- Department of Neurosurgery, Zahedan University of Medical Sciences, Zahedan, Iran.
- Department of Radiology, Zahedan University of Medical Sciences, Zahedan, Iran.
- Department of Neurosurgery, Mashhad University of Medical Sciences, Mashhad, Iran.
- Department of Radiology, Faculty of Medicine, Islamic Azad University, Mashhad, Iran.
- Department of Neurosurgery, Razavi Hospital, Mashhad, Iran.
Correspondence Address:
Daniel Kheradmand, Department of Neurosurgery, Mashhad University of Medical Sciences, Mashhad, Iran.
DOI:10.25259/SNI_46_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohammad Safdari1, Zohre Safdari2, Masoud Pishjoo3, Sirous Seifirad4, Daniel Kheradmand3, Sajjad Saghebdoust5. Radiological outcome of operative treatment with posterior approach in patients with thoracolumbar junction traumatic injuries: A single-center pilot study in a developing country. 26-Aug-2022;13:376
How to cite this URL: Mohammad Safdari1, Zohre Safdari2, Masoud Pishjoo3, Sirous Seifirad4, Daniel Kheradmand3, Sajjad Saghebdoust5. Radiological outcome of operative treatment with posterior approach in patients with thoracolumbar junction traumatic injuries: A single-center pilot study in a developing country. 26-Aug-2022;13:376. Available from: https://surgicalneurologyint.com/surgicalint-articles/11835/
Abstract
Background: The thoracolumbar junction (TLJ) represents a transition zone of the spine that leads to a high incidence of fractures. The treatment of burst fractures remains controversial regarding the ideal management. This study assessed the postoperative radiological outcome of TLJ fixation in patients with TLJ injuries who underwent surgery.
Methods: All traumatic patients with TLJ injuries who were referred to the Khatam hospital of Zahedan between 2015 and 2020, with their thoracolumbar injury classification and severity score (TLICS) of four or more and who underwent surgery, were included in this study. The patients who entered the study were called for a follow-up examination. The degree of kyphosis, proximal junctional kyphosis, and fusion were assessed in these patients.
Results: Among 273 patients, the average age was 43.5 ± 12.3 (21–73) years. One hundred and ninety-eight patients (72.5%) had no neurological symptoms at admission. Based on the above criteria, the kyphosis angle of these patients was calculated before surgery, which in 46 patients (16.8%), the kyphosis angle was more than 25°. Preoperation kyphosis was significantly associated with follow-up kyphosis (P P > 0.05).
Conclusion: According to our study, the posterior spinal fixation procedure is a low-complication method with an acceptable radiological outcome. Although kyphosis before surgery is a factor in developing long-term kyphosis, it is not associated with nonfusion and PJK.
Keywords: Posterior spinal fixation, Radiological outcome, Thoracolumbar junction, Trauma
INTRODUCTION
Thoracolumbar spinal cord injuries are often caused by high-energy injuries, most of which are caused by a car accident or falling.[
Fortunately, most spinal fractures are stable, do not require surgery, and are usually cured with proper hyperextension braces.[
Several studies have reported the consequences of TLJ fracture surgery compared to conservative treatment and have reported different results.[
MATERIALS AND METHODS
A prospective cohort was performed on the patients with TLJ injuries who were referred to Khatam Al-Anbia hospital in Zahedan (Southeast Iran Referral Center) between 2015 and 2020. Inclusion criteria were age over 18 years, traumatic injury to the vertebrae of the TLJ area including vertebrae T10, T11, T12, L1, and L2, with the thoracolumbar injury classification and severity score (TLICS)[
The patients that enrolled in the study were called for a follow-up examination. It should be noted that all of these patients were examined at least 1 year after surgery. In follow-up studies, all patients were evaluated based on neurological status (ASIA score) and imaging findings (kyphosis angle and fusion status). The 36-inch film longstanding radiography was used to check the kyphosis of the fracture area. The amount of kyphosis was calculated based on the cobb method of a healthy vertebra above and below the damaged vertebra 00.[
In a study on proximal junctional kyphosis (PJK), the sagittal Cobb angle should be more than 20° between the inferior endplate of the upper instrumented vertebra and the superior endplate of two vertebrae above the upper instrumented vertebra.[
The following criteria were also used to investigate the presence of fusion:
No motion or <3° of intersegment position change on lateral flexion and extension views Lack of a lucent area around the implant Minimal loss of disc height No fracture of the instrument, bone graft, or vertebrae No sclerotic change in the graft or adjacent vertebrae Visible osseous formation in or around the cage.[
All patient data were entered into particular forms based on the hospital files, electronic health documents, and clinical findings during follow-up and were analyzed by SPSS ver 23 software. Chi-square and t-test were used to analyze this data.
