- Department of Orthopaedic P D Hinduja National Hospital and Medical Research Centre, Mumbai, Maharashtra, India.
- Department of Radiology, P D Hinduja National Hospital and Medical Research Centre, Mumbai, Maharashtra, India.
Correspondence Address:
Pratik Patel
Department of Radiology, P D Hinduja National Hospital and Medical Research Centre, Mumbai, Maharashtra, India.
DOI:10.25259/SNI_759_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Pratik Patel1, Dhanish Mehendiratta1, Vivek Bhambhu1, Samir Dalvie1, Aniruddha Kulkarni2, Bhavesh Popat2. Psoas hematoma due to segmental vessel injury leads to paresis following CT-guided biopsy of lumbar vertebrae: A case report. 22-Dec-2020;11:457
How to cite this URL: Pratik Patel1, Dhanish Mehendiratta1, Vivek Bhambhu1, Samir Dalvie1, Aniruddha Kulkarni2, Bhavesh Popat2. Psoas hematoma due to segmental vessel injury leads to paresis following CT-guided biopsy of lumbar vertebrae: A case report. 22-Dec-2020;11:457. Available from: https://surgicalneurologyint.com/surgicalint-articles/10482/
Abstract
Background: Percutaneous bone biopsy is the first-line procedure for obtaining a tissue diagnosis to confirm focal, diffuse vertebral, and/or paravertebral metastatic lesions. Percutaneous bone biopsy to evaluate metastatic disease can be performed under fluoroscopy, ultrasonography, magnetic resonance (MR) imaging, and computed tomography (CT). Notably, CT-scans best