- Department of Neurosurgery, Kesennuma City Hospital, Kesennuma, Miyagi, Japan,
- Department of Neurosurgery, Tohoku University, Sendai, Miyagi, Japan.
Correspondence Address:
Norio Narita
Department of Neurosurgery, Tohoku University, Sendai, Miyagi, Japan.
DOI:10.25259/SNI_774_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Masahito Katsuki1, Norio Narita1, Naoya Ishida1, Ohmi Watanabe1, Siqi Cai1, Dan Ozaki1, Yoshimichi Sato1, Yuya Kato1, Wenting Jia1, Taketo Nishizawa1, Ryuzaburo Kochi1, Kanako Sato1, Teiji Tominaga2. Preliminary development of a prediction model for daily stroke occurrences based on meteorological and calendar information using deep learning framework (Prediction One; Sony Network Communications Inc., Japan). 28-Jan-2021;12:31
How to cite this URL: Masahito Katsuki1, Norio Narita1, Naoya Ishida1, Ohmi Watanabe1, Siqi Cai1, Dan Ozaki1, Yoshimichi Sato1, Yuya Kato1, Wenting Jia1, Taketo Nishizawa1, Ryuzaburo Kochi1, Kanako Sato1, Teiji Tominaga2. Preliminary development of a prediction model for daily stroke occurrences based on meteorological and calendar information using deep learning framework (Prediction One; Sony Network Communications Inc., Japan). 28-Jan-2021;12:31. Available from: https://surgicalneurologyint.com/surgicalint-articles/10552/
Abstract
Background: Chronologically meteorological and calendar factors were risks of stroke occurrence. However, the prediction of stroke occurrences is difficult depending on only meteorological and calendar factors. We tried to make prediction models for stroke occurrences using deep learning (DL) software, Prediction One (Sony Network Communications Inc., Tokyo, Japan), with those variables.
Methods: We retrospectively investigated the daily stroke occurrences between 2017 and 2019. We used Prediction One software to make the prediction models for daily stroke occurrences (present or absent) using 221 chronologically meteorological and calendar factors. We made a prediction models from the 3-year dataset and evaluated their accuracies using the internal cross-validation. Areas under the curves (AUCs) of receiver operating characteristic curves were used as accuracies.
Results: The 371 cerebral infarction (CI), 184 intracerebral hemorrhage (ICH), and 53 subarachnoid hemorrhage patients were included in the study. The AUCs of the several DL-based prediction models for all stroke occurrences were 0.532–0.757. Those for CI were 0.600–0.782. Those for ICH were 0.714–0.988.
Conclusion: Our preliminary results suggested a probability of the DL-based prediction models for stroke occurrence only by meteorological and calendar factors. In the future, by synchronizing a variety of medical information among the electronic medical records and personal smartphones as well as integrating the physical activities or meteorological conditions in real time, the prediction of stroke occurrence could be performed with high accuracy, to save medical resources, to have patients care for themselves, and to perform efficient medicine.
Keywords: Artificial intelligence, Calendar factors, Deep learning, Meteorological factors, Stroke
INTRODUCTION
Meteorological factors were reported as the risks of stroke occurrence. In Japanese studies, it is reported that low ambient temperature and winter season are the risks for all stroke types,[
Furthermore, calendar factors are also related to stroke occurrence. Nakaguchi et al. reported that Japanese national holidays are related to ICH occurrence. They also reported that, during RokuYo (traditional Japanese day of the week), the relative risk of ICH is extremely low on the traditionally unlucky days of ButsuMetsu and TomoBiki.[
Furthermore, some studies focused on the chronological changes of the meteorological factors, because physical responses to environmental changes may be delayed. Short-term change of ambient temperature is related to stroke.[
These studies suggested that meteorological conditions on the onset day as well as chronological changes in the former days may play important roles for the stroke occurrence. However, the prediction of the stroke occurrence is still difficult because the meteorological conditions and patients’ backgrounds vary from region to region.
Recently, artificial intelligence (AI) is attracting. Especially, it is a transitional period regarding AI from machine learning to deep learning (DL). DL applications use a layered structure of algorithms called an artificial neural network (ANN). The design of ANN is inspired by the biological neural network of the human brain, leading to a process of learning that’s far more capable than that of standard machine learning models.[
MATERIALS AND METHODS
Study population
We retrospectively investigated the daily stroke occurrence between January 2017 and December 2019 from the Kesennuma City Hospital’s medical records. The occurrence date was defined as the time when the ambulance or patients arrived at our hospital. Stroke subtypes include CI, hypertensive ICH, and aneurysmal subarachnoid hemorrhage. CI includes cardioembolic infarction, atherothrombotic infarction, lacunar infarction, or others according to the Trial of Org 10172 in Acute Stroke Treatment (TOAST) criteria.[
Study area
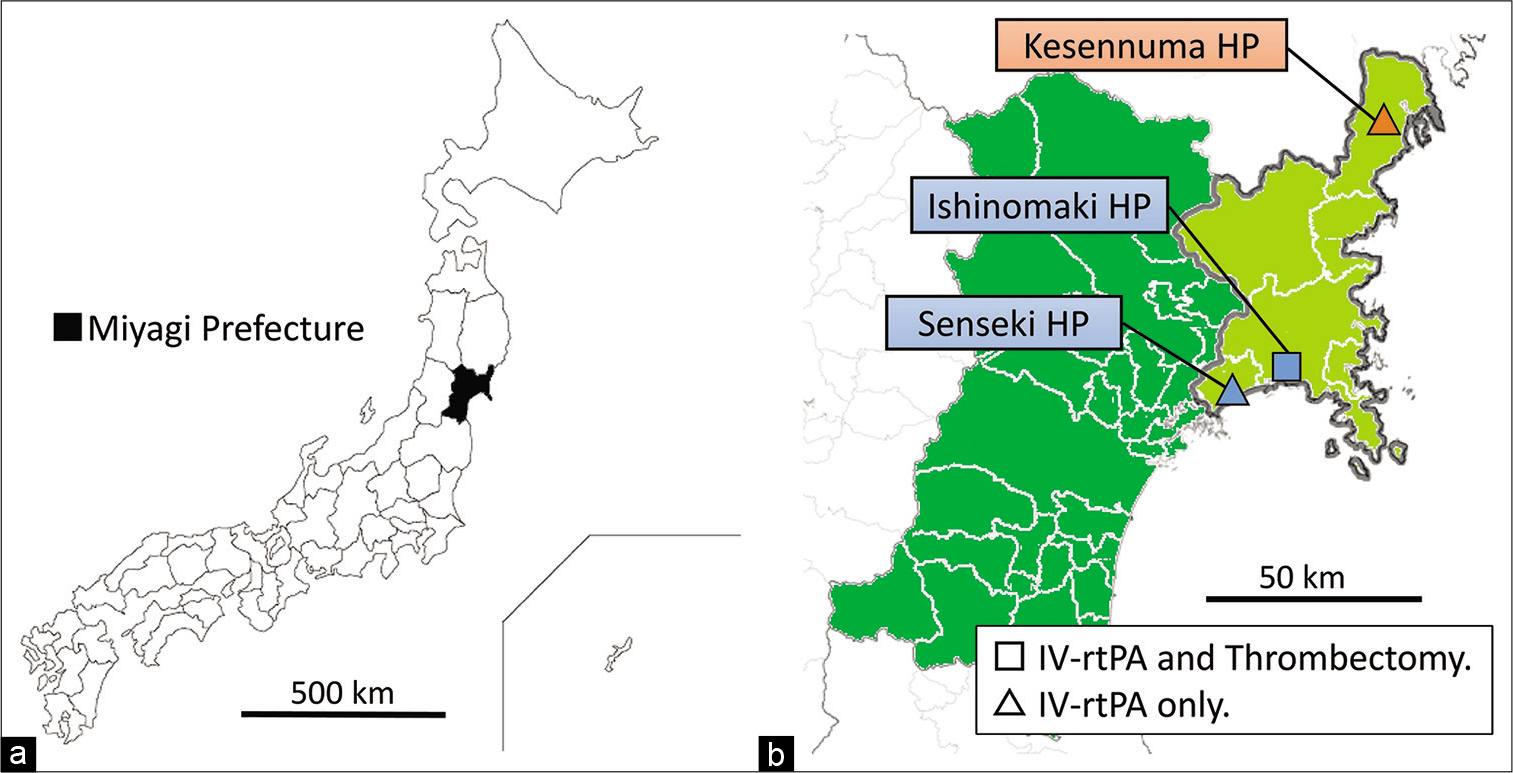
Japan is located in a temperate climate zone with four distinct seasons: spring, summer, autumn, and winter. Miyagi prefecture, where Kesennuma City Hospital[
Figure 1:
(a) Miyagi prefecture is located in the northeastern part of Japan. (b) Map of Miyagi prefecture. The Ishinomaki, Tome, and Kesennuma medical area, with background populations of about 350,000 people, is inside the thick line and colored with light green. The blue square is Japanese Red Cross Ishinomaki Hospital (HP), where both intravenous (IV) rt-PA and thrombectomy capable in this medical area. The blue triangle (Senseki HP) and the red triangle (Kesennuma City HP, where this study was performed) are IV rt-PA capable hospitals.
