- Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita, Japan
- Department of Neurosurgery, Imari Arita Kyoritsu Hospital, Arita, Japan
- Department of Neurosurgery, Shiroishi Kyoritsu Hospital, Shiroishi, Japan
- Department of Orthopaedic Surgery, Faculty of Medicine, Saga University, Saga, Japan.
Correspondence Address:
Tatsuya Tanaka, Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita, Japan.
DOI:10.25259/SNI_818_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tatsuya Tanaka1, Hideki Iwashita2, Xuan Liu3, Nobuaki Momozaki2, Eiichiro Honda3, Akira Matsuno1, Tadatsugu Morimoto4. Prevalence of idiopathic normal pressure hydrocephalus in patients with vertebral compression fractures. 15-Dec-2023;14:429
How to cite this URL: Tatsuya Tanaka1, Hideki Iwashita2, Xuan Liu3, Nobuaki Momozaki2, Eiichiro Honda3, Akira Matsuno1, Tadatsugu Morimoto4. Prevalence of idiopathic normal pressure hydrocephalus in patients with vertebral compression fractures. 15-Dec-2023;14:429. Available from: https://surgicalneurologyint.com/surgicalint-articles/12671/
Abstract
Background: Patients with idiopathic normal pressure hydrocephalus (iNPH) may be more prone to all fracture types due to falls. Vertebral compression fractures (VCFs) are a global burden that temporarily or permanently affects millions of elderly people. This study aimed to investigate the prevalence of iNPH in patients with VCFs.
Methods: We retrospectively reviewed 128 patients aged 60–102 years who underwent balloon kyphoplasty (BKP) for VCFs between November 1, 2017, and March 31, 2020. We also assessed the presence of the iNPH triad (i.e., gait disturbance, cognitive impairment, and urinary incontinence). Patients with Evans’ index (EI) >0.3 and the iNPH triad were defined as having possible iNPH, those with clinical improvement after a cerebrospinal fluid tap test were defined as having probable iNPH, and those with clinical improvement after a shunt surgery were defined as having definite iNPH.
Results: Of the 128 patients, seven were excluded due to a history of intracranial disease that could cause ventricular enlargement or gait disturbance. Another 70 patients who did not undergo head computed tomography or magnetic resonance imaging one year before or after BKP were excluded from the study. Finally, 51 patients with a mean age of 78.9 years were enrolled. The mean EI value of these 51 patients was 0.28, with 18 patients showing EI >0.3. Moreover, 18 had possible iNPH, one had probable iNPH, and one had definite iNPH.
Conclusion: Screening for iNPH in elderly patients with VCFs can allow early diagnosis of iNPH and benefit them more from surgical treatment.
Keywords: Balloon kyphoplasty, Disproportionately enlarged subarachnoid space hydrocephalus, Idiopathic normal pressure hydrocephalus, Prevalence of idiopathic normal pressure hydrocephalus, Risk factor, Shunt, Vertebral compression fracture
INTRODUCTION
Idiopathic normal pressure hydrocephalus (iNPH) is a progressive syndrome of unknown cause characterized by the iNPH triad (i.e., gait disturbance, cognitive impairment, and urinary incontinence) in the elderly, ventricular enlargement on neurological imaging, normal cerebrospinal fluid (CSF) pressure, and improvement with shunt surgery.[
The prevalence of vertebral compression fractures (VCFs) in people aged 70 and ≥80 years has been reported to be 26.3% and 41.5%, respectively, in men and 27.1% and 53.0%, respectively, in women.[
We hypothesized that patients with VCFs may include those with iNPH and predicted that early detection and treatment may help prevent fractures due to falls. This study aimed to investigate the prevalence of iNPH in patients with VCFs.
MATERIALS AND METHODS
Patient
We retrospectively reviewed a consecutive series of 128 patients aged 60–102 years who presented to Imariarita Kyoritsu Hospital in Arita, Japan, and underwent BKP for VCFs over 29 months between November 1, 2017, and March 31, 2020.
Patients who did not undergo head computed tomography (CT) or magnetic resonance imaging (MRI) 1 year before or after BKP were excluded from the study.
Patients younger than 60 years were excluded because iNPH is rare in individuals in their 40s and 50s, although international guidelines define the onset of this disease to be after 40 years of age. Patients with a history of ventricular enlargement, such as cerebral contusion and subarachnoid hemorrhage, were excluded from the study. Moreover, patients with a history of neurological diseases, such as Parkinson’s disease and hemiplegia due to stroke, which can cause gait disturbance, were excluded from the study. Those with progressive symptoms of Alzheimer’s disease, Lewy body dementia, or frontotemporal dementia were included in the study to avoid underdiagnosis of iNPH because disease entities may be indistinguishable.
