- Department of Neurosurgery, The National Hospital for Neurology and Neurosurgery, London
- Department of Neurosurgery, Hull Royal Infirmary, Hull, United Kingdom
Correspondence Address:
Sayal Parag
Department of Neurosurgery, Hull Royal Infirmary, Hull, United Kingdom
DOI:10.4103/2152-7806.183496
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Parag S, Arif Z, Chittoor R. Radiotherapy-related intracranial aneurysms: A role for conservative management. Surg Neurol Int 03-Jun-2016;7:
How to cite this URL: Parag S, Arif Z, Chittoor R. Radiotherapy-related intracranial aneurysms: A role for conservative management. Surg Neurol Int 03-Jun-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/radiotherapy%e2%80%91related-intracranial-aneurysms-a-role-for-conservative-management/
Abstract
Background:Radiotherapy-related intracranial aneurysms are a recognized but rare phenomenon and often present following rupture leading to subarachnoid hemorrhage. Treatment poses a particular dilemma and both endovascular, and surgical approaches have been used with varied success. We present the case of a radiotherapy-related aneurysm treated conservatively with a favorable outcome.
Case Description:A 37-year-old man was diagnosed with a left temporal lobe mass for which he underwent an uneventful craniotomy and debulking. Histology revealed Grade III anaplastic astrocytoma following which he received radiotherapy. Three years later, he presented with subacute headache and transient dysphasia. Computed tomography and catheter angiography revealed a fusiform aneurysm of the supramarginal branch of the left middle cerebral artery with probable intra-aneurysmal thrombus. Adjacent vessels also showed mild vasculitic changes. Trial balloon occlusion of the parent vessel resulted in profound dysphasia and was therefore abandoned. Bypass surgery or stent placement was deemed to have too high a risk of neurological deficit, and keeping in mind, the diagnosis of anaplastic astrocytoma, conservative management was pursued with partial thrombosis noted on serial imaging and stable appearances subsequently at 42 months’ follow-up.
