- Department of Neurosurgery, All India Institute of Medical Sciences, Raipur, Chhattisgarh, India.
DOI:10.25259/SNI_213_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Lokesh Suresh Nehete, Raghavendra Sharma, Prashant Raj Singh, Surendra Gupta. Rapidly growing diffuse neurofibroma of the scalp with calvarial defect in a young woman: A rare entity. 02-Oct-2020;11:313
How to cite this URL: Lokesh Suresh Nehete, Raghavendra Sharma, Prashant Raj Singh, Surendra Gupta. Rapidly growing diffuse neurofibroma of the scalp with calvarial defect in a young woman: A rare entity. 02-Oct-2020;11:313. Available from: https://surgicalneurologyint.com/surgicalint-articles/10309/
Abstract
Background: A diffuse neurofibroma, a variant of neurofibroma, most commonly occurs in young adults and involves the head and neck. In the absence of neurofibromatosis, associated calvarial defect with these swellings is rarely seen.
Case Description: An 18-year-old woman presented with a history of rapidly progressive painless large swelling over the bilateral parieto-occipital region of scalp. It was soft and boggy with brownish discoloration of overlying skin. Imaging study showed brilliantly enhancing diffuse lesion involving the bilateral parieto-occipital region of scalp and extending into the extradural region. She underwent excision of lesion. Postoperatively, she developed flap necrosis and it was allowed to heal with the secondary intention. The biopsy findings were consistent with neurofibroma. The patient is on regular follow-up, without any evidence of recurrence at 1 year.
Conclusion: Rapidly growing solitary diffuse neurofibroma is rare in children and adolescents. Preoperative diagnosis may be difficult and surgical treatment needs to be individualized. These patients need regular follow-up for early detection of recurrence.
Keywords: Diffuse neurofibroma of the scalp, Neurofibroma, calvarial defect, Reconstructive surgery, Surgical excision
INTRODUCTION
A diffuse neurofibroma, a variant of neurofibroma, most commonly occurs in young adults and involves the head and neck. Associated calvarial defect with these swellings is also rarely seen in the absence of neurofibromatosis.
We report a young woman with rapidly progressive diffuse neurofibroma of the scalp with a small calvarial defect, without any features of neurofibromatosis.
CASE REPORT
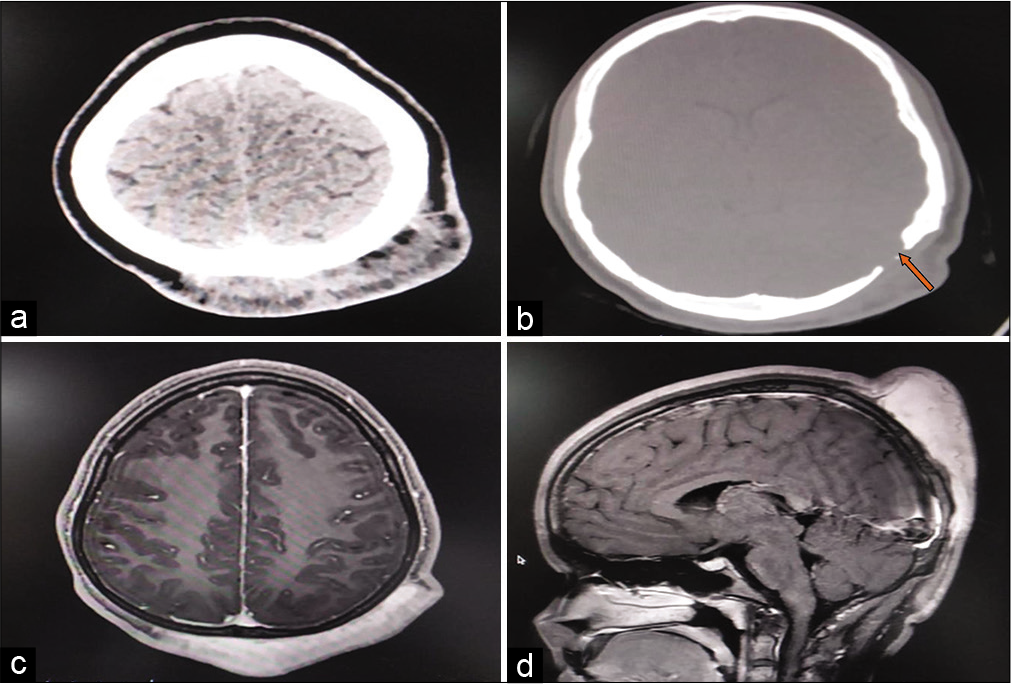
An 18-year-old woman presented with a history of painless rapidly progressive large swelling over bilateral parieto-occipital region of scalp for the past 6 months. She underwent surgery for the swelling at occipital region 5 years back, but reports of the previous treatment were not available with the patient. Local examination showed soft boggy swelling over the scalp with brownish discoloration of the overlying skin. Healed linear scar was noted near the center of the swelling [
Computed tomography scan of the head revealed a diffuse soft-tissue mass in bilateral parieto-occipital region with the left occipital bone defect near the asterion [
The patient was planned for the excision of lesion with reconstructive surgery. Due to the possibility of loss of a large area of the scalp, only surgical excision of the mass was done preserving the overlying scalp. The lesion was soft, fleshy, moderately vascular, infiltrating scalp at places but was free from pericranium. During surgery, hair follicles were also exposed at some places. Small extradural part was also present near the asterion with bony defect. The lesion was excised, with small part of infiltrating scalp was also removed, preserving the pericranium. Calvarial defect is left as such and as calvarial defect was small; no cranioplasty was performed during surgery. Scalp was closed primarily without any difficulty.