direct and demonstrate the needle position for these procedures, decreasing the risk of injury to critical adjacent structures (e.g. major vessels, nerve roots). Hemorrhagic complication to lumbar segmental arteries following needle biopsy are uncommon; only a few cases have been reported. Although percutaneous bone biopsy is typically safe when performed utilizing computed tomography (CT) guidance, here we encountered a 60-year-old-female who developed a L4 lumbar segmental artery psoas hematoma following this procedure requiring emergent embolization.
Case Description: A 60-year-old female, with a history of breast cancer, underwent a CT-guided core needle biopsy of an L4 lytic lesion (e.g., likely a metastasis). This acutely resulted in the onset of radicular leg pain and weakness. When the postprocedural CT scan demonstrated a large psoas hematoma attributed to laceration of the left posterior L4 segmental artery, the patient required emergent embolization. Following this procedure, she exhibited a fully neurological recovery.
Conclusion: Following a CT-guided L4 vertebral biopsy to document metastatic breast carcinoma, a 60-year-old patient developed an immediate postprocedure CT-documented psoas hematoma due to laceration of the left posterior L4 segmental artery. Following emergent embolization, the patient recovered full neurological function.
Keywords: Angiography, Computed tomography-guided biopsy, Embolization, Lumbar segmental vessel injury, Psoas muscle hematoma
INTRODUCTION
Percutaneous bone biopsy is typically the first-line procedure for obtaining a tissue diagnosis for unifocal, diffuse vertebral, and/or paravertebral metastatic disease; the complication rate typically ranges from 0% to 10%.[
CASE PRESENTATION
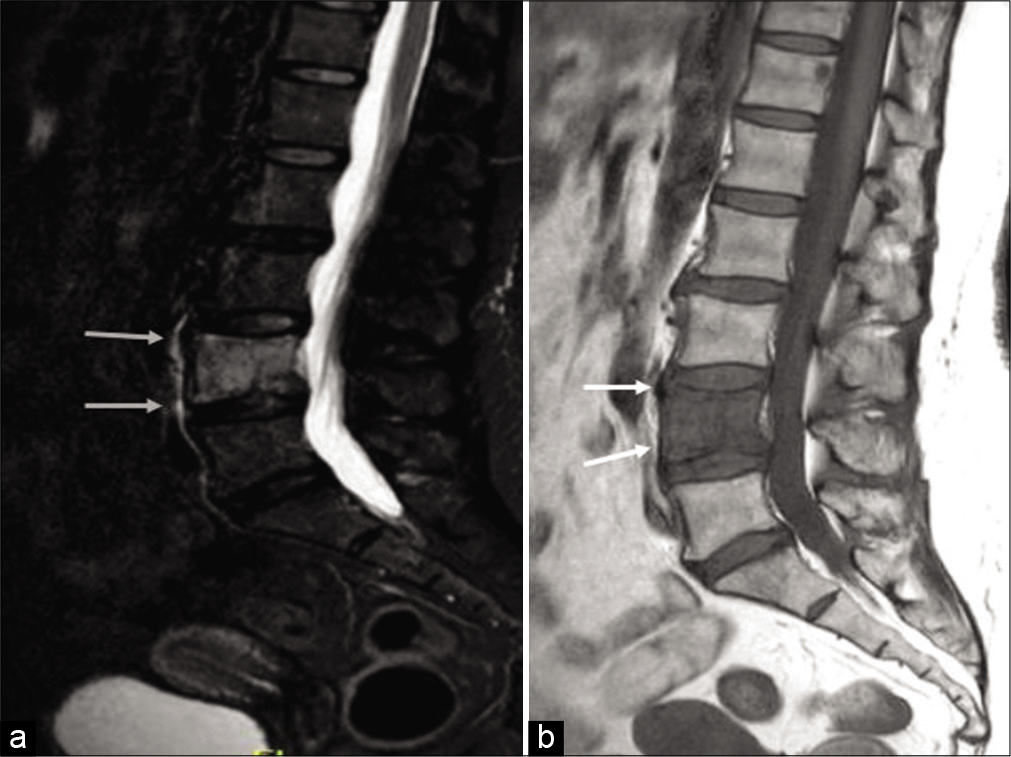
A 60-year-old female, recently diagnosed with right-sided infiltrating pleomorphic lobular breast carcinoma, presented with back pain attributed to a positron emission tomography-CT documented L4 vertebral body lytic lesion. When the MRI showed a T1 hypointense/short-tau inversion recovery hyperintense lesion involving the L4 vertebral body (e.g., including the pedicles and lamina), a CT-guided core needle biopsy was performed to document whether this was a metastatic lesion [
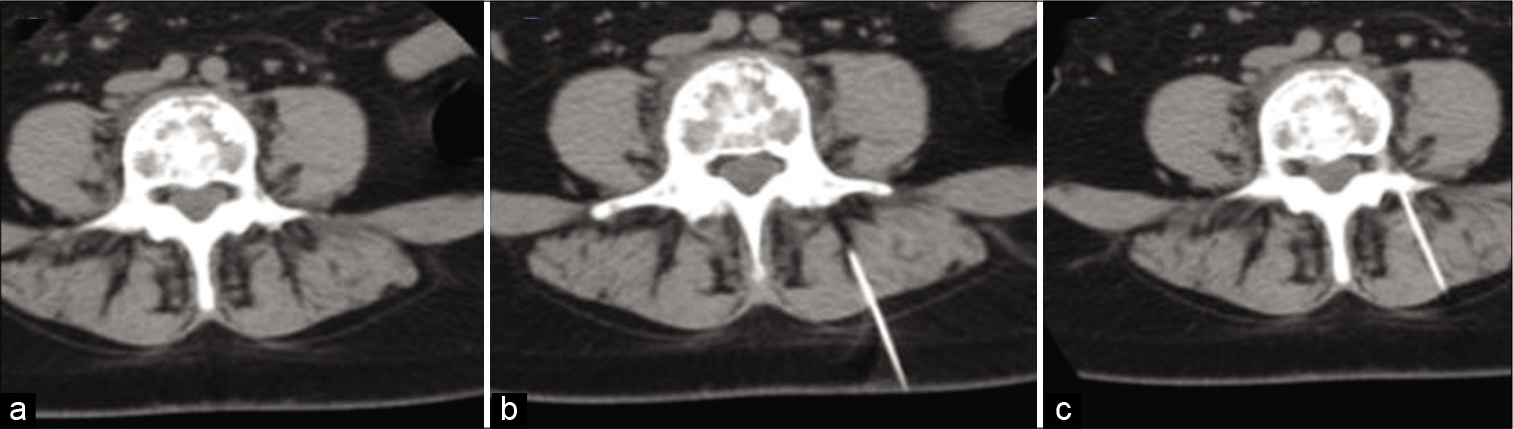
CT-guided biopsy of L4
The CT-guided biopsy of the L4 vertebral body was performed under local anesthesia, and the histopathological examination was consistent with metastatic breast carcinoma [
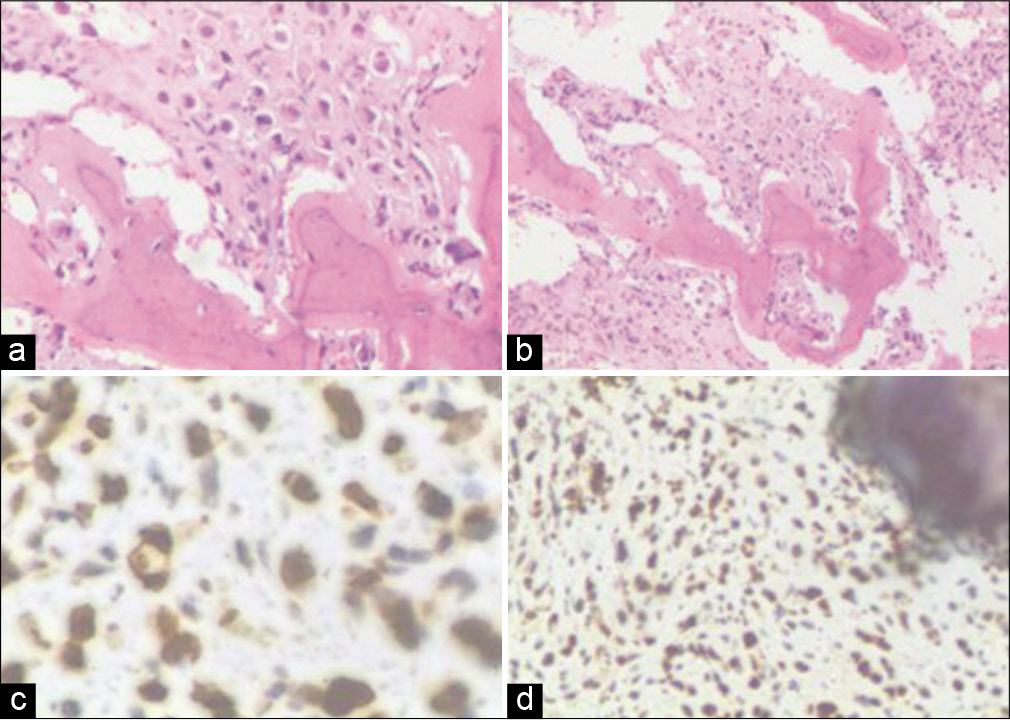
Figure 3:
Histopathological images of the computed tomography-guided biopsy from L4 vertebrae, (a) ×40 and (b) ×20 H and E stained image – showing bony trabeculae infiltrated by neoplastic cells having hyperchromatic nuclei, (c) ×40 and (d) ×20 immunohistochemistry image – tumor cells show GATA 3 positivity.
