- Department of Neurosurgery, Hassan II Hospital, University Sidi Mohamed Ben Abdellah, Fes, Morocco
- Department of Neurosurgery, Cheikh Zaid Hospital, Rabat, Morocco
Correspondence Address:
Lakhdar Fayçal
Department of Neurosurgery, Cheikh Zaid Hospital, Rabat, Morocco
DOI:10.4103/sni.sni_21_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Lakhdar Fayçal, Bougrine Mouna, El Abbadi Najia. Rare case of conus medullaris glioblastoma multiforme in a teenager. 26-Sep-2017;8:234
How to cite this URL: Lakhdar Fayçal, Bougrine Mouna, El Abbadi Najia. Rare case of conus medullaris glioblastoma multiforme in a teenager. 26-Sep-2017;8:234. Available from: http://surgicalneurologyint.com/surgicalint-articles/rare-case-of-conus-medullaris-glioblastoma-multiforme-in-a-teenager/
Abstract
Background:Primary intramedullary spinal glioblastoma multiforme (GBM) lesions are very rare comprising only 1.5% of all spinal cord tumors. These lesions typically result in rapid neurological deterioration and are associated with a very poor prognosis.
Case Description:A 16-year-old male exhibited a slowly progressive paraparesis with urinary incontinence, ultimately resulting in paraplegia. On magnetic resonance (MR), he was diagnosed with an intramedullary GBM of the spinal cord extending from the T9 level through the conus medullaris. Ten months following decompression/partial surgical resection of the intramedullary mass, he remained paraplegic.
Conclusion:GBM of the spinal cord are rare in the pediatric age group. A 16-year-old male presented with a flaccid paraplegia attributed to an MR-documented GBM of the distal thoracic cord extending from the T9 level through the conus medullaris. Despite partial intramedullary tumor resection, 10 months postoperatively, he remained paraplegic.
Keywords: Conus medullaris, glioblastoma multiforme, intramedullary tumor, poor prognosis, radiation therapy, review of GBM, spinal cord
INTRODUCTION
Glioblastoma multiforme (GBM) rarely involves the spinal cord (1–5% of all GBM cases), and accounts for only 1.5% of all spinal cord tumors.[
At present, younger patients are optimally treated with maximal tumor removal to minimize neurological morbidity. Here, we present the case of a 16-year-old male with flaccid paraplegia attributed to magnetic resonance (MR) documented intramedullary T9-conus likely GBM. Despite partial tumor resection followed by aggressive adjunctive treatment. he remained paraplegic 10 months later.
CASE REPORT
Clinical presentation
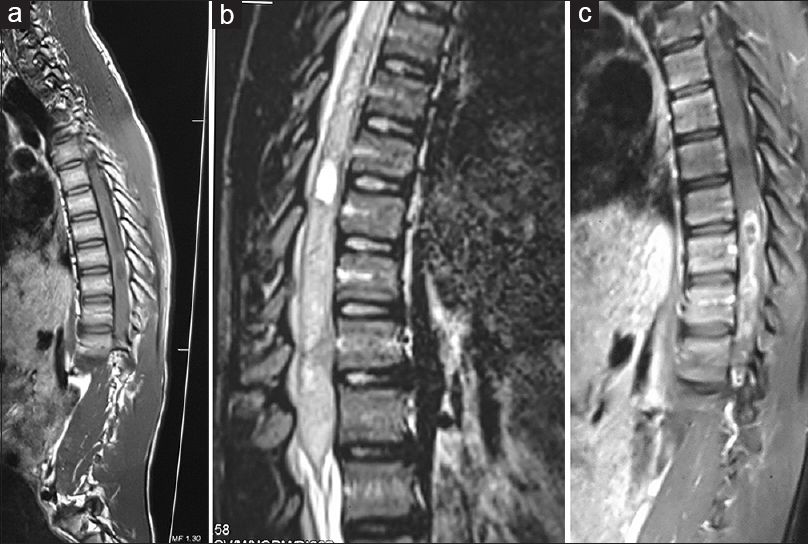
A 16-year-old male presented with a 3-week history of low back pain and a rapidly progressive sensorimotor flaccid paraplegia with urinary incontinence. Motor examination showed 1/5 strength in all distributions in the lower extremities, with a relative loss of pin appreciation below the Th10-Th11 levels. The thoracic MR showed an intramedullary, fusiform, expansile lesion extending from T9-conus. It was iso- to hypointense on T1- and hyperintense on T2-weighted MR images and heterogeneously enhanced with gadolinium [Figure
Figure 1
MRI findings: sagittal T1-weighted (a) and T2-weighted (b) and T1 post contrast (c) weighted sagittal images of a dorsal intramedullary GBM from Th9-L1. Note then large conus medullaris in a prominently widened spinal canal. Diffuse, inhomogeneous tumor enhancement and reactive cord edema were seen on the enhanced MR (c)
Histopathology
Histopathologically, the lesion was a GBM (WHO grade IV). It was characterized by hyperchromatism, pleomorphism (hematoxylin and eosin stains), atypical cells with high cellularity, vascular proliferation, and necrosis. Immunohistochemistry revealed glial fibrillary acidic protein (GFAP) and S100 protein, along with a high MIB1/Ki-67 labelling index.
Outcome
Despite surgery, conventional radiation therapy (40–50 Gy in 20–25 fractions), chemotherapy [temozolomide (TMZ)], and corticosteroids, the patient remained paraplegic at 10 postoperative months. Of interest, there has been no further tumor progression.
DISCUSSION
Clinical, diagnostic, and pathological presentation of pediatric glioblastoma multiforme
GBM involves the spinal cord in only 1–5% of all GBM cases, accounting for only 1.5% of all spinal cord tumors.[
Treatment, surgery, and chemotherapy/radiation therapy
Although surgical decompression/excision of intramedullary GBM is the treatment of choice, it is often accompanied by significantly increased morbidity and does not necessarily increase survival; therefore, some recommend biopsy alone. Although radiotherapy and adjuvant TMZ are widely used, effective results have not been documented in children whose average survival barely exceeds 6 to 16 months, with a mean survival of 12 months.[
CONCLUSION
Intramedullary GBM of the spinal cord (T9-conus) are extremely rare in the pediatric age group. Despite aggressive intramedullary tumor resection, followed by adjuvant chemotherapy and radiation therapy, the patient's ultimate long-term outcomes are minimally impacted (e.g. estimated survival at 6–16 month; mean survival of 12 months).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bonde V, Balasubramaniam S, Goel A. Glioblastoma multiforme of the conus medullaris with holocordal spread. J Clin Neurosci. 2008. 15: 6013-
2. Chiagozie O, Vivek M, Chetan B, George J. Pediatric spinal glioblastoma multiforme: Current treatment strategies and possible predictors of survival. Childs Nerv Syst. 2012. 28: 715-20
3. Cohen AR, Wisoff JH, Allen JC, Epstein F. Malignant astrocytomas of the spinal cord. J Neurosurg. 1989. 70: 50-4
4. Cohen KJ, Pollack IF, Zhou T. Temozolomide in the treatment of high-grade gliomas in children: A report from the Children's Oncology Group. Neuro Oncol. 2011. 13: 317-23
5. Morais N, