- Department of Orthopedics, Institute of Orthopedics “Carlos E. Ottolenghi,” Hospital Italiano de Buenos Aires, Buenos Aires, Argentina,
- School of Medicine, University of California Irvine,
- Department of Orthopaedics, University of California Irvine, Orange, California, United States,
- Department of Neurosurgery, University of California Irvine, Orange, California, United States,
- Department of Neurological Surgery, Children’s Hospital La Plata, La Plata, Argentina.
Correspondence Address:
Gaston Camino-Willhuber , Institute of Orthopedics “Carlos E. Ottolenghi,” Hospital Italiano de Buenos Aires, Buenos Aires, Argentina.
DOI:10.25259/SNI_330_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Gaston Camino-Willhuber1, Austin Franklin2, Katherine Rosecrance2, Sarah Oyadomari2, Justin Chan3, Fernando Holc1, Sohaib Hashmi3, Michael Oh4, Nitin Bhatia3, Juan Emmerich5, Yu-Po Lee3. Preoperative hypoalbuminemia and dialysis increase morbidity/mortality after spine surgery for primary pyogenic spinal infections (ACS-NSQIP Study). 06-May-2022;13:193
How to cite this URL: Gaston Camino-Willhuber1, Austin Franklin2, Katherine Rosecrance2, Sarah Oyadomari2, Justin Chan3, Fernando Holc1, Sohaib Hashmi3, Michael Oh4, Nitin Bhatia3, Juan Emmerich5, Yu-Po Lee3. Preoperative hypoalbuminemia and dialysis increase morbidity/mortality after spine surgery for primary pyogenic spinal infections (ACS-NSQIP Study). 06-May-2022;13:193. Available from: https://surgicalneurologyint.com/surgicalint-articles/11579/
Abstract
Background: We analyzed the role of hypoalbuminemia, dialysis, and other risk factors that increase morbidity/ mortality following surgery for primary pyogenic spinal infections (PSIs). The American College of Surgeons’ National Surgical Quality Improvement Program (ACS-NSQIP) that included 627 patients was utilized as our database.
Methods: Primary spinal surgery for spondylodiscitis was evaluated in a ACS-NSQIP database involving 627 patients between 2010 and 2019. Outcome assessment included evaluation of 30-day postoperative morbidity, and mortality rates.
Results: Within 30 postoperative days, complications occurred in 14.6% (92/627) of patients; 59 (9.4%) required readmission, and 39 (6.2%) required additional surgery. The most common complications were: wound infections, pneumonia, septic shock, and death (1.8%). Hypoalbuminemia (i.e., significantly associated with unplanned readmission and reoperation), and dialysis were the two major risk factors contributing to increased perioperative morbidity and mortality.
Conclusion: Among 627 ACS-NSQIP patients undergoing primary surgery for PSIs, hypoalbuminemia and dialysis were associated with higher risks of major perioperative morbidity (i.e., within 30 postoperative days – mostly readmissions and reoperations) and mortality.
Keywords: Dialysis, Hypoalbuminemia, Readmission, Reoperation, Spondylodiscitis
INTRODUCTION
Pyogenic spinal infections (PSI) occur in between 0.5 and 2.4/100,000 patient/year.[
MATERIALS AND METHODS
Study design and criteria
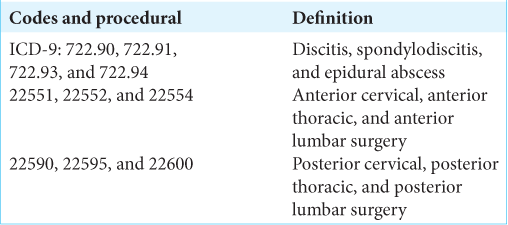
Institutional Review Board exemption was obtained from our institution. We utilized the American College of Surgeons’ National Surgical Quality Improvement Program (ACS-NSQIP) database looking at 627 patients undergoing primary spine surgery for spondylodiscitis between 2010 and 2019. We looked at a variety of demographics including comorbidities (i.e., diabetes, hypertension, chronic obstructive pulmonary disease (COPD), congestive heart failure, smoking, chronic steroid use, and dialysis), and 30-day outcomes (i.e., postoperative morbidity and mortality rates using major vs. minor Glassman classification) based on Classification of Diseases 9th and 10th codes and Current Procedural Terminology (CPT) codes [
Surgical data
Spine operations were defined as cervical if performed between C0 and C7-T1, thoracic if from T1 to T12-L1, and lumbar if from L1 to the sacrum. Primary outcomes were assessed at 30 postoperative days and included; the evaluation of; 1) major complication rates, 2) wound-complications, 3) mortality rates, 4) unplanned readmissions, 5) reoperations, 6) operative times, and 7) fusion rates.
Preoperative laboratory studies
Preoperative laboratory data included albumin levels, with hypoalbuminemia being defined as <3.5 g/dl.
