinon MD, Nasser R, Nakhla JP, Adogwa O, Moreno JR, Harowicz M, Verla T, Yassari R, Bagley CA. Predictive parameters for the antecedent development of hip pathology associated with long segment fusions to the pelvis for the treatment of adult spinal deformity. Surg Neurol Int 20-Oct-2016;7:93
How to cite this URL: Kinon MD, Nasser R, Nakhla JP, Adogwa O, Moreno JR, Harowicz M, Verla T, Yassari R, Bagley CA. Predictive parameters for the antecedent development of hip pathology associated with long segment fusions to the pelvis for the treatment of adult spinal deformity. Surg Neurol Int 20-Oct-2016;7:93. Available from: http://surgicalneurologyint.com/surgicalint_articles/predictive-parameters-antecedent-development-hip-pathology-associated-long-segment-fusions-pelvis-treatment-adult-spinal-deformity/
Abstract
Background:The surgical treatment of adult scoliosis frequently involves long segment fusions across the lumbosacral joints that redistribute tremendous amounts of force to the remaining mobile spinal segments as well as to the pelvis and hip joints. Whether or not these forces increase the risk of femoral bone pathology remains unknown. The aim of this study is to determine the correlation between long segment spinal fusions to the pelvis and the antecedent development of degenerative hip pathologies as well as what predictive patient characteristics, if any, correlate with their development.
Methods:A retrospective chart review of all long segment fusions to the pelvis for adult degenerative deformity operated on by the senior author at the Duke Spine Center from February 2008 to March 2014 was undertaken. Enrolment criteria included all available demographic, surgical, and clinical outcome data as well as pre and postoperative hip pathology assessment. All patients had prospectively collected outcome measures and a minimum 2-year follow-up. Multivariable logistic regression analysis was performed comparing the incidence of preoperative hip pain and antecedent postoperative hip pain as a function of age, gender, body mass index (BMI), and number of spinal levels fused.
Results:In total, 194 patients were enrolled in this study. Of those, 116 patients (60%) reported no hip pain prior to surgery. Eighty-three patients (71.6%) remained hip pain free, whereas 33 patients (28.5%) developed new postoperative hip pain. Age, gender, and BMI were not significant among those who went on to develop hip pain postoperatively (P P P P
Conclusion:This study demonstrates that long segment lumbosacral fusions are not associated with an increase in postoperative hip pathology. Age, gender, BMI, and levels fused do not correlate with the development of postoperative hip pain. The restoration of spinal alignment with long segment fusions may actually decrease the risk of developing femoral bone pathology and have a protective effect on the hip.
Keywords: Adult spine deformity, degenerative spine disease, hip pain, long segment fusion, lumbar spondylosis, pelvis, sacrum, sagittal balance, spinal alignment, spine fusion
INTRODUCTION
With advances in medicine, the US adult population is rapidly expanding, while staying more active.[
Treatment of adult degenerative spinal deformity often requires multilevel spinal decompression, with corrective osteotomies and arthrodesis to the sacrum and pelvis.[
MATERIALS AND METHODS
This study was based on a retrospective chart review of all patients who underwent long segment thoracolumbar fusion to the sacrum and pelvis performed by the senior author at the Duke Spine Center from February 2008 to March 2014. Prospectively collected demographic, surgical, and functional outcomes data as well as pre and postoperative hip pain assessment were recorded.
Institutional Review Board approval was obtained prior to study initiation. We included patients older than 18 years of age with either an idiopathic deformity or a degenerative spinal deformity with the primary complaint of back pain with associated neurogenic claudication or radiculopathy. Degree of deformity was assessed on standard scoliosis films by the senior author. Surgical corrective procedure as well as number of spinal levels fused was recorded. All patients had functional assessment data collected at the baseline and then post intervention at regular intervals, with most patients having greater than 1 year of follow up. Baseline hip pain assessment was gathered from the patients’ histories preoperatively as well as from patients’ history postoperatively or patients’ specific concern. Based on the degree and duration of hip discomfort, patients were then referred to Orthopedics for evaluation, and any available orthopedic recommendation or intervention, if available, was recorded.