Meteorological data
Meteorological data in this study included daily mean ambient temperature (Tmean, °C), daily highest ambient temperature (Tmax, ghes daily lowest ambient temperature (Tmin, atu daily difference between the highest and lowest ambient temperature (Tmax-min, °C), daily mean AP (Pa, hPa), daily mean vapor pressure (hPa), mean wind speed (m/s), daily amount of the rainfall (mm) or snowfall (mm), sunlight hours (h), and daily mean relative humidity (RH, %) of the 24 h calendar day period (0:00 AM–11:59 PM) on the onset day and the past 7 days, which were obtained from the local meteorological observatories (Japan Meteorological Agency, Ministry of Land, Infrastructure, Transport and Tourism). The THI (°C) was calculated using the formula; THI = Tmean – 0.55 × (1 – 0.01 × RH) × (Tmean – 14.5) as reported previously.[
Calendrical variables
We also investigated the various calendrical variables over the study period, including date, day of the week, national holidays, and RokuYo. According to RokuYo, each day is classified as 1 of 6 days in a recurring 6-day calendrical series consisting of SenSho, TomoBiki, SenBu, ButsuMetsu, TaiAn, and ShakKo. ButsuMetsu is believed to be an unlucky day, when weddings and special events are avoided, and many crematories in Japan are closed on TomoBiki. Conversely, the other days of RokuYo, especially TaiAn, are believed to be lucky days, and events or ceremonies are generally scheduled for these days.
Making prediction model by Prediction One