Conclusion:Conservative management can be pursued in selective cases of radiotherapy-related aneurysms, particularly if the risk of treating is too high and in the context of intracranial malignancy with limited lifespan.
Keywords: Fusiform aneurysm, intracranial aneurysm, radiotherapy
CASE REPORT
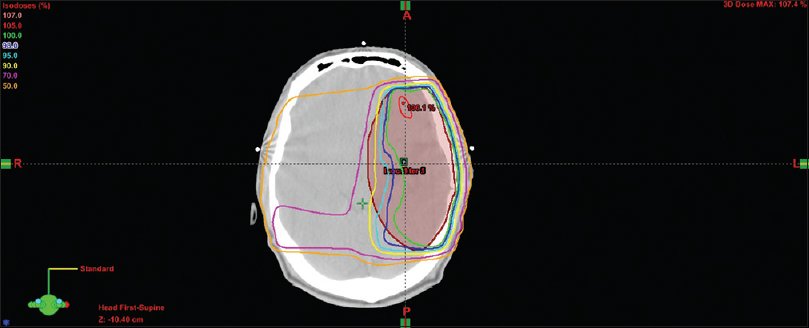
A 37-year-old man presented in April 2009 with seizures. Magnetic resonance imaging (MRI) brain showed a minimally enhancing left temporal lobe mass. He underwent left temporal craniotomy and debulking of tumor in May 2009 and made an uneventful postoperative recovery. Follow-up scans showed a significant reduction in tumor volume. Histology revealed the lesion to be a Grade III anaplastic oligoastrocytoma, and the patient subsequently underwent radiotherapy using conformal technique receiving 60 Gy in 30 fractions over 6 weeks in July 2009. This was delivered in two phases. The first phase delivered 54 Gy to the whole planning treatment volume in 27 fractions [
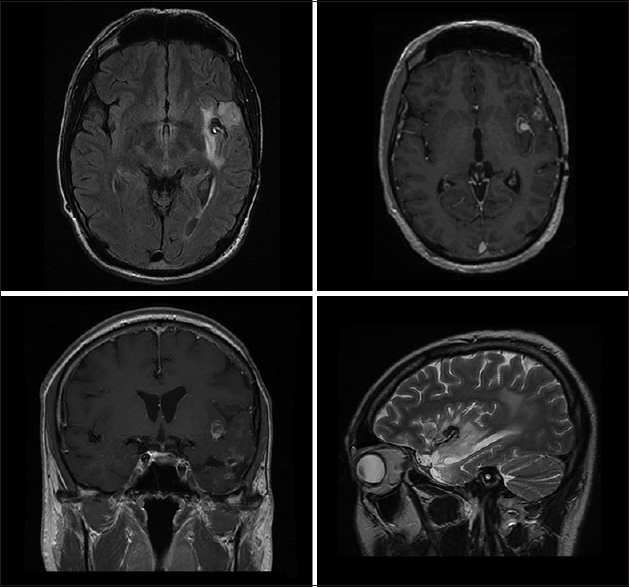
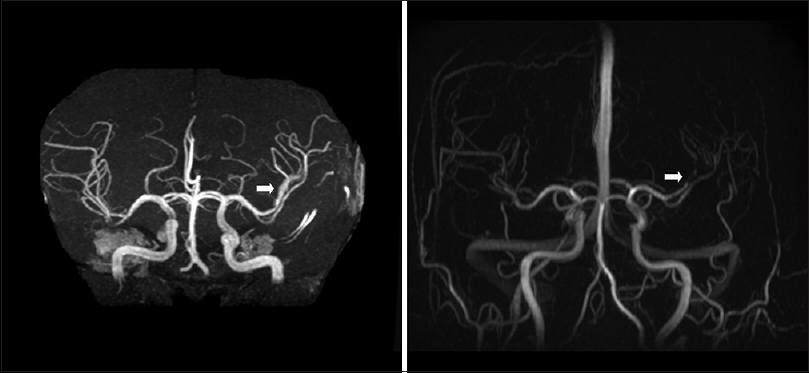
MRI in June 2011 showed a few areas of nodular enhancement within the primary tumor. This was deemed to be disease progression and chemotherapy using temozolomide was commenced. A routine follow-up MRI in April 2012 showed an entirely new area of enhancement in the left Sylvian cortex adjacent to two prominent vessels thought initially to be further tumor progression [
Figure 2
Magnetic resonance imaging brain performed a few days before aneurysm presentation. It shows small intensely enhancing area closely related to left insula showing unusual peripheral ring of enhancement (top right and bottom left) and strikingly low signal on T2-weighted imaging (bottom right). This was initially thought to be tumor progression but later retrospectively recognized as corresponding to the fusiform aneurysm
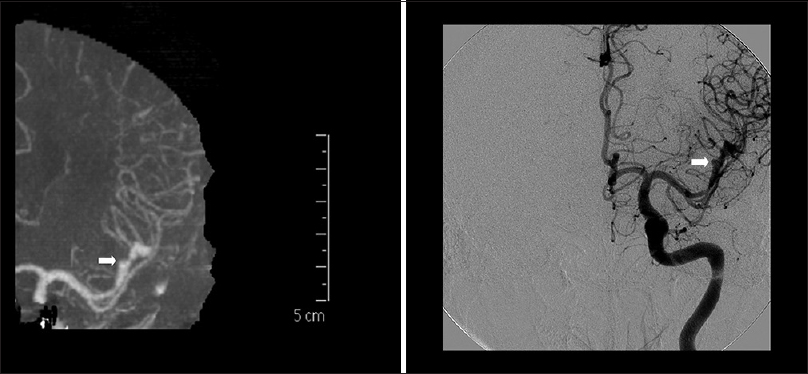
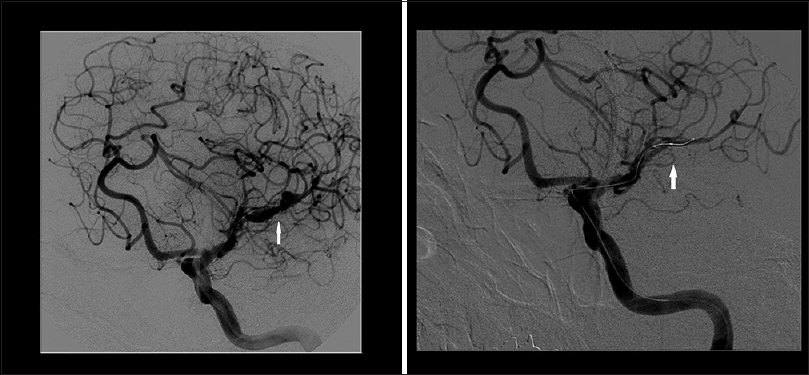
