- Department of Neurosurgery, Osaka University, Graduate School of Medicine, Suita, Japan
- Department of Neurosurgery, Iseikai International General Hospital, Osaka, Japan.
Correspondence Address:
Koshi Ninomiya, Department of Neurosurgery, Osaka University, Graduate School of Medicine, Suita, Japan.
DOI:10.25259/SNI_88_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Natsuki Nakamura1, Koshi Ninomiya1, Masahiro Ishihara2, Akihiro Yamamoto1, Manabu Sasaki1, Haruhiko Kishima1. Psoriasis vulgaris of the skin caused a L3-L4 lumbar epidural spinal abscess. 12-Apr-2024;15:125
How to cite this URL: Natsuki Nakamura1, Koshi Ninomiya1, Masahiro Ishihara2, Akihiro Yamamoto1, Manabu Sasaki1, Haruhiko Kishima1. Psoriasis vulgaris of the skin caused a L3-L4 lumbar epidural spinal abscess. 12-Apr-2024;15:125. Available from: https://surgicalneurologyint.com/surgicalint-articles/12857/
Abstract
Background: In a 31-year-old male, psoriasis vulgaris (PV) of the skin caused paraparesis attributed to a L3-L4 epidural spinal abscess that required emergent surgical decompression.
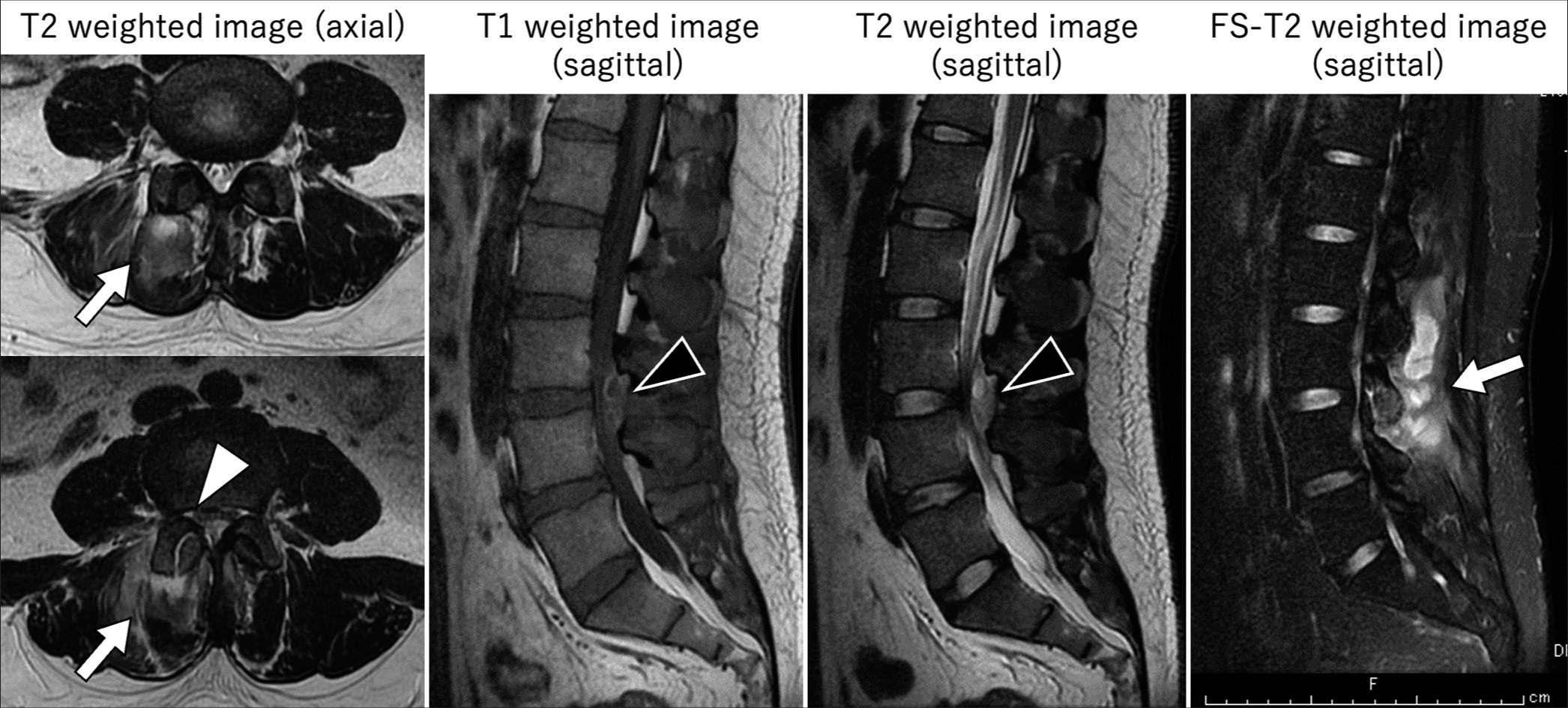
Case Description: A 31-year-old male presented with lower back pain and cauda equina compression attributed to a magnetic resonance-documented L34 enhancing lesion consistent with a spinal epidural abscess (SEA). The skin over the L3-L4 level revealed severe PV that proved to be the likely etiology of the right-sided paraspinal muscle abscess, infected right L3-L4 facet joint, and SEA. At surgery, the foci of infection were excised/decompressed, and cultures grew methicillin-susceptible Staphylococcus aureus. Following surgery, the patient was improved and was treated with appropriate antibiotic therapy.