We used Prediction One software to make the prediction models for daily stroke occurrence using 221 variables described above. Prediction One read the 3-year dataset and automatically divided them into almost a half as internal training and cross-validation datasets. Prediction One automatically adjusted and optimized the variables in a way that is easy to process statistically and mathematically, and select appropriate algorithm with ensemble learning. Prediction One made the best prediction model by ANN with internal cross-validation. The details are trade secrets and could not be provided.
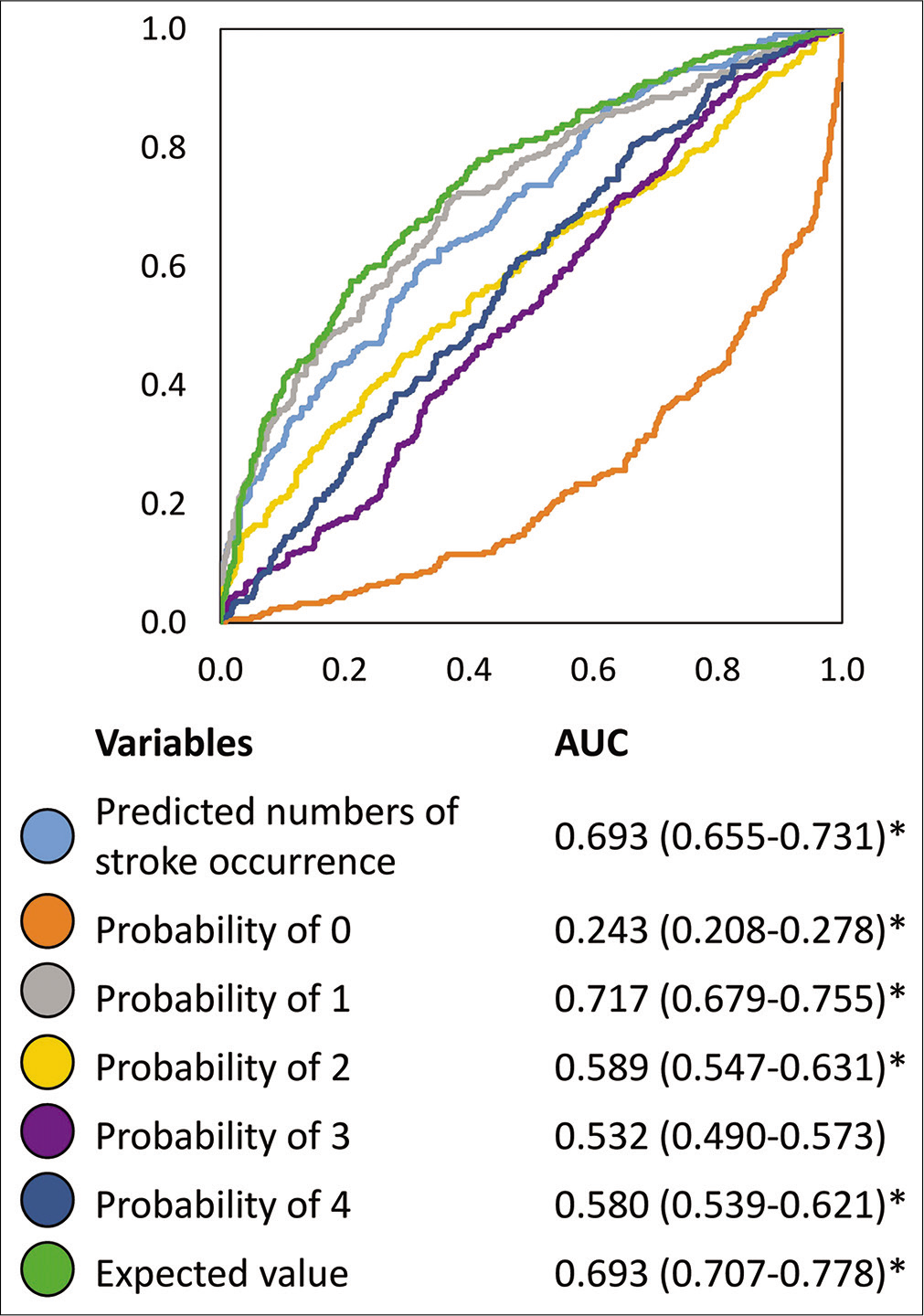
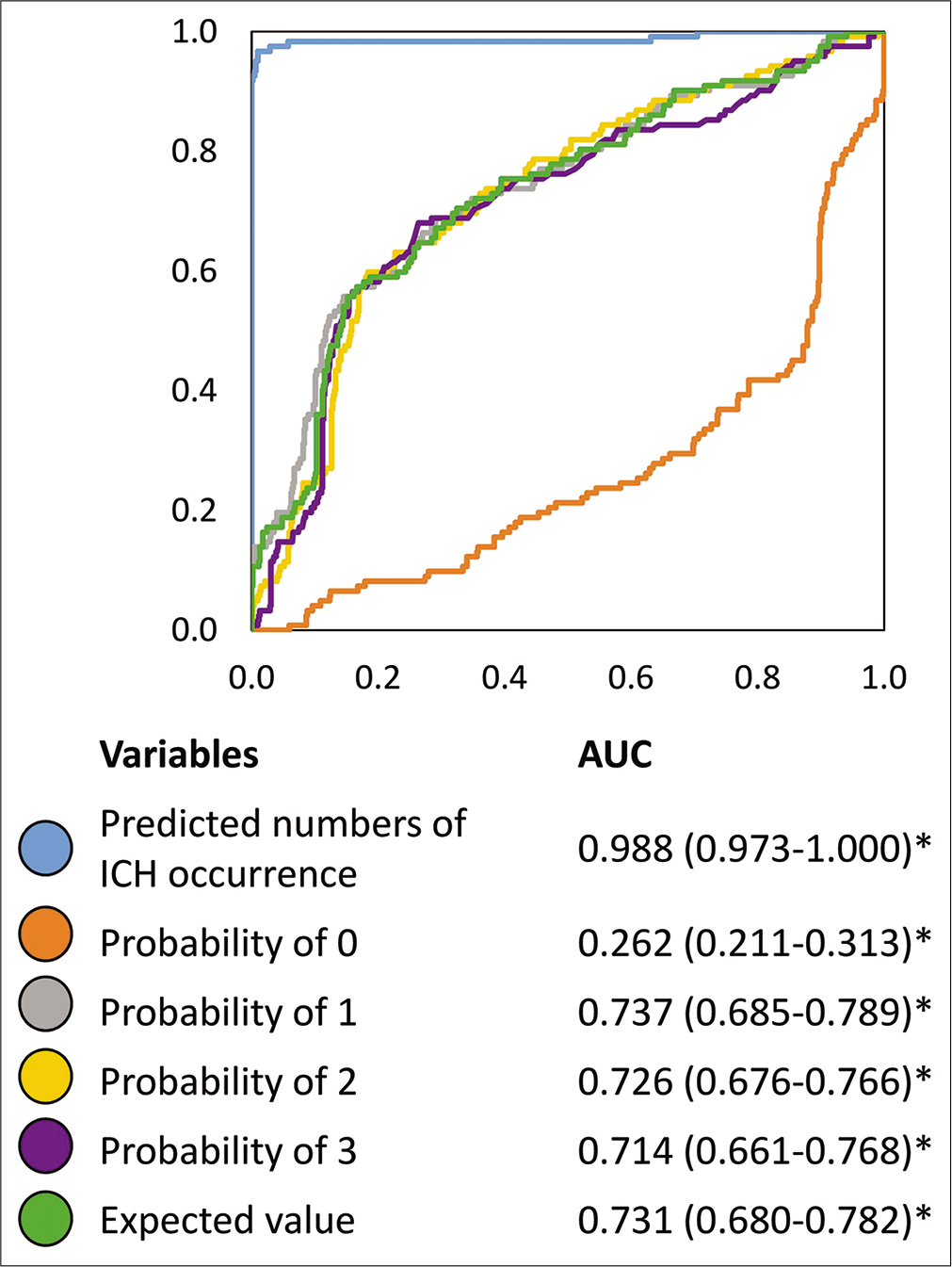
We made three prediction models; one for all daily stroke occurrences (just present or absent), one for daily CI occurrences, and the other for daily ICH occurrences. Each model made by Prediction One exported predicted numbers of the daily stroke occurrences, each probability of the number of the daily occurrences from 0 to 4, and the expected values from the probabilities. We then use these values as predictive markers for the stroke, CI, or ICH occurrences binomially (present or not). The area under the curves (AUC) of the receiver operating characteristic curve (ROC) of each value was statistically calculated, and we evaluated the models’ accuracy.
Statistical analysis
Results are shown as median (interquartile range). AUC of ROC was calculated using SPSS software version 24.0.0. (IBM, New York, USA). A two-tailed P < 0.05 was considered statistically significant.
RESULTS
Clinical characteristics
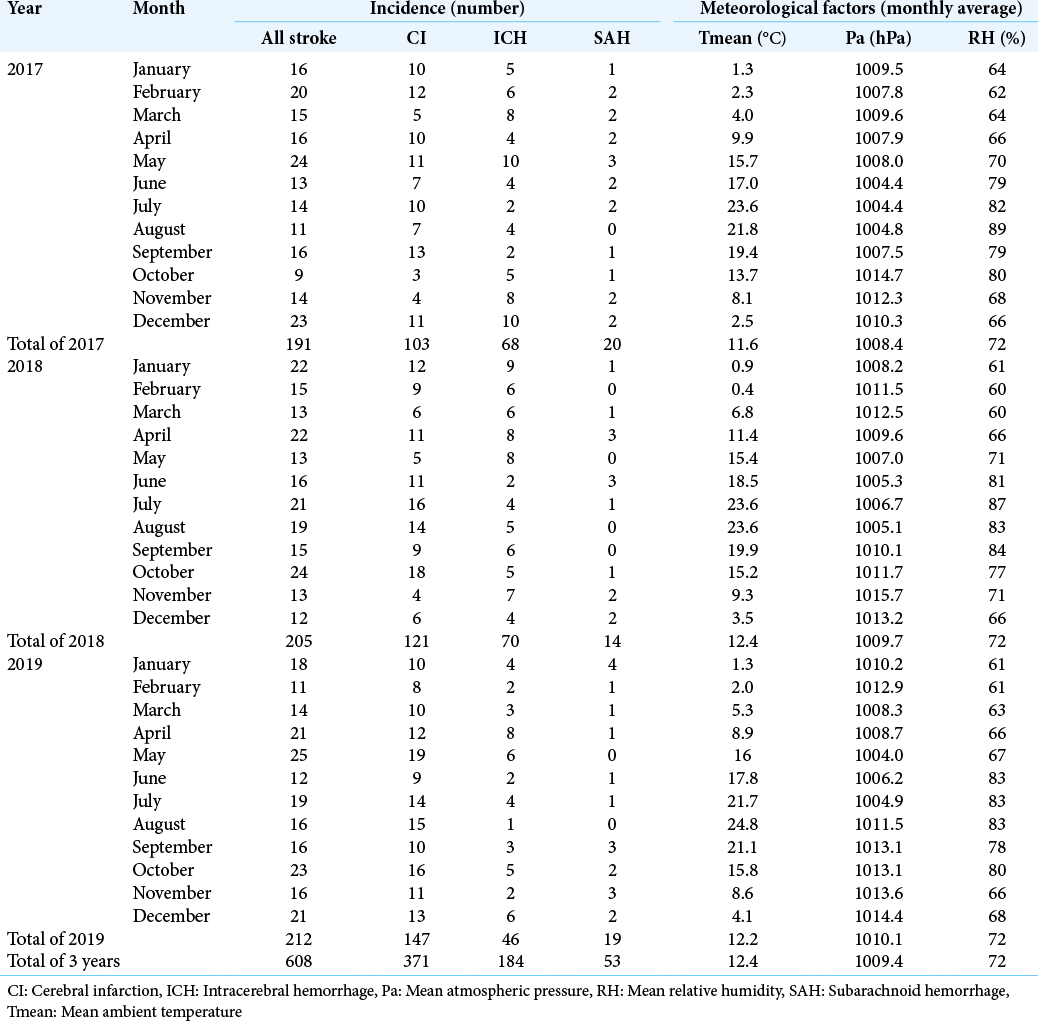
The monthly incidence of the 608 stroke patients (371 CI, 184 ICH, and 53 SAH) and monthly meteorological factors are summarized in [
Model development for all stroke, CI, and ICH occurrence
