- Department of Neurosurgery, University of Tsukuba, Tsukuba, Japan.
- Department of Pathology, University of Tsukuba, Tsukuba, Japan.
Correspondence Address:
Eiichi Ishikawa, Department of Neurosurgery, University of Tsukuba, Tsukuba, Japan.
DOI:10.25259/SNI_682_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hiroki Karita1, Takao Koiso1, Ai Muroi1, Noriaki Sakamoto2, Alexander Zaboronok1, Eiichi Ishikawa1. Preoperatively difficult-to-diagnose medulla oblongata germinoma: A case report and literature review. 13-Oct-2023;14:366
How to cite this URL: Hiroki Karita1, Takao Koiso1, Ai Muroi1, Noriaki Sakamoto2, Alexander Zaboronok1, Eiichi Ishikawa1. Preoperatively difficult-to-diagnose medulla oblongata germinoma: A case report and literature review. 13-Oct-2023;14:366. Available from: https://surgicalneurologyint.com/surgicalint-articles/12591/
Abstract
Background: Intracranial germinomas are rare tumors, accounting for 0.5–2% of primary intracranial neoplasms. While they typically occur in the pineal gland, suprasellar region, basal ganglia, and thalamus, germinomas arising in the medulla oblongata are exceptionally rare. Diagnosis of medulla oblongata germinoma is challenging, potentially leading to misdiagnosis and poor prognosis.
Case Description: We present a case of a 29-year-old man complaining of left leg numbness. Radiological findings revealed a contrast-enhanced lesion in the medulla oblongata. The patient underwent tumor biopsy, and intraoperative pathological diagnosis (IOD) suspected the diagnosis of medulla oblongata germinoma. He underwent chemoradiotherapy after confirming the diagnosis of germinoma. Intracranial germinoma arising in the medulla oblongata differs from germinomas in other locations due to its higher incidence in individuals in their 20s and a slight female predominance.