Conclusion: PV caused a L3-L4 epidural spinal abscess and cauda equina compression in a 31-year-old male who was successfully treated with operative decompression and appropriate antibiotic management.
Keywords: Epidural abscess, Facet joint arthritis, Methicillin-susceptible Staphylococcus aureus, Paraspinal muscle abscess, Psoriasis vulgaris
INTRODUCTION
Psoriasis vulgaris (PV) affects 85–90% of patients with psoriasis; it is the most common phenotype of atopic dermatitis. PV typically involves extensor surfaces of the elbows, knees, sacral region, and scalp. Here, a 31-year-old male with PV over the L3-L4 lumbar level presented with a cauda equina syndrome attributed to a L3-L4 spinal epidural abscess (SEA).
CASE DESCRIPTION
A 31-year-old male presented with one week of lower back pain, fever, bilateral lower extremity numbness, and one day of paraplegia with loss of sphincter function (i.e., cauda equina syndrome). The lumbar magnetic resonance (MR) documented an enhancing right paraspinal abscess that extended into the right L3-L4 facet joint and spinal epidural compartment[
Surgery
The incision for the laminectomy extended directly through the large erythematous skin lesion containing a small exudate (i.e., later diagnosed as PV) [
Figure 2:
We found a skin lesion on the patient’s lower back. It was a large erythema with a small amount of exudate. There was no apparent fistula, but an inflammatory state was suspected. This lesion was diagnosed as psoriasis vulgaris by a dermatologist, which was severe but improved with topical medication.