All data were collected and analyzed in aggregate form. All parametric data were expressed as means ± standard deviation (SD). A multivariable logistic regression model was used to compare the incidence of preoperative hip pain and the antecedent development of postoperative hip pain as a function of age, gender, body mass index (BMI), and the number of spinal levels fused. Statistical significance was set at a P value less than 0.05.
RESULTS
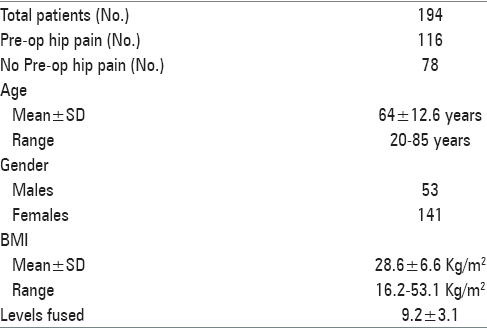
One hundred and ninety-four patients met the inclusion criteria for this study, with 141 female and 53 male patients [
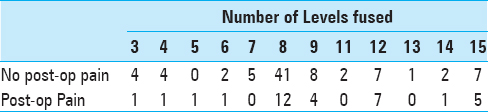
In the group of patients without hip pain prior to long segment thoracolumbar fusion to the sacrum or pelvis, 83 (70%) patients of the total 116 patients remained hip pain free after surgical intervention. Thirty-three (30%) patients went on to develop postoperative hip pain after deformity correction surgery with long segment fusion to the sacrum and pelvis. Age (P < 0.0651), gender (P < 0.3491), and BMI (P < 0.1021) did not have any statistically significant association with the development of hip pain after deformity correction in patients without preoperative hip pain.
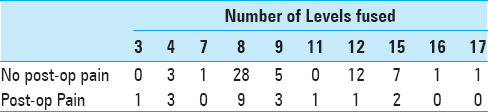
Of the 78 patients that complained of hip pain prior to surgery, 20 patients (26%) reported no change in their hip pain after long segment thoracolumbar fusion to the sacrum or pelvis. Fifty-eight patients reported improvement in their hip pain postoperatively, an approximate 74% reduction. Age (P < 0.4385), gender (P < 0.4637), and BMI (P < 0.2545) did not have any statistical significant correlation with the persistence of hip pain after deformity correction among patients with preoperative hip pain.
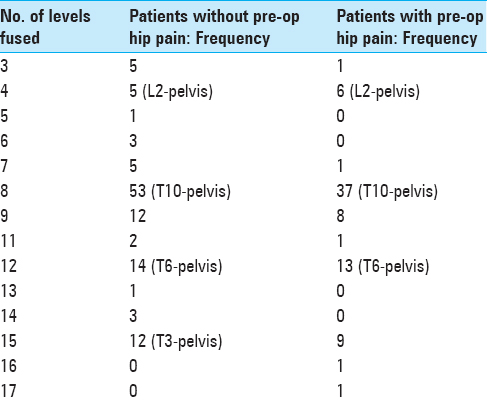
Long segment fusion was defined as a spinal fusion surgery involving at least 3 or more spinal levels. In the patient group who had no hip pain before surgery, there was an average of 9 (interquartile range) spinal levels fused for their deformity correction surgery, with a range of 3 spinal levels to a maximum of 15 levels. The most frequent number of levels fused in this study were 8, 9, 12, and 15 which correlated with T10-sacrum/pelvis, T9-sacrum/pelvis, T6-sacrum/pelvis, and T3-sacrum/pelvis, respectively. The corresponding frequencies were 45.7%, 10.3%, 12.1%, and 10.3%, respectively, [
DISCUSSION
The pelvis plays a pivotal role in maintaining global sagittal alignment. There is a harmonious and synergistic interplay between the spine and pelvis to maintain a healthy sagittal balance. Through compensatory mechanisms such as bending of the knees, uncovering the hip joint, and modulating the tilt of the pelvis can influence the spine by adjusting the lumbar lordosis.[
With an aging population, the prevalence of degenerative spondyloarthropathies increases.[
Out of the patients who were hip pain free prior to the deformity correction, nearly 70% remained hip pain free postoperatively. However, 30% developed hip pain postoperatively. Long segment spinal fusion creates significant stress and transfer significant forces that to the remaining mobile spinal segments and joints. These long fusion masses also alter the biomechanical environment and load sharing capability of the adjacent joints.[