Conclusion: When encountering lesions in the medulla oblongata, germinoma should be considered as one of the differential diagnoses, and surgical strategies including IOD should be planned accordingly.
Keywords: Germ cell tumor, Germinoma, Medulla oblongata
INTRODUCTION
Intracranial germinomas are rare, accounting for 0.5–2% of primary intracranial tumors.[
Here, we report a case of germinoma in the medulla oblongata and summarize the epidemiology, imaging findings, treatment, and prognosis compared to previously reported cases.
CASE PRESENTATION
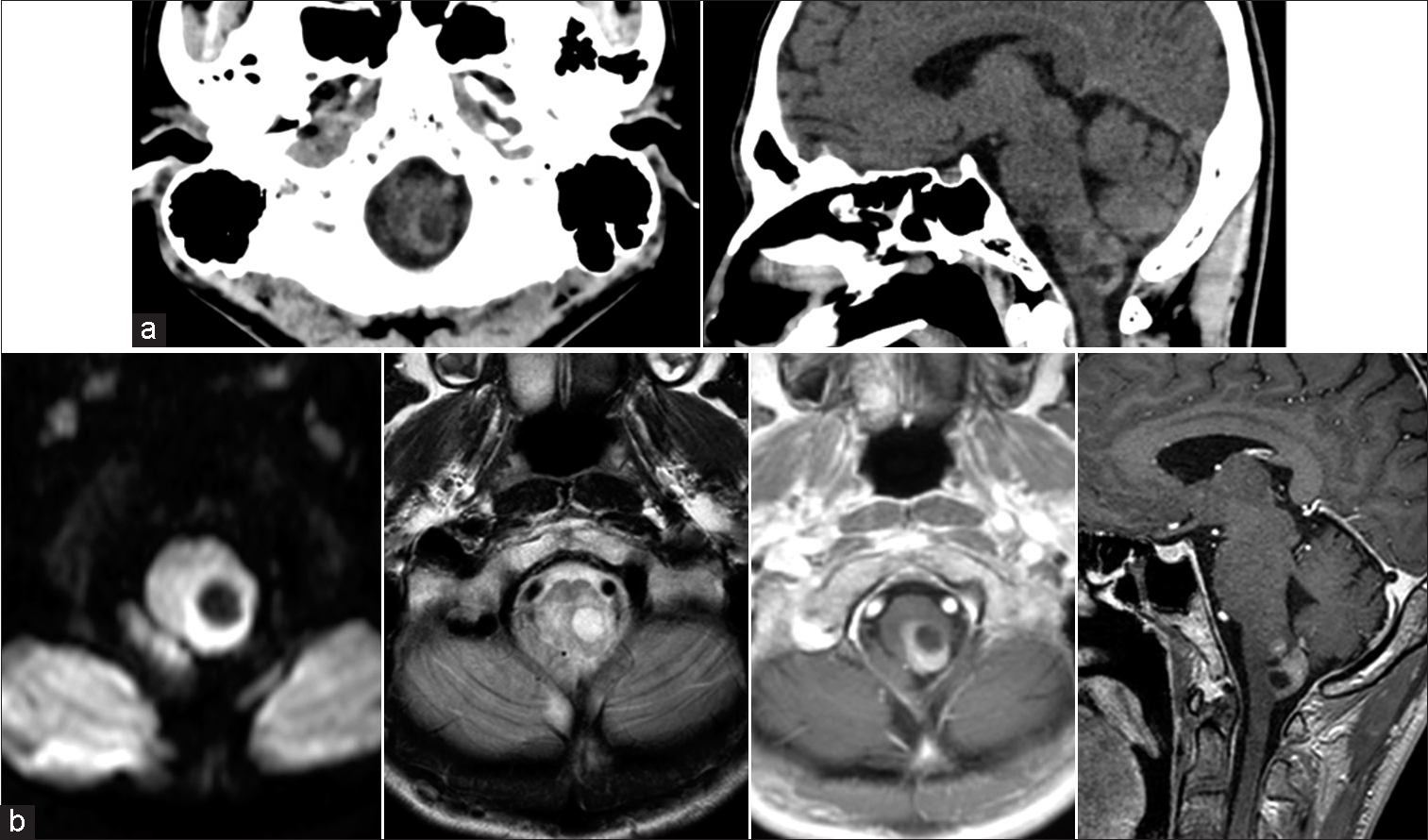
A 29-year-old man has been experiencing numbness in his left leg for a year. As the numbness progressed to the left side of the abdomen, he underwent gadolinium (Gd)-enhanced head magnetic resonance (MR) imaging at a local medical facility. The examination revealed an enhanced lesion in the medulla oblongata, and the patient was subsequently referred to our hospital. There was no significant medical history or family history, and except for the left-sided numbness, no neurological abnormalities were observed. Head computed tomography (CT) showed a hypodense lesion in the central area with hyperdense areas protruding from the medulla oblongata to the surrounding tissues [
Figure 1:
(a) Plain head computed tomography: axial (left) and sagittal (right) views show a hypodense lesion in the central area with hyperdense areas protruding from the medulla oblongata to the surrounding tissues. (b) Magnetic resonance imaging. The axial view on the diffusion-weighted image (WI) (left) and T2WI (middle left). Axial and sagittal views on T1WI with gadolinium contrast enhancement (middle right and right) shows a circumscribed enhanced mass.
