- Department of Neurosurgery, Institute of Neurosurgery, Madras Medical College, Chennai, Tamil Nadu, India
Correspondence Address:
Srihari Sridharan
Department of Neurosurgery, Institute of Neurosurgery, Madras Medical College, Chennai, Tamil Nadu, India
DOI:10.4103/sni.sni_495_16
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Srihari Sridharan, D. Balasubramanian. Primary calvarial tuberculosis. 21-Jun-2017;8:126
How to cite this URL: Srihari Sridharan, D. Balasubramanian. Primary calvarial tuberculosis. 21-Jun-2017;8:126. Available from: http://surgicalneurologyint.com/surgicalint-articles/primary-calvarial-tuberculosis/
Abstract
Background:Tuberculosis is a very common disease in India. Its prevalence, capacity to affect every other organ, and atypical presentations make it an important part of the differential diagnosis for cases presenting in the rural setup. Primary tuberculous caries of the calvarium is a rare manifestation of this common entity.
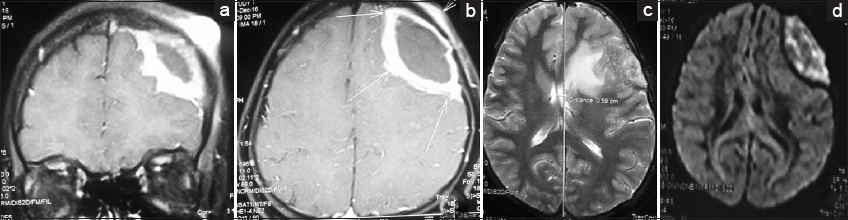
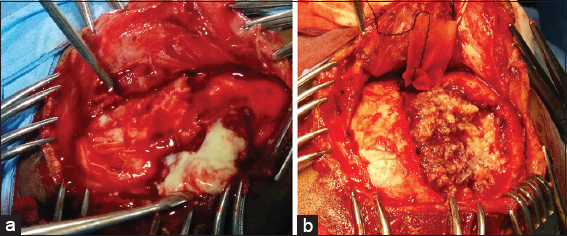
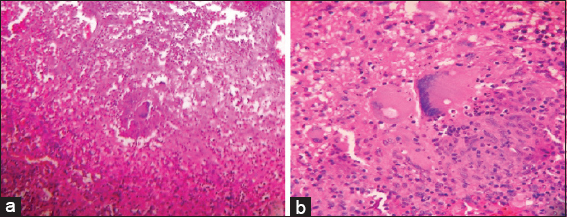
Case Description:A young lady presented with headache and discharging sinus of the scalp. Imaging revealed epidural abscess with midline shift. She underwent surgery, and histopathological diagnosis of tuberculous etiology was made. The pre and intraoperative images, radiological images, and histopathological images are reported and discussed.
Conclusion:Tuberculosis should be included in the differential diagnosis of the osteolytic lesions of skull with discharging sinus. A high degree of suspicion, especially in patients from low socioeconomic status, is warranted in managing such cases.
Keywords: Calvarium, skull tuberculosis, TB, tuberculosis
INTRODUCTION
Tuberculosis is a major public health problem with a significant effect on the economy of developing countries. The social stigma associated with the disease cannot be understated. Malnutrition, overcrowding, poor sanitation, lack of hygiene, lack of awareness, and delay in seeking medical care contribute significantly to the spread of the disease. Extrapulmonary tuberculosis is the term used to describe isolated occurrence of tuberculosis at body sites other than the lung.[
CASE HISTORY
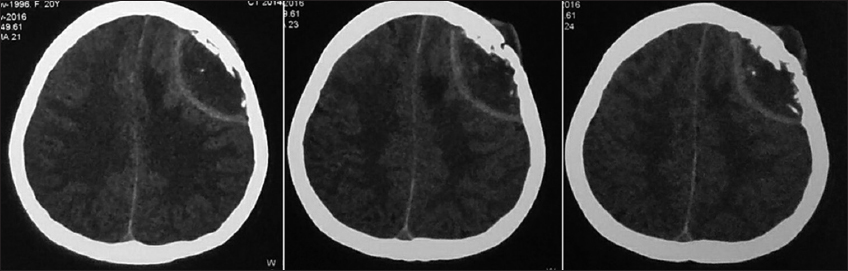
A 20-year-old lady from the rural parts of Tamil Nadu, south India presented with complaints of headache for the past 4 months and persistent discharging sinus from the left frontal scalp region for 1 month [
DISCUSSION
Reid reported the first case of calvarial tuberculosis.[
Anti-tuberculous therapy forms the mainstay of the treatment[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Barton . Tuberculosis of the vault of the skull. Br J Radiol. 1961. 34: 286-90
2. Biniwale SN, Rajshekhar V. Tuberculous osteomyelitis of bone flap following craniotomy for a glioma. Neurol India. 2000. 48: 91-2
3. Diyora B, Kumar R, Modgi R, Sharma A. Calvarial tuberculosis: A report of eleven patients. Neurol India. 2009. 57: 607-12
4. Gupta PK, Sastry-Kolluri VR, Chandramouli BA, Venkatramana NK, Das BS. Calvarial tuberculosis: A report of 2 cases. Neurosurgery. 1989. 25: 830-33
5. Ip M, Tsui E, Wong KL, Jones B, Pung CF, Ngan H. Disseminated skeletal tuberculosis with skull involvement. Tuberc Lung Dis. 1993. 74: 211-4
6. Jadhav RN, Palande DA. Calvarial tuberculosis. Neurosurgery. 1999. 45: 1345-50
7. LeRoux PD, Griffin GE, Marsh HT, Winn HR. Tuberculosis of the skull; A rare condition-Case report and review of the literature. Neurosurgery. 1990. 26: 851-5
8. Ramdurg SR, Gupta DK, Suri A, Sharma BS, Mahapatra AK. Calvarial tuberculosis: Uncommon manifestation of common disease – A series of 21 cases. Br J Neurosurg. 2010. 24: 572-7
9. Raut AA, Nagar AM, Muzumdar D, Chawla AJ, Narlawar RS, Fattepurkar S. Imaging features of calvarial tuberculosis: A study of 42 cases. Am J Neuroradiol. 2004. 25: 409-14
10. Sharma SK, Mohan A. Extrapulmonary tuberculosis. Indian J Med Res. 2004. 120: 316-53