Written informed consent was obtained from all patients before they participated in the study, and ethical criteria were observed throughout the study.
RESULTS
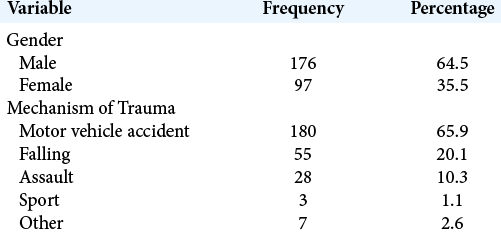
A total of 273 patients (176 males and 97 females) with an average age of 43.5 ± 12.3 (21–73) years were studied. In 180 cases (65.9%), motor vehicle accidents were the most common cause of injury, followed by falls from heights and assault from other causes of injury [
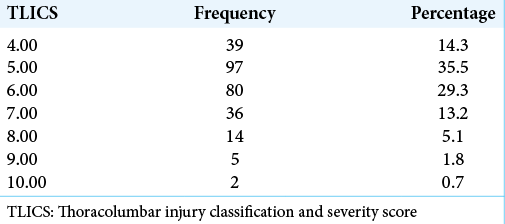
One hundred and ninety-eight patients (72.5%) had no neurological symptoms at admission. According to the TILCS rating, the mean score of these patients undergoing surgery was 5.6 ± 1.1 [
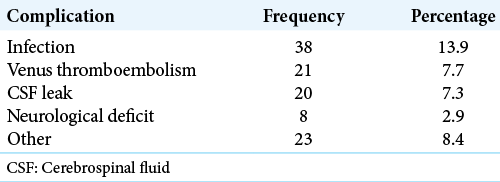
The mean hospitalization in the patients was 7.58 ± 2.35 days. Forty-seven patients (17.2%) had surgery complications during their hospitalization, the most common of which was infection [
DISCUSSION
The TLJ area refers to the T10 to L2 vertebrae, which is the most common area for fractures in the thoracic spine.[
Fortunately, most spinal fractures are stable, do not require surgery, and are often cured with proper braces or hyperextension.[
According to the previous studies, surgical indications based on the presence of canal compromise, neurological defects, reduction in body height, and the presence of kyphosis were used relatively.[
In 2005, Vaccaro et al. introduced a new classification for thoracolumbar fractures called TLICS. According to this classification, patients who receive a score of 3 or less do not need surgery; however, patients with a score of 5 or higher must undergo surgery. In cases where the patient’s score is 4, the type of treatment is based on the surgeon’s judgment.[
This study assessed the radiological outcomes of patients with traumatic TLJ who underwent posterior approach fixation surgery. About one-third of patients had a follow-up neurological status assessment based on the ASIA score. In our study, the degree of preoperative kyphosis was directly associated with the follow-up kyphosis; the higher the degree of preoperative kyphosis, the higher the rate of follow-up kyphosis. However, this variable was not related to nonfusion and PJK. So far, few studies have explored the outcome of patients who suffered TLJ injuries. A retrospective study by Kraemer et al. showed that patients with kyphosis more than 25° had poorer outcomes.[
Krompinger et al. found that about 36% of burst fractures in their follow-up examinations had changed more than 10°.[
Aoife Feeley et al. found that anterior approaches led to increase in the rate of complications.[
CONCLUSION
According to the results of previous studies, in TLJ traumatic injuries, conservative treatment is associated with significant complications such as prolonged immobility, delayed return to work, higher chances of developing kyphosis, and less spinal stabilization. According to the general results and radiological studies of follow-up in our study, it can be concluded that the posterior spinal fixation procedure is a low complication method and with an acceptable radiological outcome. Although kyphosis before surgery is a factor in developing long-term kyphosis, it is not associated with nonfusion and PJK. Although we evaluated the radiological outcome of these patients in this study, further studies are needed to determine the long-term clinical outcome in these patients.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Chow GH, Nelson BJ, Gebhard JS, Brugman JL, Brown CW, Donaldson DH. Functional outcome of thoracolumbar burst fractures managed with hyperextension casting or bracing and early mobilization. Spine (Phila Pa 1976). 1996. 21: 2170-5
2. Dai LY, Yao WF, Cui YM, Zhou Q. Thoracolumbar fractures in patients with multiple injuries: Diagnosis and treatment-a review of 147 cases. J Trauma. 2004. 56: 348-55
3. De Stefano F, Haddad H, Mayo T, Nouman M, Fiani B. Outcomes of anterior vs posterior approach to single-level lumbar spinal fusion with interbody device: An analysis of the nationwide inpatient sample. Clin Neurol Neurosurg. 2022. 212: 107061
4. DeWald RL. Burst fractures of the thoracic and lumbar spine. Clin Orthop Relat Res. 1984. 189: 150-61
5. Feeley A, Feeley I, Clesham K, Butler J. Is there a variance in complication types associated with ALIF approaches? A systematic review. Acta Neurochir (Wien). 2021. 163: 2991-3004
6. Gertzbein SD. Scoliosis research society. Multicenter spine fracture study. Spine (Phila Pa 1976). 1992. 17: 528-40
7. Grazier K.editors. The Frequency of Occurrence, Impact, Cost of Selected Musculoskeletal Conditions in the United States. Rosemont, Illinois: American Academy of Orthopaedic Surgeons; 1984. p.