Statistical analysis
Outcomes were analyzed utilizing univariate analysis based on the demographics, preoperative comorbidities, and other surgical variables. Comparisons were performed using Chi-square tests, Fisher’s exact test, or Student’s t-tests.
RESULTS
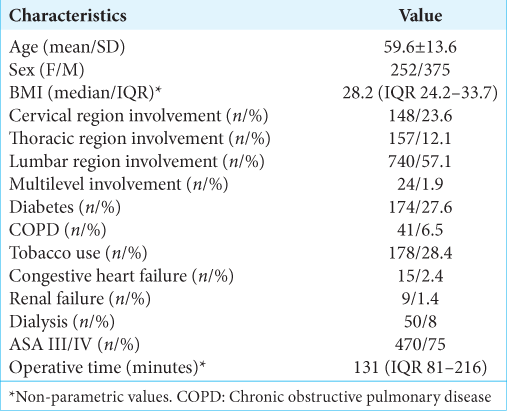
The most common comorbidities for 627 patients from the NSQIP database undergoing predominant lumbar followed by cervical spinal surgery included diabetes (27.6%) and COPD (6.5%: smokers 28.4%); [
Minor and major postoperative complications
A total of 71 (11.3%) patients sustained 92 complications within 30 postoperative days; 28 (30.4%) were minor, and 64 (69.5%) were major. The most common complications in descending order were wound infections (n = 23 [3.7%] largely attributed to hypoalbuminemia), pneumonia (n = 20), septic shock (n = 13), cardiac arrest (n = 11), mortality (n-11 (1.7%): highly correlated with dialysis), deep vein thrombosis (n = 10), and urinary tract infection (n = 5) [
Unplanned readmissions
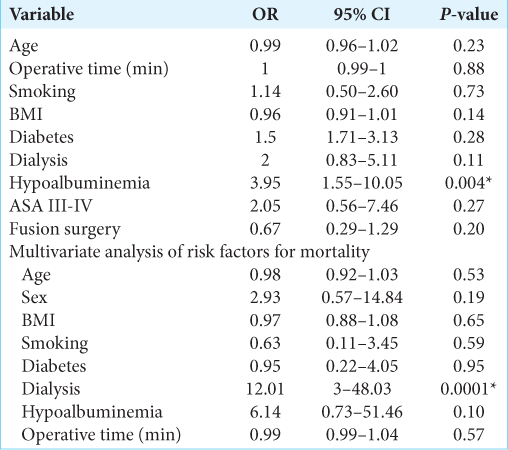
Various factors were associated with readmissions observed in 59 patients (9.4%) within 30 postoperative days. These included hypoalbuminemia, dialysis, smoking, and an ASA of III-IV [
Unplanned reoperations
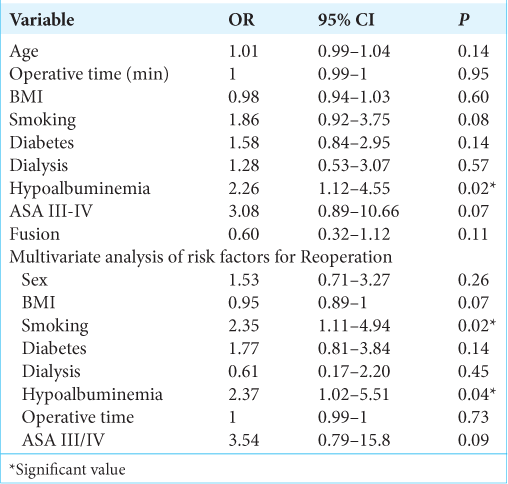
There were 39 (6.2%) patients who required spinal reoperations within 30 postoperative days. Patients who were smokers or had hypoalbuminemia were the most likely to require secondary surgery [
DISCUSSION
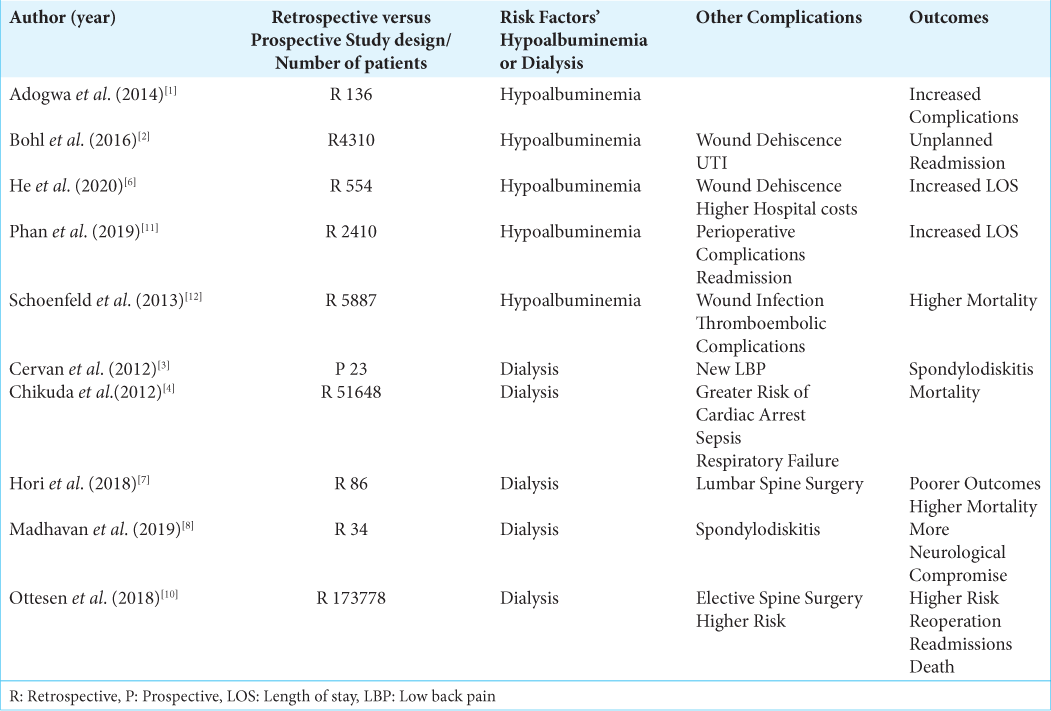
In this study, we analyzed morbidity and mortality rates for 627 patients from the ACS-NSQIP database undergoing surgery for PSI.[
Postoperative complication leading to higher reoperation rates
Postoperative complications and adverse events in spine surgery are associated with higher morbidity, reoperation rates, and greater health-care costs.[
CONCLUSION
Hypoalbuminemia was associated with a higher risk of major and wound-related complications whereas dialysis was associated with a higher mortality rate for patients undergoing primary spine surgery for spondylodiscitis.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adogwa O, Martin JR, Huang K, Verla T, Fatemi P, Thompson P. Preoperative serum albumin level as a predictor of postoperative complication after spine fusion. Spine (Phila Pa 1976). 2014. 39: 1513-9