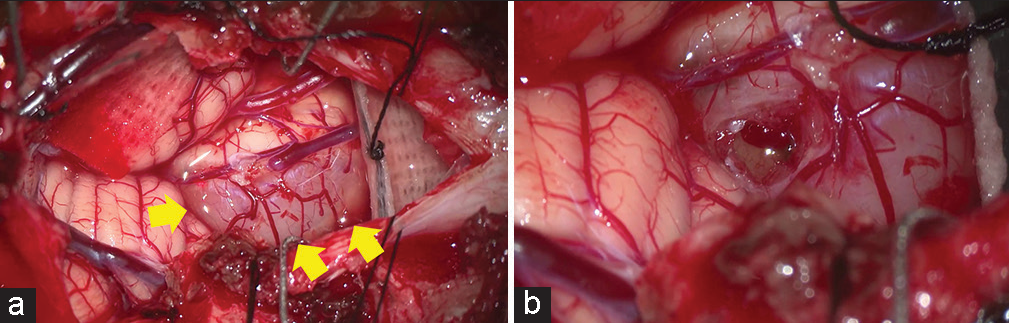
Surgical findings
The tumor located on the dorsal side of the medulla oblongata, presumably corresponding to the nucleus gracilis, was visible through the pia mater as a brown mass [
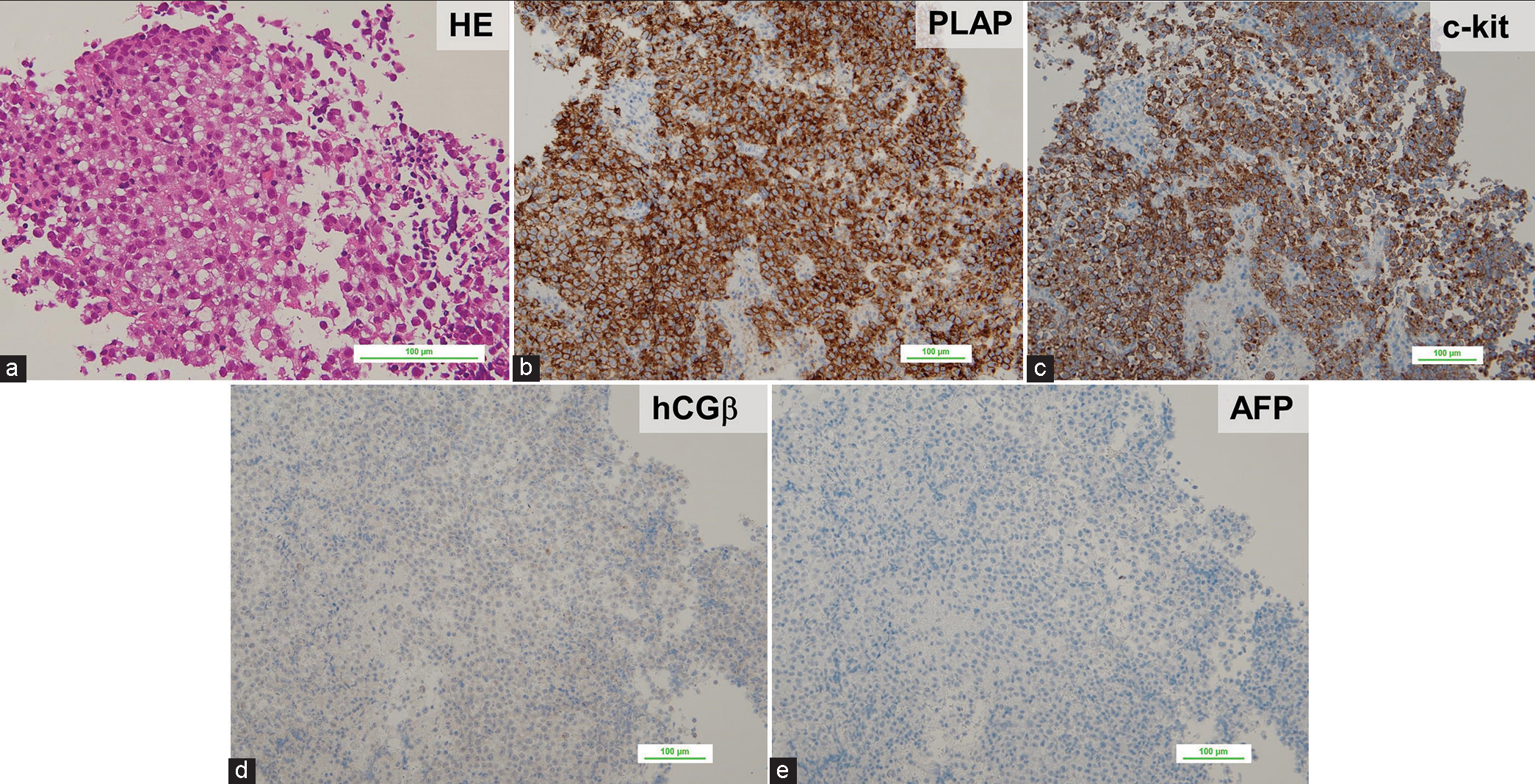
As for pathological findings [
Figure 3:
(a) Hematoxylin-Eosin (HE) staining showed the proliferation of atypical cells with relatively large nuclei, pale cytoplasm, and infiltrating lymphocytes. (b-e) Immunohistochemistry showed that the tumor cells were positive for placental alkaline phosphatase (PLAP) and c-kit antibodies, weakly positive for human chorionic gonadotropin beta (hCGβ) antibodies, and negative for alpha-fetoprotein (AFP) antibodies.