Diagnosis and treatment of psoas hematoma
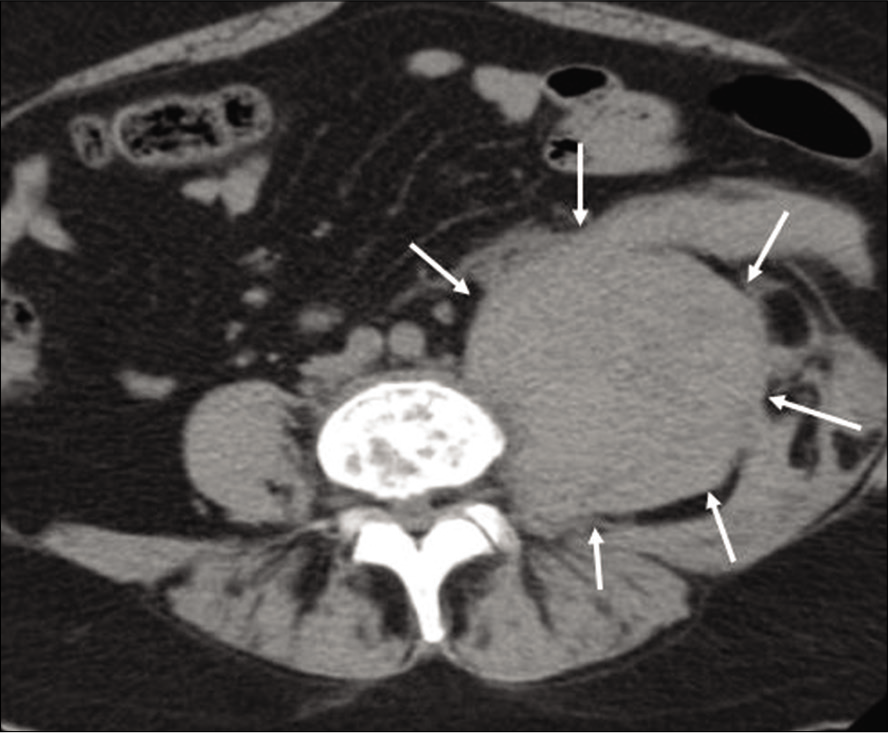
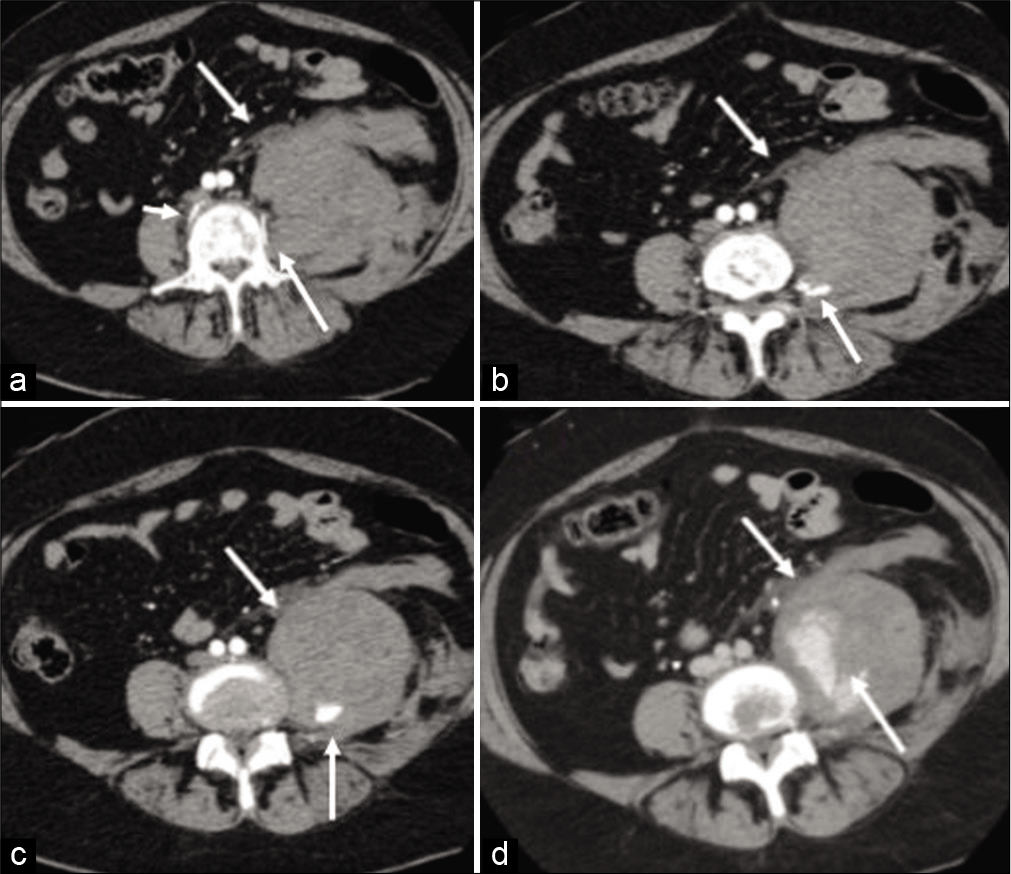
The emergent postprocedure CT scan confirmed an acute left psoas hematoma [
DISCUSSION
The complication rate for spinal percutaneous vertebral body biopsies ranges from 0% to 10%.[
Many case reports document how CT-guided spinal biopsies provide for more optimal/accurate needle position, thus reducing the risk of neural or vascular injuries.[
Monitoring of clinical symptoms and vital signs for patients undergoing such procedures is critical to rapidly diagnosing complications like the neurovascular injury seen in this case.