Postoperatively, the patient has developed skin flap necrosis and pus discharge from the center of the skin flap. The wound was allowed to heal by the secondary intention under appropriate antibiotics after the debridement of necrotic tissue.
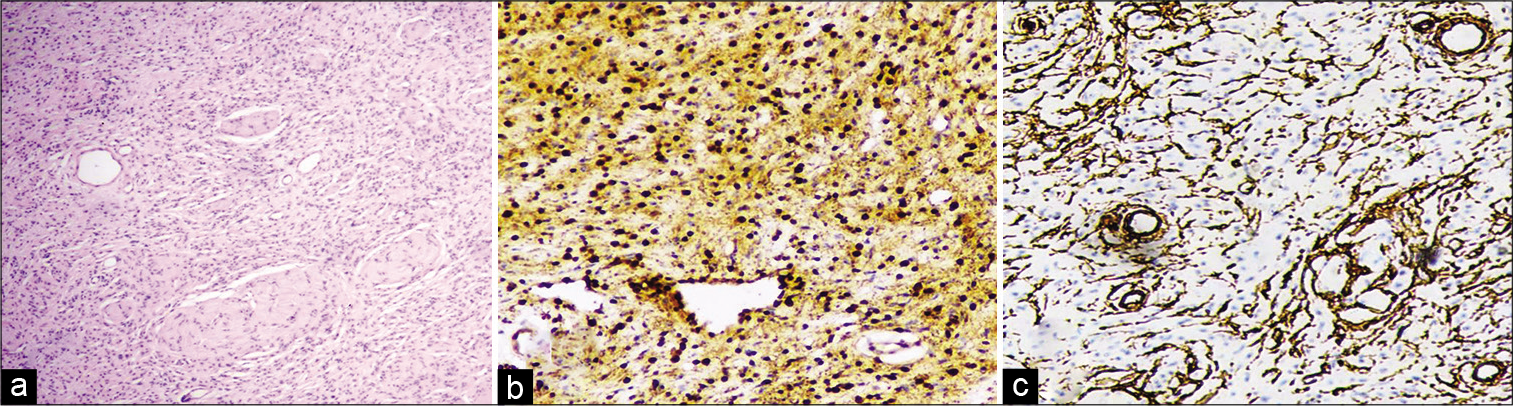
The histopathology report was consistent with neurofibroma [
Figure 3:
Photomicrograph illustrating histopathology of the lesion (a) shows irregular shaped groups of bland spindle cells with wavy nuclei and pale eosinophilic cytoplasm. There is no nuclear atypia. Mitotic activity is not appreciated (H&E, ×20), (b) diffuse positivity for S-100; (c) CD34 positivity in blood vessels only (IHC, ×200).