Prediction One produced each prediction model and value in <5 min. Against the stroke occurrence (present or not), the AUCs of predicted numbers of stroke occurrences, probability of each number of stroke patients as 0, 1, 2, 3, and 4, and the expected value were 0.693, 0.243, 0.717, 0.589, 0.532, 0.580, and 0.693, respectively [
DISCUSSION
We made preliminarily prediction models of daily stroke, CI, and ICH occurrences (present or not) using DL software, Prediction One, with 221 meteorological and calendar variables. This is the first report on making DL-based prediction models for the daily stroke occurrence only from the meteorological and calendar variables.
The need for prediction of stroke occurrence
The previous studies on the association between meteorological or calendar data and stroke occurrence were statistically performed, and the meteorological or calendar risk factors for stroke occurrence were already revealed. However, accurate prediction of the stroke occurrence is still difficult, so stroke neurologists and comedicals must be on the alert at all times. In Japan, 7500 neurosurgeons work according to the 2018 statistics.[
Future outlook
Simple DL software is being developed, so we should have an active interest in using it for the benefit of medical staff and patients. Our study did not produce a good prediction model from the meteorological and calendar data and was just one example. However, we suggested the potential of DL software. DL-based efficient medicine, depending on each patient and hospital, would be performed as DL software becomes more popular. Nowadays, smartphone apps or smartwatches[
Limitations of DL