Patients’ electronic medical records were retrospectively reviewed.
Radiological assessments
In this study, we used Evans’ index (EI) and disproportionately enlarged subarachnoid space hydrocephalus (DESH) to evaluate imaging findings characteristic of iNPH. We defined cases with significant DESH findings or those with DESH findings and EI >0.3 as possible iNPH cases.
Definition of iNPH
According to the Clinical Guidelines for iNPH, 3rd edition,[
Patients who showed clinical improvement after a CSF tap test were defined as having probable iNPH. For the CSF tap test, 30 mL CSF was removed. Patients with abnormal CSF analysis results, such as protein >50 mg/dL, cell count >3 cells/mL, or CSF pressure >20 cm H2O, were excluded.
The following items were assessed after the tap test: (1) Timed Up and Go Test (TUG), which assesses the number of seconds required for the individual to stand up from a chair, walk 3 m at their usual pace past a safety cone on the floor, turn around, walk back to the chair, and sit back down again with their back against the chair. (2) We defined the following improvements as a positive result of the tap test: (a) an improvement of ≥11% in the TUG test, (b) an improvement of ≥3 points in the Mini-Mental State Examination (MMSE), or (c) an improvement of ≥1 point in urinary incontinence on the iNPH Grading Scale (iNPH GS).
Patients with probable iNPH who showed clinical improvement after shunt surgery (shunt responders) were diagnosed with definite iNPH.
A lumboperitoneal shunt was used as the first-line treatment, while a ventriculoperitoneal shunt was selected for patients with severe lumbar spinal deformity or spinal canal stenosis.
Patients who showed an improvement of ≥11% on the TUG test, ≥3 points on the MMSE, or ≥1 point on the iNPH GS 1 month after surgery, were considered shunt responders.
RESULTS
Of the 128 patients who presented and underwent BKP, seven were excluded because they had a history of intracranial disease that could cause ventricular enlargement or gait disturbance, such as brain tumors, cerebral contusions, hemiplegia due to stroke, and Parkinson’s disease. Moreover, another 70 patients who did not undergo a head CT or MRI scans were excluded from the study. Finally, 51 patients who underwent head CT or MRI 1 year before or after BKP were included in the study.
The mean age of the patients included in this study was 78.9 years. Of the 51 patients, 17 (33.3%) were male and 34 (66.7%) were female. The mean EI value was 0.28, with 18 patients (35.3%) showing EI >0.3. Five of the 18 patients (27.8%) had DESH.
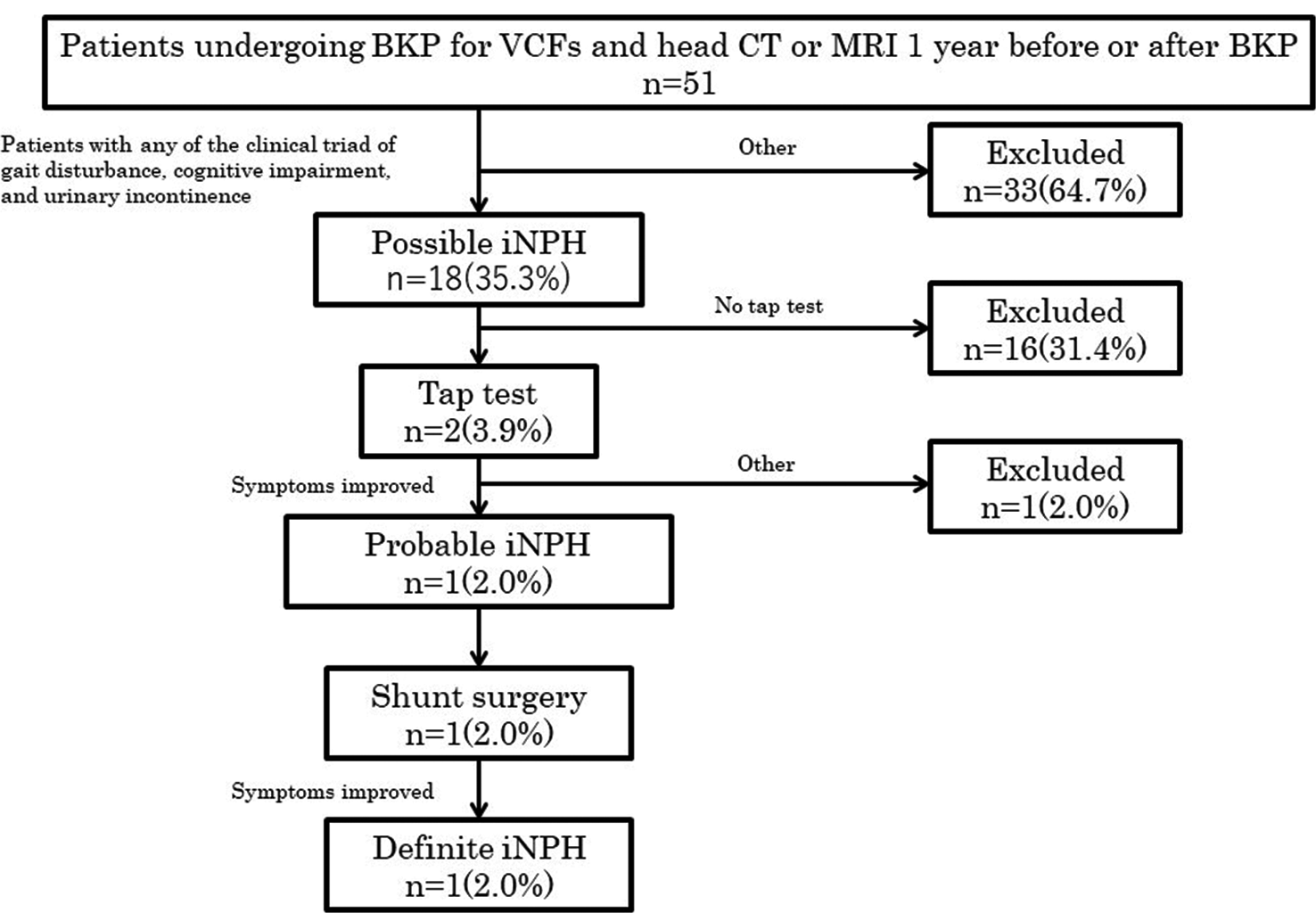