Post-operative course
Since germinoma was not suspected before surgery, blood tests were conducted to measure AFP, hCG, and hCG-β levels on the day after surgery. The results showed an AFP of 2.0 ng/ml, HCG <0.5 mIU/mL, and HCG-β <0.28 ng/ mL. Post-operative MR imaging showed no complications, and the right-side numbness remained unchanged. The patient was discharged home with a Karnofsky performance status (KPS) score of 90. Subsequently, chemotherapy using carboplatin and etoposide was initiated. After completing two cycles of chemotherapy, the contrast-enhanced lesion mostly disappeared, confirming its significant effectiveness. Therefore, radiation therapy with a total dose of 30.6 Gy in 17 fractions to all the ventricles was performed concurrently with the third cycle of chemotherapy. Post-treatment Gd-contrasted MR imaging showed no evidence of the enhanced lesion and no tumor dissemination. The patient was in good condition (KPS = 90) except for mild dysesthesia in the left extremities 6 months after the biopsy.
DISCUSSION
Intracranial germinomas predominantly occur in the pineal and suprasellar regions, basal ganglia, and thalamus.[
This suggests that medulla oblongata germinoma shows a different age distribution, occurring at a later age and being more common in women. The symptoms observed in medulla oblongata germinomas mainly involved motor and sensory abnormalities, lower cranial nerve dysfunction, and disturbances in the respiratory center, reflecting anatomical and functional impairments.
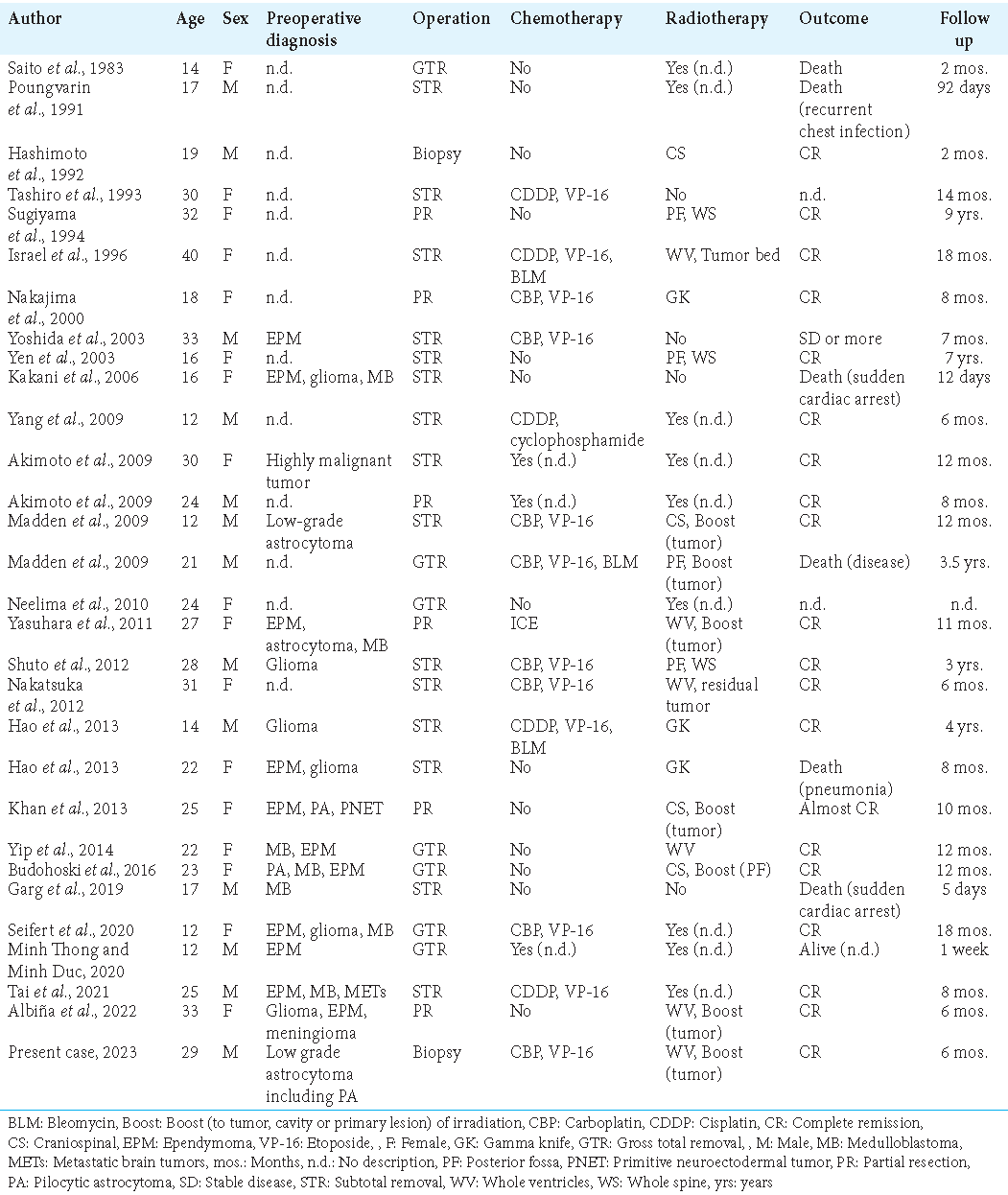
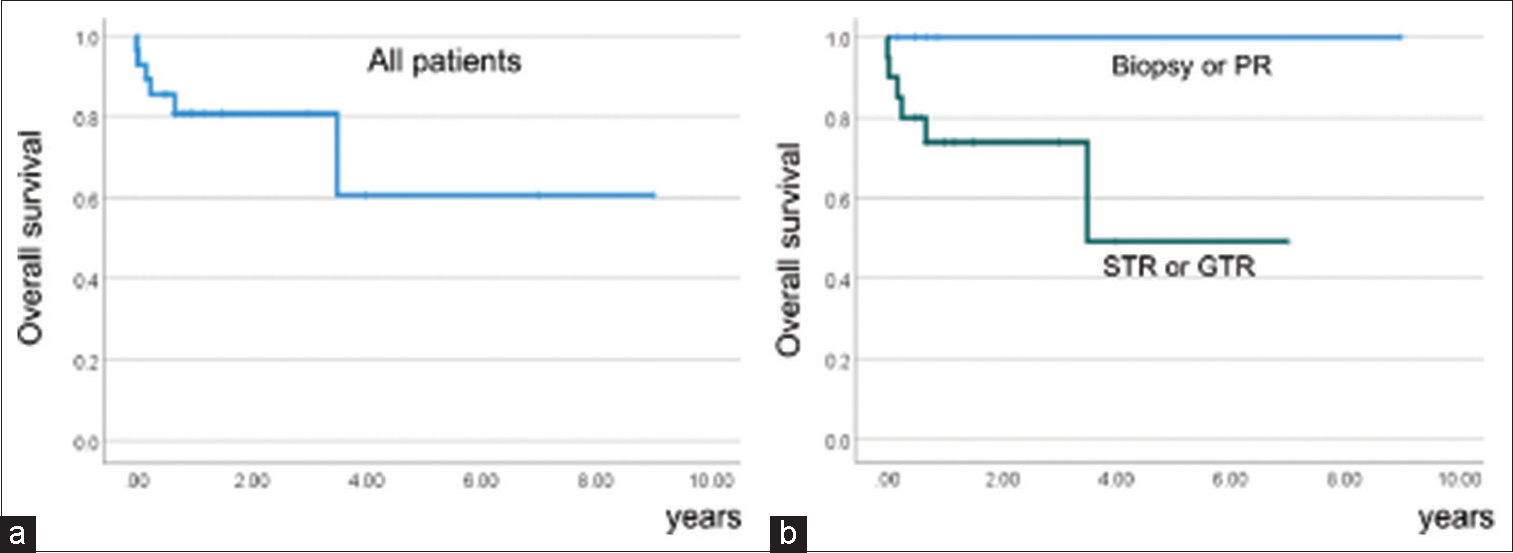
In our case review, the 1-year survival rate for the medulla oblongata germinoma was 80% [
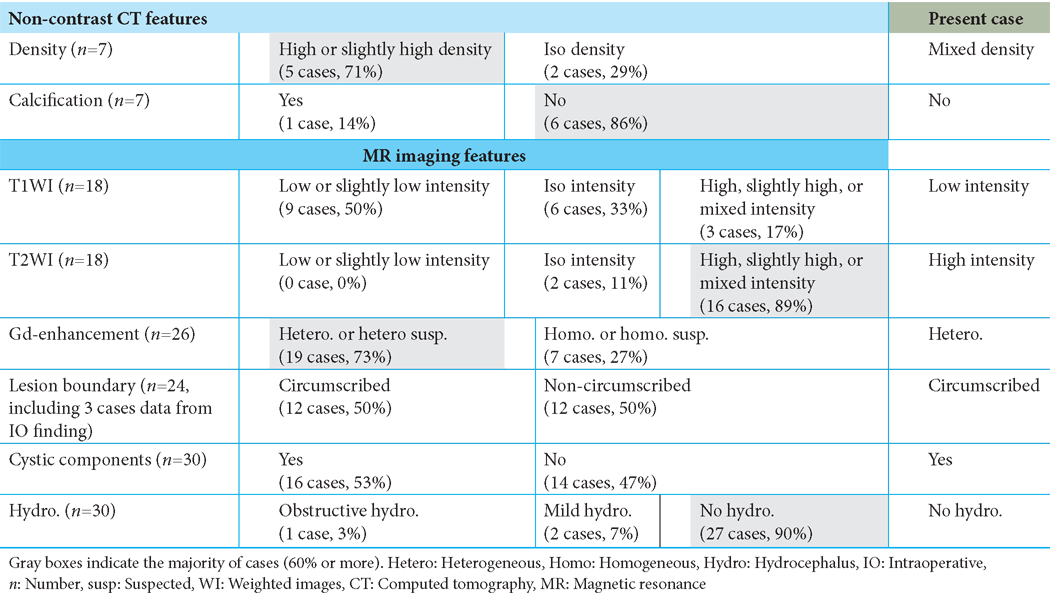
In the preoperative imaging diagnosis, including our case, ependymoma, medulloblastoma, glioma, and other lesions were considered, but not germinoma. The characteristic findings based on preoperative imaging are summarized in
Thus, the absence of hydrocephalus on CT and/or MR imaging, a high-density lesion without calcification on CT scan, and the higher prevalence in women with an onset in the 20s may provide some assistance in the differentiation from ependymoma and medulloblastoma; however, it is extremely difficult to diagnose medulla oblongata germinoma preoperatively. As mentioned above, a biopsy or PR is recommended for medulla oblongata germinoma to prevent fatal complications, such as cardiac arrest or respiratory failure. Therefore, in cases where the diagnosis of germinoma cannot be definitively ruled out based on preoperative imaging and intraoperative findings, IOD using a frozen section should be performed, and excessive resection should be avoided in confirmed or suspected germinoma cases.