We need to examine the clinical usefulness of the prediction models prospectively. For example, by predicting the stroke occurrence, we would evaluate the reduction of the workload and stress of the medical staff, and examine whether the medical resources and costs could be saved or not. Furthermore, we could examine the changes of the patients’ activities after showing the result of DL-based stroke prediction, similar to carrying an umbrella or not according to the information from the weather forecasts.
We used Prediction One software, but there are many AI softwares (frameworks) worldwide, and there are a thousand different ways to assemble the ANN (libraries). Prediction One is suitable for predicting binomial, ordinal, or continuous variables and can treat Japanese sentences themselves. Furthermore, when there are missing values, it automatically compensates. However, the details of how the ANN is assembled and tuned have not been released, so we need to think carefully about the accuracy of the models. Furthermore, Prediction One suggested important variables like “the difference of Tmax between day 5 and day 2,” but we should investigate why the variables were judged as important, considering the clinical meaning. Furthermore, we tried to predict the “numbers” of stroke occurrences, and the F-values of the models, which are an indicator of the AI-based model accuracy, were ranging from 0.745 to 0.912. They seemed good, but the predicted values were all 0. This is because the actual predicted numbers of the patients were ranging from 0.061 to 0.689, and the cutoff value was above those. In other words, DL, in this study, could not predict the actual numbers of strokes. Therefore, we separately calculate the AUCs using each exported values in this study.