Among patients with baseline hip pain, we found a 74% approximate rate of reduction in hip symptoms after deformity correction. This was most likely due to restoration of their sagittal alignment and putting these patients into a more energy efficient posture with less need for them to rely on compensatory posture by the pelvis and hip joints.[
We also investigated whether the amount of spinal levels fused caused an increased rate of the antecedent development of hip pathology. The most frequent amount of spinal levels fused were 8, 9, 12, and 15 which correlated to T10-, T9-, T6-, T3-sacrum/pelvis, respectively. These were the most frequent spinal fusions because these are biomechanically good spinal segments to end a fusion as they all avoid ending a long spinal fusion construct at either a transition point or apex of the thoracic or lumbar curves.[
It is valuable to consider the study's limitations to best utilize the knowledge gained from our analysis. Of note, this was a single institution retrospective analysis, which included 194 patients from a single surgeon. The inherent weakness with this study is the small sample size and a single surgeon's experience, which makes it difficult to generalize the conclusions of this study. In addition, the determination of hip pain or hip pathology was subjective and was gathered from the patient's corresponding medical record, rather than having the patients undergo a formal orthopedic evaluation prior to and after long segment fusion. It is difficult to objectively quantify the amount and degree of hip pathology the patients had in this study. Furthermore, it is difficult to define if their pain was truly from the hip joint rather than from other areas referred to the hip. Finally, our main focus of this study was to determine if the amount of transferred force from long segment fusion to the pelvis caused increased degeneration of the mobile hip joint rather than the degree of deformity and its relationship to hip pathology. It is well known that better spinal alignment puts patients into a more economical and comfortable posture. In addition to achieving spinal balance, the sacroiliac joint must not be neglected. In a study performed by Boachie-Adjei et al., sacroiliac degeneration occurred in 75% of patients undergoing long segment fusion to the sacrum.[
CONCLUSION
This study shows that long segment fusions to the sacrum and pelvis are not associated with an increase in postoperative hip pathology. Age, gender, BMI, and levels fused did not correlate with development of postoperative hip pain. The restoration of spinal alignment with long segment fusions may actually decrease the risk of developing femoral bone pathology and have a protective effect on the end hip joint.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bradford DS, Tay BK, Hu SS. Adult scoliosis: Surgical indications, operative management, complications, and outcomes. Spine. 1999. 24: 2617-29
2. Edwards CC, Bridwell KH, Patel A, Rinella AS, Jung Kim Y, Berra AB. Thoracolumbar deformity arthrodesis to L5 in adults: The fate of the L5-S1 disc. Spine. 2003. 28: 2122-31
3. Ekman P, Moller H, Shalabi A, Yu YX, Hedlund R. A prospective randomised study on the long-term effect of lumbar fusion on adjacent disc degeneration. Eur Spine J. 2009. 18: 1175-86
4. Emami A, Deviren V, Berven S, Smith JA, Hu SS, Bradford DS. Outcome and complications of long fusions to the sacrum in adult spine deformity: Luque-galveston, combined iliac and sacral screws, and sacral fixation. Spine. 2002. 27: 776-86
5. Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine. 2005. 30: 2024-9
6. Harvey J, Tanner S. Low back pain in young athletes. A practical approach. Sports Med. 1991. 12: 394-406
7. Heary RF, Albert TJ.editorsSpinal Deformities: The Essentials. New York, NY: Thieme Medical Publishers, Inc; 2007. p.
8. Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: The consequences of spinal fusion?. Spine J. 2004. 4: 190s-4
9. Horton WC, Holt RT, Muldowny DS. Controversy. Fusion of L5-S1 in adult scoliosis. Spine. 1996. 21: 2520-2
10. Islam NC, Wood KB, Transfeldt EE, Winter RB, Denis F, Lonstein JE. Extension of fusions to the pelvis in idiopathic scoliosis. Spine. 2001. 26: 166-73
11. Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: Prevalence and risk factor analysis of 144 cases. Spine. 2006. 31: 2329-36
12. Klineberg E, Schwab F, Smith JS, Gupta MC, Lafage V, Bess S. Sagittal spinal pelvic alignment. Neurosurg Clin N Am. 2013. 24: 157-62
13. Kuklo TR, Bridwell KH, Lewis SJ, Baldus C, Blanke K, Iffrig TM. Minimum 2-year analysis of sacropelvic fixation and L5-S1 fusion using S1 and iliac screws. Spine. 2001. 26: 1976-83
14. Lebwohl NH, Cunningham BW, Dmitriev A, Shimamoto N, Gooch L, Devlin V. Biomechanical comparison of lumbosacral fixation techniques in a calf spine model. Spine. 2002. 27: 2312-20
15. Lee CK, Langrana NA. Lumbosacral spinal fusion. A biomechanical study. Spine. 1984. 9: 574-81
16. Nagata H, Schendel MJ, Transfeldt EE, Lewis JL. The effects of immobilization of long segments of the spine on the adjacent and distal facet force and lumbosacral motion. Spine. 1993. 18: 2471-9
17. O’Lynnger TM, Zuckerman SL, Morone PJ, Dewan MC, Vasquez-Castellanos RA, Cheng JS. Trends for Spine Surgery for the Elderly: Implications for Access to Healthcare in North America. Neurosurgery. 2015. 77: S136-41
18. Offierski CM, MacNab I. Hip-spine syndrome. Spine. 1983. 8: 316-21
19. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: Review of the literature. Spine. 2004. 29: 1938-44
20. Quan GM, Wilde P. Fractured neck of femur below long spinopelvic fixation for Charcot spine: A case report. J Med Case Rep. 2013. 7: 277-
21. Quinnell RC, Stockdale HR. Some experimental observations of the influence of a single lumbar floating fusion on the remaining lumbar spine. Spine. 1981. 6: 263-7
22. Schlegel JD, Smith JA, Schleusener RL. Lumbar motion segment pathology adjacent to thoracolumbar, lumbar, and lumbosacral fusions. Spine. 1996. 21: 970-81
23. Schroeder JE, Cunningham ME, Ross T, Boachie-Adjei O. Early results of sacro-iliac joint fixation following long fusion to the sacrum in adult spine deformity. HSS J. 2014. 10: 30-5
24. Schwab F, Dubey A, Pagala M, Gamez L, Farcy JP. Adult scoliosis: A health assessment analysis by SF-36. Spine. 2003. 28: 602-6
25. Seo M, Choi D. Adjacent segment disease after fusion for cervical spondylosis; myth or reality?. Br J Neurosurg. 2008. 22: 195-9
26. Shono Y, Kaneda K, Abumi K, McAfee PC, Cunningham BW. Stability of posterior spinal instrumentation and its effects on adjacent motion segments in the lumbosacral spine. Spine. 1998. 23: 1550-8
27. Takemitsu Y, Harada Y, Iwahara T, Miyamoto M, Miyatake Y. Lumbar degenerative kyphosis. Clinical, radiological and epidemiological studies. Spine. 1988. 13: 1317-26
28. Tumialan LM, Mummaneni PV. Long-segment spinal fixation using pelvic screws. Neurosurgery. 2008. 63: 183-90
29. Vaz G, Roussouly P, Berthonnaud E, Dimnet J. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J. 2002. 11: 80-7
30. Yoshimoto H, Sato S, Masuda T, Kanno T, Shundo M, Hyakumachi T. Spinopelvic alignment in patients with osteoarthrosis of the hip: A radiographic comparison to patients with low back pain. Spine. 2005. 30: 1650-7
31. Zhu Q, Itshayek E, Jones CF, Schwab T, Larson CR, Lenke LG. Kinematic evaluation of one- and two-level Maverick lumbar total disc replacement caudal to a long thoracolumbar spinal fusion. Eur Spine J. 2012. 21: S599-611