2. Bohl DD, Shen MR, Mayo BC, Massel DH, Long WW, Modi KD. Malnutrition predicts infectious and wound complications following posterior lumbar spinal fusion. Spine (Phila Pa 1976). 2016. 41: 1693-9
3. Cervan AM, Colmenero Jde D, Del Arco A, Villanueva F, Guerado E. Spondylodiscitis in patients under haemodyalisis. Int Orthop. 2012. 36: 421-6
4. Chikuda H, Yasunaga H, Horiguchi H, Takeshita K, Kawaguchi H, Matsuda S. Mortality and morbidity in dialysis-dependent patients undergoing spinal surgery: Analysis of a national administrative database in Japan. J Bone Joint Surg Am. 2012. 94: 433-8
5. Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG. The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976). 2007. 32: 2764-70
6. He Z, Zhou K, Tang K, Quan Z, Liu S, Su B. Perioperative hypoalbuminemia is a risk factor for wound complications following posterior lumbar interbody fusion. J Orthop Surg Res. 2020. 15: 538
7. Hori Y, Takahashi S, Terai H, Hoshino M, Toyoda H, Suzuki A. Impact of hemodialysis on surgical outcomes and mortality rate after lumbar spine surgery: A matched cohort study. Spine Surg Relat Res. 2018. 3: 151-6
8. Madhavan K, Chieng LO, Armstrong VL, Wang MY. Spondylodiscitis in end-stage renal disease: A systematic review. J Neurosurg Spine. 2019. p. 1-9
9. Mylona E, Samarkos M, Kakalou E, Fanourgiakis P, Skoutelis A. Pyogenic vertebral osteomyelitis: A systematic review of clinical characteristics. Semin Arthritis Rheum. 2009. 39: 10-7
10. Ottesen TD, McLynn RP, Zogg CK, Shultz BN, Ondeck NT, Bovonratwet P. Dialysis is an independent risk factor for perioperative adverse events, readmission, reoperation, and mortality for patients undergoing elective spine surgery. Spine J. 2018. 18: 2033-42
11. Phan K, Ranson W, White SJ, Cheung ZB, Kim J, Shin JI. Thirty-day perioperative complications, prolonged length of stay, and readmission following elective posterior lumbar fusion associated with poor nutritional status. Glob Spine J. 2019. 9: 417-23
12. Schoenfeld AJ, Carey PA, Cleveland AW, Bader JO, Bono CM. Patient factors, comorbidities, and surgical characteristics that increase mortality and complication risk after spinal arthrodesis: A prognostic study based on 5,887 patients. Spine J. 2013. 13: 1171-9