CONCLUSION
Intracranial germinoma occurring in the medulla oblongata differs from germinomas in other locations, as it has a higher incidence in individuals in their 20s, a slight female predominance, and no evidence of hydrocephalus or calcification. When encountering lesions in the medulla oblongata, germinoma should be considered as one of the differential diagnoses, and surgical strategies including IOD should be planned accordingly.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
SUPPLEMENTARY
Supplementary Figure 1:
(a) A survival curve of all patients with previously reported medulla oblongata germinomas, including ours. (b) Survival curves of patients who underwent biopsy or partial resection (PR) and patients who underwent subtotal removal (STR) or gross total removal (GTR). (P = 0.122, logrank test).
References
1. Akimoto J, Murakami M, Fukami S, Ikeda Y, Haraoka J. Primary medulla oblongata germinoma--an unusual posterior fossa tumors in young adults. J Clin Neurosci. 2009. 16: 705-8
2. Albiña P, Solis A, Lorenzoni J, Henny P, Manriquez M. Primary germinoma of the medulla oblongata: Illustrative case. J Neurosurg Case Lessons. 2022. 3: CASE21315
3. Aoyama H, Shirato H, Kakuto Y, Inakoshi H, Nishio M, Yoshida H. Pathologically-proven intracranial germinoma treated with radiation therapy. Radiother Oncol. 1998. 47: 201-5
4. Budohoski KP, O’Donovan DG, Harris F, Santarius T. Germinoma of the medulla oblongata-a case report. Br J Neurosurg. 2016. 30: 348-50
5. Echevarría ME, Fangusaro J, Goldman S. Pediatric central nervous system germ cell tumors: A review. Oncologist. 2008. 13: 690-9
6. Garg K, Sharma R, Gurjar HK, Kale SS. Pontomedullary germinoma with suprasellar and spinal metastasis: A report and comprehensive review of literature. Neurol India. 2019. 67: 308-11
7. Hao S, Li D, Feng J, Wang L, Wu Z, Zhang J. Primary medulla oblongata germinomas: Two case reports and review of the literature. World J Surg Oncol. 2013. 11: 274
8. Hashimoto M, Hatasa M, Shinoda S, Masuzawa T. Medulla oblongata germinoma in association with Klinefelter syndrome. Surg Neurol. 1992. 37: 384-7
9. Israel Z, Lossos A, Ashkenazi E, Soffer D, Umansky F. Germinoma and choroid plexus papilloma coexisting in the fourth ventricle. Acta Neurochir (Wien). 1996. 138: 1252-3
10. Jennings MT, Gelman R, Hochberg F. Intracranial germ-cell tumors: Natural history and pathogenesis. J Neurosurg. 1985. 63: 155-67
11. Kanamori M, Kumabe T, Saito R, Yamashita Y, Sonoda Y, Ariga H. Optimal treatment strategy for intracranial germ cell tumors: A single institution analysis. J Neurosurg Pediatr. 2009. 4: 506-14
12. Kakani AB, Karmarkar VS, Deopujari CE, Shah RM, Bharucha NE, Muzumdar G. Germinoma of fourth ventricle: A case report and review of literature. J Pediatr Neurosci. 2006. 1: 33-5
13. Khan AA, Kirkman MA, Anderson C, Jaunmuktane Z, Morris RC, Kitchen ND. An unusual anatomic and geographic location of primary germinoma of the fourth ventricle. J Clin Neurosci. 2013. 20: 1620-2