A few days after this MRI, he presented with subacute headache and acute dysphasia, the latter improving rapidly. Computed tomography (CT) brain showed a small 2 mm hyperdensity in the insular cistern corresponding to the new enhancement which had been noted on the recent MRI. CT angiography [
Figure 4
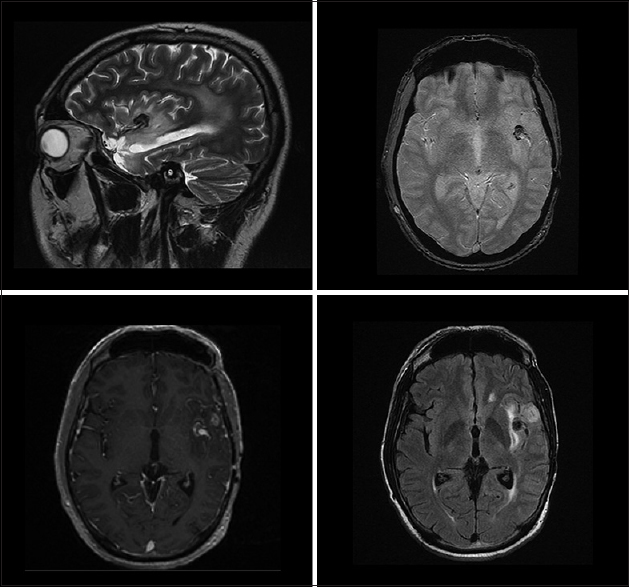
Magnetic resonance imaging brain performed after patient presented with symptoms related to the aneurysm. T2-weighted fast spin echo (top left), gradient echo (top right), T1 with gadolinium (bottom left), and axial flair (bottom right) images confirmed the fusiform aneurysm with a cap of thrombus around its distal part, likely to be either intraluminal or intramural thrombus. There was no evidence of extraluminal hemorrhage
Endovascular occlusion of the aneurysm was considered the best treatment option, provided vessel occlusion was tolerated clinically. Awake catheter angiography was performed to trial balloon occlusion. Placement of a balloon microcatheter, without inflation, into the origin of the MCA branch was sufficient to arrest flow [
Figure 5
Awake catheter angiogram/digital subtraction angiogram performed during trial balloon occlusion showing the fusiform aneurysm (left) and loss of flow in the middle cerebral artery branch when the balloon microcatheter was deployed even without inflation resulting in profound dysphasia (right)
The patient was discussed with neurovascular surgeons and interventional neuroradiologists at two other specialist centers regarding bypass, flow diverters, or stent placement. However, these were deemed to be exceptionally difficult technically with a very high risk of leaving the patient with the permanent neurological deficit. The patient's underlying diagnosis of Grade III oligoastrocytoma and the possibility of generalized vascular fragility due to radiotherapy/vasculitis also served as a detriment while considering the option of bypass or stenting. After detailed counseling, the patient also opted for conservative treatment.