8. Hsu JM, Joseph T, Ellis AM. Thoracolumbar fracture in blunt trauma patients: Guidelines for diagnosis and imaging. Injury. 2003. 34: 426-33
9. Kraemer WJ, Schemitsch EH, Lever J, McBroom RJ, McKee MD, Waddell JP. Functional outcome of thoracolumbar burst fractures without neurological deficit. J Orthop Trauma. 1996. 10: 541-4
10. Krompinger WJ, Fredrickson BE, Mino DE, Yuan HA. Conservative treatment of fractures of the thoracic and lumbar spine. Orthop Clin North Am. 1986. 17: 161-70
11. McLain RF, Sparling E, Benson DR. Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am. 1993. 75: 162-7
12. Price C, Makintubee S, Herndon W, Istre GR. Epidemiology of traumatic spinal cord injury and acute hospitalization and rehabilitation charges for spinal cord injuries in Oklahoma, 1988-1990. Am J Epidemiol. 1994. 139: 37-47
13. Ray CD. Threaded fusion cages for lumbar interbody fusions. An economic comparison with 360 degrees fusions. Spine (Phila Pa 1976). 1997. 22: 681-5
14. Reid DC, Hu R, Davis LA, Saboe LA. The nonoperative treatment of burst fractures of the thoracolumbar junction. J Trauma. 1988. 28: 1188-94
15. Scheer JK, Fakurnejad S, Lau D, Daubs MD, Coe JD, Paonessa KJ. Results of the 2014 SRS survey on PJK/ PJF: A report on variation of select SRS member practice patterns, treatment indications, and opinions on classification development. Spine (Phila Pa 1976). 2015. 40: 829-40
16. Siebenga J, Segers MJ, Leferink VJ, Elzinga MJ, Bakker FC, Duis HJ. Cost-effectiveness of the treatment of traumatic thoracolumbar spine fractures: Nonsurgical or surgical therapy?. Indian J Orthop. 2007. 41: 332-6
17. Vaccaro AR, Lehman RA, Hurlbert RJ, Anderson PA, Harris M, Hedlund R. A new classification of thoracolumbar injuries: The importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976). 2005. 30: 2325-33
18. Vaccaro AR, Zeiller SC, Hulbert RJ, Anderson PA, Harris M, Hedlund R. The thoracolumbar injury severity score: A proposed treatment algorithm. J Spinal Disord Tech. 2005. 18: 209-15
19. Wall BA, Moskowitz A, Whitaker MC, Jones TL, Stuckey RM, Carr-Maben CL. Functional outcomes of thoracolumbar junction spine fractures. Kans J Med. 2017. 10: 30-4
20. White AA, Panjabi MM. The basic kinematics of the human spine. A review of past and current knowledge. Spine (Phila Pa 1976). 1978. 3: 12-20
21. Wood KB, Bohn D, Mehbod A. Anterior versus posterior treatment of stable thoracolumbar burst fractures without neurologic deficit: A prospective, randomized study. J Spinal Disord Tech. 2005. 18: S15-23
22. Wood KB, Buttermann GR, Phukan R, Harrod CC, Mehbod A, Shannon B. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit: A prospective randomized study with follow-up at sixteen to twenty-two years: *. J Bone Joint Surg Am. 2015. 97: 3-9
23. Wood KB, Li W, Lebl DR, Ploumis A. Management of thoracolumbar spine fractures. Spine J. 2014. 14: 145-64