DISCUSSION
Diffuse neurofibroma is a rare, but distinctive variant of neurofibroma. Diffuse neurofibroma is most commonly seen in the head-and-neck regions of adolescents or young adults.[
Most reported cases in the literature are in adults age group, with a gradually progressive tumor growth over decades.[
Diffuse neurofibroma is composed of elongated, spindle-shaped cells with round or fusiform nuclei and eosinophilic cytoplasm within a loose matrix of fine fibrillar collagen. The lesion diffusely infiltrates the dermis and subcutaneous tissue. The tumor encircles the surrounding structures rather than destroying them.[
A calvarial defect is usually not associated with neurofibroma in the absence of syndromic association. Skull defect having sclerotic margins is suggestive of an underlying neurogenic tumor.[
The treatment of large neurofibroma consists of surgical excision with or without reconstructive surgery. As these lesions are highly vascular, obliteration of feeding vessels in early stages of surgery helps to minimize intraoperative bleeding. We were able to control bleeding from the lesion by the bipolar coagulation. Lin and Chen highlight the importance of hypotensive anesthesia and preliminary sutures around the lesion to control bleeding.[
Reconstruction of the defect can be done with expanded myocutaneous flaps and tissue expander[
Rapidly growing solitary diffuse neurofibroma is rare in children and adolescents. Preoperative diagnosis may be difficult and surgical treatment needs to be individualized. These patients need regular follow-up as lesion may recur even after complete excision due to the infiltrative nature of the tumor.
CONCLUSION
Rapidly growing solitary diffuse neurofibroma is rare in children and adolescents and has less propensity to involve calvarial bones. These cases need long term follow up after surgical excision for early detection of recurrence.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
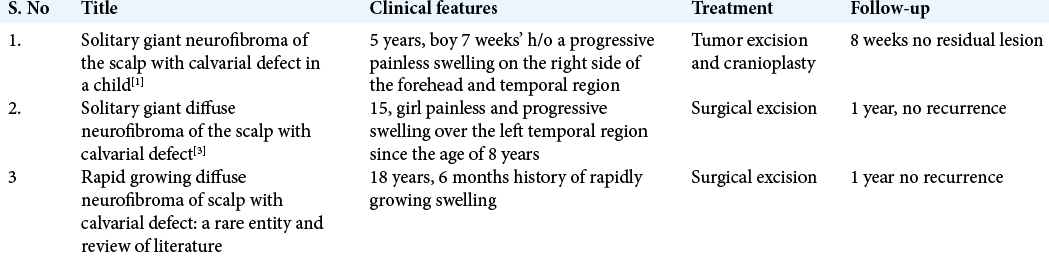
References
1. Ismail NJ, Shehu BB, Lasseini A, Hassan I, Shilong DJ, Obande JO. Solitary giant neurofibroma of the scalp with calvarial defect in a child. J Surg Tech Case Rep. 2010. 2: 24-6
2. Kareem H, Al-Rashed S, Pülhorn H. Resection of a large scalp neurofibroma using multiple overlapping string sutures to control vascularity. JPRAS Open. 2017. 13: 11-6
3. Kumar S, Chaurasia P, Singh D, Batra VV, Aher R. Solitary giant diffuse neurofibroma of the scalp with calvarial defect. Asian J Neurosurg. 2017. 12: 263-5
4. Kwak SW, Min HY, Park YS. Diffuse neurofibroma presenting with spontaneous intracranial hemorrhage. J Korean Neurosurg Soc. 2006. 39: 453-63
5. Larranaga J, Rios A, Franciosi E, Mazzaro E, Figari M. Free flap reconstruction for complex scalp and forehead defects with associated full-thickness calvarial bone resections. Craniomaxillofac Trauma Reconstr. 2012. 5: 205-12
6. Lin YC, Chen HC. Rare complication of massive hemorrhage in neurofibromatosis with arteriovenous malformation. Ann Plast Surg. 2000. 44: 221-4
7. Neelam PM, Byrapuram VN, Nimmagadda LN, Odapally SK. Diffuse neurofibroma of the scalp: A distinct histopathological entity. Int Surg J. 2015. 2: 752-5
8. Park JH, Kim JR, Shin SJ, Lee NH, Lee HS, Lim YJ. Use of tissue expansion to allow reconstruction of the back after wide resection of a diffuse neurofibroma. J Plast Surg Hand Surg. 2011. 45: 244-7
9. Tsutsumi M, Kazekawa K, Tanaka A, Ueno Y, Nomoto Y, Nii K. Rapid expansion of benign scalp neurofibroma caused by massive intratumoral hemorrhage--case report. Neurol Med Chir (Tokyo). 2002. 42: 338-40
10. Yoo KH, Kim BJ, Rho YK, Lee JW, Kim YJ, Kim MN. A case of diffuse neurofibroma of the scalp. Ann Dermatol. 2009. 21: 46-8