MRI, 3 months later [
DISCUSSION
Aneurysm formation following radiotherapy is a rare but recognized phenomenon with the first identified radiotherapy-related intracranial aneurysm being reported in 1984.[
Radiotherapy-related aneurysms are often discovered when they rupture causing subarachnoid hemorrhage. Besides, subarachnoid hemorrhage, they can also present with nonspecific neurological symptoms, epistaxis, otorrhagia and occasionally as incidental findings.[
The pathophysiology of radiation-induced aneurysms is not fully appreciated. Acute injury associated with radiotherapy has been long recognized; however, chronic vasculopathy and aneurysm formation are poorly understood. It has been postulated that endothelial damage is most commonly responsible for these changes with capillaries and small arteries mainly affected; however, large vessel involvement has also been documented.[
In our patient, the aneurysm was deemed to be secondary to radiotherapy as the margin of surgical resection during the initial surgery did not reach the Sylvian fissure, ruling out possible vascular injury as an etiology. Furthermore, the follow-up MRI scans up to 3 years after the surgery did not reveal any abnormality, enhancement, or vascular changes in the insular region. A new area of Sylvian enhancement picked up on the MRI [
The dose of radiation given to each patient reported to have a radiotherapy-related aneurysm has been comparatively similar with most papers reporting a dose of 50–60 Gy.[
Treatment of these aneurysms poses a particular challenge and coiling, stenting, clipping, and wrapping with or without arterial bypass have all been used with varied success. It must be noted however that quite a few of the reported cases were published in the 1980s and 1990s before the recent advances in endovascular techniques. However, the perceived radiation-induced frailty of the parent vessels poses a challenge for endovascular techniques. Outcomes reported from this condition range from excellent recovery to high neurological morbidity and mortality, with the latter not uncommon.[
In our case, the patient's underlying diagnosis played a significant role in decision-making. Although Grade III oligoastrocytoma has been shown to have a better prognosis than other high-grade gliomas, reported median survival is approximately 60 months. This had an obvious impact on our choice of decision.
Our literature search revealed only one case where the aneurysm was conservatively managed with subsequent spontaneous occlusion of the vessel and no significant morbidity.[
Our case report demonstrates the treatment dilemmas associated with certain radiotherapy-related aneurysms. This is particularly relevant in the context of radiotherapy for intracranial malignancy. The vast majority of the previously reported such cases have been reported in nonmalignant conditions which had a more favorable overall long-term prognosis and therefore prompting aggressive treatment.
Some authors believe that these aneurysms are more prone to rupture than typical aneurysms. It may be the case that radiotherapy-related aneurysms are under-reported as authors may be discouraged to publish similar cases once the novelty of the condition has disappeared, and hence, one can only speculate about the true incidence and natural history.[
We demonstrate that conservative management can be considered as a feasible option for complex and difficult-to-treat aneurysms wherein the treatment is likely to be offset by a high risk of morbidity and mortality and also in the context of intracranial malignancy with limited lifespan. Serial imaging may subsequently provide clues regarding spontaneous resolution as against radiological or symptomatic progression which would then necessitate intervention.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abla AA, Lawton MT, McDermott MW. Intracranial aneurysm formation following radiation. World Neurosurg. 2014. 81: 492-3
2. Azzarelli B, Moore J, Gilmor R, Muller J, Edwards M, Mealey J. Multiple fusiform intracranial aneurysms following curative radiation therapy for suprasellar germinoma. Case report. J Neurosurg. 1984. 61: 1141-5
3. Gomori JM, Levy P, Weshler Z. Radiation-induced aneurysm of the basilar artery – A case report. Angiology. 1987. 38: 147-50
4. Huh W, Bang JS, Oh CW, Kwon OK, Hwang G. Intracranial aneurysm following cranial radiation therapy. J Cerebrovasc Endovasc Neurosurg. 2012. 14: 300-4
5. Nanney AD, El Tecle NE, El Ahmadieh TY, Daou MR, Bit Ivan EN, Marymont MH. Intracranial aneurysms in previously irradiated fields: Literature review and case report. World Neurosurg. 2014. 81: 511-9
6. Park KY, Ahn JY, Lee JW, Chang JH, Huh SK. De novo intracranial aneurysm formation after Gamma Knife radiosurgery for vestibular schwannoma. J Neurosurg. 2009. 110: 540-2
7. Sciubba DM, Gallia GL, Recinos P, Garonzik IM, Clatterbuck RE. Intracranial aneurysm following radiation therapy during childhood for a brain tumor. Case report and review of the literature. J Neurosurg. 2006. 105: S134-9
8. Yamaguchi S, Kato T, Takeda M, Ikeda H, Kitamura K. Ruptured distal anterior inferior cerebellar artery aneurysm following stereotactic irradiation for vestibular schwannoma: Case report. Neurol Med Chir (Tokyo). 2009. 49: 202-5