Of the 51 patients who underwent BKP, 18 (35.3%) were diagnosed with possible iNPH after presenting with the clinical triad (i.e., gait disturbance, cognitive impairment, and urinary incontinence). Of the 18 patients with possible iNPH, two (3.9% of all 51 patients under study) underwent a CSF tap test. One of the two patients (2.0% of all 51 patients under study) who underwent a tap test was diagnosed with probable iNPH with clinical improvement of ≥11% in the TUG score, ≥3 points in the MMSE, or ≥1 point in urinary incontinence on the iNPH GS. Among the patients with probable iNPH who underwent shunt surgery, one (2.0% of all 51 patients under study) was diagnosed with definite iNPH one month after shunt surgery with an improvement of ≥1% in the TUG score, 3 points in the MMSE, and 1 point in the iNPH GS.
Figure 1:
Flowchart of the process used to identify possible idiopathic normal pressure hydrocephalus (iNPH), probable iNPH, and definite iNPH in 51 patients who underwent balloon kyphoplasty (BKP) for vertebral compression fractures (VCFs) and head computed tomography or magnetic resonance imaging one year before or after BKP. Of the 51 patients, 18 (35.3%) had possible iNPH (meeting the following two criteria: Evans’ index >0.3 and any of the three clinical features of iNPH: Gait disturbance, cognitive impairment, and urinary incontinence). Of the 18 patients with possible iNPH, two (3.9%) underwent a cerebrospinal fluid tap test, and one (2.0%) showed clinical improvement. Shunt surgery was performed in one patient (2.0%), and one (2.0%) showed clinical improvement.
DISCUSSION
This is the first retrospective study to investigate the prevalence of iNPH in patients with VCFs. In this study, the mean EI value of the 51 patients with VCFs under study was 0.28, with 18 patients (35.3%) showing EI >0.3. Iseki et al. revealed that among elderly subjects aged 61–72 years in Japan, 6.46% had EI >0.3.[
Gait disturbance is the most common initial clinical symptom of iNPH, and 82.6% of patients with iNPH had a history of falls within six months before shunt surgery,[
This study has several limitations. Because this study involved patients with VCFs who underwent BKP, the results of this study theoretically cannot be applied to all patients with VCFs. In addition, due to the retrospective nature of this study, 57.9% of the 121 patients with VCFs who underwent BKP were not evaluated using CT or MRI. Therefore, our sample may not accurately represent the population of patients with VCFs, and iNPH may have affected some patients who were not screened. Finally, this was a single-center study. This finding must be replicated with additional cases from multiple institutions.