Postoperative course
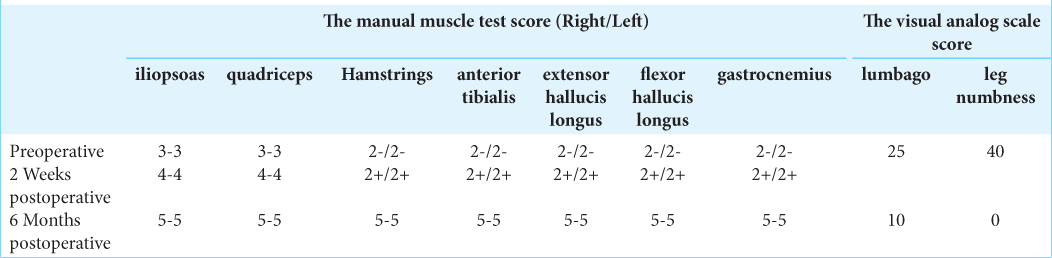
Postoperatively, the patient’s lower extremity motor function improved to nearly normal (i.e., 4/5 level). Two weeks postoperatively, the lumbar MR showed no residual L3-L4 epidural abscess. Six months after surgery, the patient was neurologically intact [
DISCUSSION
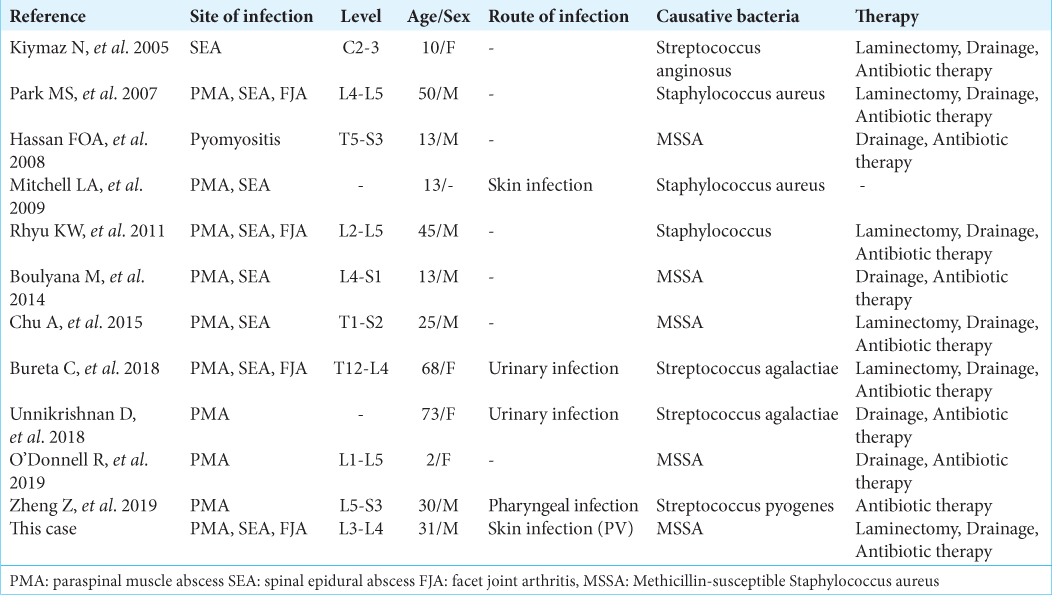
Few studies report SEAs attributed to infection [
CONCLUSION
PV caused a L3-L4 epidural spinal abscess that was quickly diagnosed, decompressed, and treated with appropriate antibiotic therapy.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Boulyana M, Kilani MS. Nontropical pyomyositis complicated with spinal epidural abscess in a previously healthy child. Surg Neurol Int. 2014. 5: S119-21
2. Bureta C, Tominaga H, Yamamoto T, Setoguchi T, Kawamura H, Nagano S. Lumbar spine epidural abscess and facet joint septic arthritis due to Streptococcus agalactiae A case report. BMC Surg. 2018. 18: 16
3. Hassan FO, Shannak A. Primary pyomyositis of the paraspinal muscles: A case report and literature review. Eur Spine J. 2008. 17: 239-42
4. Kiymaz N, Demir O. Spontaneous cervical paraspinal and epidural giant abscess in a child--case report--. Neurol Med Chir (Tokyo). 2005. 45: 540-2
5. Mitchell LA, Rooks VJ, Martin JE, Burgos RM. Paraspinal tropical pyomyositis and epidural abscesses presenting as low back pain. Radiol Case Rep. 2009. 4: 303
6. Park MS, Moon SH, Hahn SB, Lee HM. Paraspinal abscess communicated with epidural abscess after extra-articular facet joint injection. Yonsei Med J. 2007. 48: 711-4
7. Rhyu KW, Park SE, Ji JH, Park I, Kim YY. Pyogenic arthritis of the facet joint with concurrent epidural and paraspinal abscess: A case report. Asian Spine J. 2011. 5: 245-9
8. Unnikrishnan D, Delacruz MA, Saha A, Daniels R. Case of acute paraspinal pyomyositis in an elderly diabetic secondary to spread from urinary tract infection. BMJ Case Rep. 2018. 2018: bcr2018225739