Limitation of this study
First, we used the data from only 3 years, so further studies using that from the previous years or various regions should be performed. Second, some of the patients lived alone and were found by someone sometime after the stroke onset, and others of them came to our hospital a few days after conservation by themselves, so the models actually predicted the number of “visits” to the hospital, but not the occurrences. Third, the meteorological data are based on the 24 h calendar day period (0:00 AM–11:59 PM), but the work at the hospital begins at approximately 9:00 AM, and it should be the start line. Due to these reasons, the accurate hourly prediction would be further difficult compared to the daily one. Fourth, we should try to perform external validation.
CONCLUSION
We preliminarily made prediction models of daily stroke, CI, and ICH occurrences (present or not) using DL software, Prediction One, with meteorological and calendar variables. This is the first report on making DL-based prediction models for the daily stroke occurrences only from the meteorological and calendar variables. In the future, by synchronizing a wide variety of medical information among the electronic medical records, personal smartphones, and smartwatches as well as integrating the physical activities or meteorological conditions in real time, the prediction of stroke occurrence could be performed with much higher accuracy, to save the medical resources, to have patients care for themselves, and to perform efficient medicine.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Azimi P, Mohammadi HR, Benzel EC, Shahzadi S, Azhari S. Use of artificial neural networks to decision making in patients with lumbar spinal canal stenosis. J Neurosurg Sci. 2017. 61: 603-11
2. Fujita T, Ohashi T, Yamane K, Yamamoto Y, Sone T, Ohira Y. Relationship between the number of samples and the accuracy of the prediction model for dressing independence using artificial neural networks in stroke patients. Jpn J Compr Rehabil Sci. 2020. 11: 28-34
3. Fukuma R, Yanagisawa T, Kinoshita M, Shinozaki T, Arita H, Kawaguchi A. Prediction of IDH and TERT promoter mutations in low-grade glioma from magnetic resonance images using a convolutional neural network. Sci Rep. 2019. 9: 20311
4. Fuse N, Sakurai-Yageta M, Katsuoka F, Danjoh I, Shimizu R, Tamiya G. Establishment of integrated biobank for precision medicine and personalized healthcare: The Tohoku medical megabank project. JMA J. 2019. 2: 113-22
5. Goggins WB, Woo J, Ho S, Chan EY, Chau PH. Weather, season, and daily stroke admissions in Hong Kong. Int J Biometeorol. 2012. 56: 865-72
6. Hong YC, Rha JH, Lee JT, Ha EH, Kwon HJ, Kim H. Ischemic stroke associated with decrease in temperature. Epidemiology. 2003. 14: 473-8
7. Hui L, Ruan Y, Liang R, Liu X, Fan Z. Short-term effect of ambient temperature and the risk of stroke: A systematic review and meta-analysis. Int J Environ Res Public Health. 2015. 12: 9068-88
8. Ido K, Nakamura N, Nakayama M. Miyagi medical and welfare information network: A backup system for patient clinical information after the great east Japan earthquake and tsunami. Tohoku J Exp Med. 2019. 248: 19-25
9. Bin IS, Gyu Y, Lee KS, Bae HG, Byun BJ. Relationship between spontaneous cerebral hemorrhage and climatic factor. J Korean Neurosurg Soc. 1996. 25: 1786-93
10. Jimenez-Conde J, Ois A, Gomis M, Rodriguez-Campello A, Cuadrado-Godia E, Subirana I. Weather as a trigger of stroke: Daily meteorological factors and incidence of stroke subtypes. Cerebrovasc Dis. 2008. 26: 348-54
11. Katsuki M, Kakizawa Y, Nishikawa A, Yamamoto Y, Uchiyama T. Easily created prediction model using deep learning software (Prediction One, Sony Network Communications Inc.) for subarachnoid hemorrhage outcomes from small dataset at admission. Surg Neurol Int. 2020. 11: 374