CONCLUSION
The prevalence of possible iNPH was 35.3% in patients who underwent BKP for VCFs. This study also suggests that screening for iNPH in elderly patients with VCFs can allow early diagnosis of iNPH, who may benefit more from surgical treatment.
Ethical approval
The authors declare that this work complies the guidelines for human studies, and the research was conducted ethicallly in accordance with the World Medical Association Declaration of Helsinki.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Andersson J, Rosell M, Kockum K, Lilja-Lund O, Söderström L, Laurell K. Prevalence of idiopathic normal pressure hydrocephalus: A prospective, population-based study. PLoS One. 2019. 14: e0217705
2. Andrén K, Wikkelsø C, Tisell M, Hellström P. Natural course of idiopathic normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry. 2014. 85: 806-10
3. Hakim S, Adams RD. The special clinical problem of symptomatic hydrocephalus with normal cerebrospinal fluid pressure. Observations on cerebrospinal fluid hydrodynamics. J Neurol Sci. 1965. 2: 307-27
4. Horii C, Asai Y, Iidaka T, Muraki S, Oka H, Tsutsui S. Differences in prevalence and associated factors between mild and severe vertebral fractures in Japanese men and women: The third survey of the ROAD study. J Bone Miner Metab. 2019. 37: 844-53
5. Hsieh MK, Chen LH, Chen WJ. Current concepts of percutaneous balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures: Evidence-based review. Biomed J. 2013. 36: 154-61
6. Iseki C, Kawanami T, Nagasawa H, Wada M, Koyama S, Kikuchi K. Asymptomatic ventriculomegaly with features of idiopathic normal pressure hydrocephalus on MRI (AVIM) in the elderly: A prospective study in a Japanese population. J Neurol Sci. 2009. 277: 54-7
7. Jaraj D, Rabiei K, Marlow T, Jensen C, Skoog I, Wikkelsø C. Estimated ventricle size using Evans index: Reference values from a population-based sample. Eur J Neurol. 2017. 24: 468-74
8. Missori P, Rughetti A, Peschillo S, Gualdi G, Di Biasi C, Nofroni I. In normal aging ventricular system never attains pathological values of Evans’ index. Oncotarget. 2016. 7: 11860-3
9. Nakajima M, Yamada S, Miyajima M, Ishii K, Kuriyama N, Kazui H. Guidelines for management of idiopathic normal pressure hydrocephalus (Third Edition): Endorsed by the Japanese society of normal pressure hydrocephalus. Neurol Med Chir (Tokyo). 2021. 61: 63-97
10. Natori T, Komiyama K, Sonoda K, Utsunomiya T, Fujimura K, Jinbayashi H. Prevalence of idiopathic normal pressure hydrocephalus in patients with hip fractures: A propensity-matched cohort study. J Am Geriatr Soc. 2023. 71: 290-2
11. Nikaido Y, Akisue T, Urakami H, Kajimoto Y, Kuroda K, Kawami Y. Postural control before and after cerebrospinal fluid shunt surgery in idiopathic normal pressure hydrocephalus. Clin Neurol Neurosurg. 2018. 172: 46-50
12. Oike R, Inoue Y, Matsuzawa K, Sorimachi T. Screening for idiopathic normal pressure hydrocephalus in the elderly after falls. Clin Neurol Neurosurg. 2021. 205: 106635
13. Selge C, Schoeberl F, Zwergal A, Nuebling G, Brandt T, Dieterich M. Gait analysis in PSP and NPH: dual-task conditions make the difference. Neurology. 2018. 90: e1021-8
14. Tanaka N, Yamaguchi S, Ishikawa H, Ishii H, Meguro K. Prevalence of possible idiopathic normal-pressure hydrocephalus in Japan: The Osaki-Tajiri project. Neuroepidemiology. 2009. 32: 171-5
15. Tanaka T, Fujiwara R, Sashida R, Hirokawa Y, Wakamiya T, Michiwaki Y. Surgical treatment of vertebral compression fracture in a patient with idiopathic normal pressure hydrocephalus. JMA J. 2023. 6: 354-7