14. Madden J, Foreman NK, Liu AK. Germ cell tumors of the brainstem: Report on two cases with pulmonary complications and a review of the literature. J Neurooncol. 2009. 93: 405-8
15. Minh Thong P, Minh Duc N. A rare case of intra-fourth-ventricular germinoma, derived from the medulla oblongata. Pediatr Neurosurg. 2020. 55: 426-31
16. Nakajima H, Iwai Y, Yamanaka K, Yasui T, Kishi H. Primary intracranial germinoma in the medulla oblongata. Surg Neurol. 2000. 53: 448-51
17. Nakatsuka S, Tateishi A, Nagano T, Kimura H, Nakajo K, Takahashi J. Primary extragonadal germinoma of the medulla oblongata. Int J Surg Pathol. 2012. 20: 276-9
18. Neelima R, Mathew A, Kapilamoorthy TR, Radhakrishnan VV. Germinoma of medulla. Neurol India. 2010. 58: 768-70
19. Osuka S, Tsuboi K, Takano S, Ishikawa E, Matsushita A, Tokuuye K. Long-term outcome of patients with intracranial germinoma. J Neurooncol. 2007. 83: 71-9
20. Poungvarin N, Nimmannitya J, Issaragrisil R, Sangruchi T. Brainstem germinoma presenting as intermittent apnoea: A rare entity: Report of one patient and review of literature. J Med Assoc Thai. 1991. 74: 55-60
21. Saito A, Yamashita T, Ishiwata Y, Hirata K, Kuwabara T. A case of germinoma of the fourth ventricle. Shoni No Noshinkei. 1983. 8: 43-8
22. Seifert K, Huttner A, Malhotra A. A rare case of a pediatric medullary intracranial germinoma. World Neurosurg. 2020. 138: 137-40
23. Shuto T, Ohtake M, Matsunaga S, Hasegawa N. Primary medulla oblongata germinoma in a male patient. J Clin Neurosci. 2012. 19: 769-71
24. Sugiyama K, Uozumi T, Goishi J, Sogabe T, Arita K, Maeda H. Germinoma of the medulla oblongata--case report. Neurol Med Chir (Tokyo). 1994. 34: 291-4
25. Tai LH, Yang SF, Chen YL, Chong YB, Yu TC, Lieu AS. Medulla oblongata germinoma with Klinefelter syndrome. Br J Neurosurg. 2021. 23: 1-6
26. Tashiro T, Yoshida J, Wakabayashi T, Sugita K, Abe H. Primary intracranial germinoma involving the medulla oblongata--case report. Neurol Med Chir (Tokyo). 1993. 33: 251-4
27. Tsurubuchi T, Hara K, Takano S, Muroi A, Fukushima H, Mizumoto M. Factors influencing craniospinal relapse of intracranial germinoma after complete remission. World Neurosurg. 2022. 166: e325-36
28. Yang DT, Rozen WM, Rickert CH, Lo PA. Primary pontomedullary germinoma in a 12 year old boy. J Clin Neurosci. 2009. 16: 321-5
29. Yasuhara T, Ichikawa T, Miyoshi Y, Kurozumi K, Maruo T, Yanai H. Primary germinoma in the medulla oblongata-case report-. Neurol Med Chir (Tokyo). 2011. 51: 326-9
30. Yen PS, Chou AS, Chen CJ, Jung SM, Chuang HL, Scott RM. Primary medulla oblongata germinoma: A case report and review of the literature. J Neurooncol. 2003. 62: 339-42
31. Yip CM, Tseng HH, Hsu SS, Liao WC, Chen JY, Chen CH. Dyspnea and choking as presenting symptoms in primary medulla oblongata germinoma. Surg Neurol Int. 2014. 5: S170-4
32. Yoshida K, Nakao Y, Yamamoto T, Mori K, Maeda M. Germinoma in the fourth ventricle. Acta Neurochir (Wien). 2003. 145: 789-92