12. Kokubo Y. Epidemiology of transient ischemic attack. Front Neurol Neurosci. 2014. 33: 69-81
13. Kumar R, Gupta A, Arora HS, Pandian GN, Raman B. CGHF: A computational decision support system for glioma classification using hybrid radiomics-and stationary wavelet-based features. IEEE Access. 2020. 8: 79440-58
14. Mukai T, Hosomi N, Tsunematsu M, Sueda Y, Shimoe Y, Ohshita T. Various meteorological conditions exhibit both immediate and delayed influences on the risk of stroke events: The HEWS-stroke study. PLoS One. 2017. 12: e0178223
15. Myint PK, Vowler SL, Woodhouse PR, Redmayne O, Fulcher RA. Winter excess in hospital admissions, in-patient mortality and length of acute hospital stay in stroke: A hospital database study over six seasonal years in Norfolk, UK. Neuroepidemiology. 2007. 28: 79-85
16. Nakaguchi H, Matsuno A, Teraoka A. Prediction of the incidence of spontaneous intracerebral hemorrhage from meteorological data. Int J Biometeorol. 2008. 52: 323-9
17. Nakaguchi H, Teraoka A. Relationship between the occurrence of spontaneous intracerebral hemorrhage and holidays and traditionally unlucky days in Fukuyama city, Hiroshima prefecture, Japan. J Stroke Cerebrovasc Dis. 2007. 16: 194-8
18. Ogata T, Kimura K, Minematsu K, Kazui S, Yamaguchi T. Variation in ischemic stroke frequency in Japan by season and by other variables. J Neurol Sci. 2004. 225: 85-9
19. Adams HP, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL. Classification of subtype of acute ischemic stroke, Definitions for use in a multicenter clinical trial, TOAST, Trial of org 10172 in acute stroke treatment. Stroke. 1993. 24: 35-41
20. Peel MC, Finlayson BL, McMahon TA. Updated world map of the Köppen-Geiger climate classification. Hydrol Earth Syst Sci. 2007. 11: 1633-44
21. Shibahara I, Osawa SI, Kon H, Morita T, Nakasato N, Tominaga T. Increase in the number of patients with seizures following the Great East-Japan earthquake. Epilepsia. 2013. 54: e49-52
22. Shibahara S. The 2011 Tohoku earthquake and devastating tsunami. Tohoku J Exp Med. 2011. 223: 305-7
23. Shinkawa A, Ueda K, Hasuo Y, Kiyohara Y, Fujishima M. Seasonal variation in stroke incidence in Hisayama, Japan. Stroke. 1990. 21: 1262-7
24. Sueda Y, Hosomi N, Tsunematsu M, Takamatsu K, Nomura E, Torii T. Effects of meteorological conditions on the risk of ischemic stroke events in patients treated with alteplase-HEWS-tPA. J Stroke Cerebrovasc Dis. 2015. 24: 1500-5
25. Takizawa S, Shibata T, Takagi S, Kobayashi S. Seasonal variation of stroke incidence in Japan for 3563.1 stroke patients in the Japanese standard stroke registry, 1998-2007. J Stroke Cerebrovasc Dis. 2013. 22: 3-41
26. Turin TC, Kita Y, Murakami Y, Rumana N, Sugihara H, Morita Y. Higher stroke incidence in the spring season regardless of conventional risk factors: Takashima stroke registry, Japan, 1988-2001. Stroke. 2008. 39: 745-52
27. Wang H, Sekine M, Chen X, Kagamimori S. A study of weekly and seasonal variation of stroke onset. Int J Biometeorol. 2002. 47: 13-20
28. Wang Q, Gao C, Wang H, Lang L, Yue T, Lin H. Ischemic stroke hospital admission associated with ambient temperature in Jinan, China. PLoS One. 2013. 8: e80381
29. Wang Y, Levi CR, Attia JR, D’Este CA, Spratt N, Fisher J. Seasonal variation in stroke in the Hunter region, Australia: A 5-year hospital-based study, 1995-2000. Stroke. 2003. 34: 1144-50
30. Watari MOzawa K. Ministry of Health, Labour and Welfare, Statistical Data on Medical Doctors, Dentists, and Pharmacologists in 2018. Available from: https://www.mhlw.go.jp/toukei/saikin/hw/ishi/18/dl/gaikyo.pdf [Last accessed on 2020 Sep 28].
31. Yamamoto K, Takahashi T, Urasaki M, Nagayasu Y, Shimamoto T, Tateyama Y. Health observation app for COVID-19 symptom tracking integrated with personal health records: Proof of concept and practical use study. JMIR mHealth uHealth. 2020. 8: e19902