CTA is the diagnostic study of choice as it best defines the site of active bleeding following a CT-guided biopsy (e.g., resultant hemorrhage potentially attributed to traumatic laceration of lumbar vertebral arteries).[
CONCLUSION
Following a CT-guided vertebral body biopsy, a psoas hematoma arising from a lacerated L4 lumbar vertebral artery injury was successfully treated with endovascular embolization.
Ethical approval
Not applicable. As this submission is a single case report an ethical approval is not necessary. However, written informed consents were obtained from the patient for publication of this case report and any accompanying mages.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ashizawa R, Ohtsuka K, Kamimura M, Ebara S, Takaoka K. Percutaneous transpedicular biopsy of thoracic and lumbar vertebrae-method and diagnostic validity. Surg Neurol. 1999. 52: 545-51
2. Babu NV, Titus VTK, Chittaranjan S, Abraham G, Prem H, Korula RJ. Computed tomographically guided biopsy of the spine. Spine (Phila Pa 1976). 1994. 19: 2436-42
3. Ceyhan M, Belet U, Aslan S, Ayyildiz S, Gol K. Traumatic lumbar artery pseudoaneurysm: The role of CT angiography in diagnosis and treatment. Diagn Interv Radiol. 2010. 16: 162-4
4. Chan KT, Korivi N. Lumbar artery pseudoaneurysm in traumatic spinal cord injury: A case report. Arch Phys Med Rehabil. 2003. 84: 455-7
5. Dupuy DE, Rosenberg AE, Punyaratabandhu T, Tan MH, Mankin HJ. Accuracy of CT-guided needle biopsy of musculoskeletal neoplasms. AJR Am J Roentgenol. 1998. 171: 759-62
6. Fyfe IS, Henry AP, Mulholland RC. Closed vertebral biopsy. J Bone Joint Surg Br. 1983. 65: 140-3
7. Hadjipavlou AG, Kontakis GM, Gaitanis JN, Katonis PG, Lander P, Crow WN. Effectiveness and pitfalls of percutaneous transpedicle biopsy of the spine. Clin Orthop Relat Res. 2003. 411: 54-60
8. Kornblum MB, Wesolowski DP, Fischgrund JS, Herkowitz HN. Computed tomography-guided biopsy of the spine. A review of 103 patients. Spine (Phila Pa 1976). 1998. 23: 81-5
9. Metzger CS, Johnson DW, Donaldson WF. Percutaneous biopsy in the anterior thoracic spine. Spine (Phila Pa 1976). 1993. 18: 374-8
10. Murphy WA, Destouet JM, Gilula LA. Percutaneous skeletal biopsy 1981: A procedure for radiologists-results, review, and recommendations. Radiology. 1981. 139: 545-9
11. Nijenhuis RJ, Sluzewski M, van Rooij WJ. Iatrogenic lumbar pseudoaneurysm causing dural sac compression after spine surgery. J Neurosurg Spine. 2009. 10: 585-6
12. Ortiz AO, Zoarski GH, Mathis JM.editors. Image-guided percutaneous spine biopsy. Image-Guided Spine Interventions. New York: Springer; 2004. p. 69-93
13. Santillan A, Patsalides A, Gobin YP. Endovascular embolization of iatrogenic lumbar artery pseudoaneurysm following extreme lateral interbody fusion (XLIF). Vasc Endovascular Surg. 2010. 44: 601-3
14. Stringham DR, Hadjipavlou A, Dzioba RB, Lander P. Percutaneous transpedicular biopsy of the spine. Spine (Phila Pa 1976). 1994. 19: 1985-91
15. Szolar DH, Preidler KW, Steiner H, Riepl T, Flaschka G, Stiskal M. Vascular complications in lumbar disk surgery: Report of four cases. Neuroradiology. 1996. 38: 521-5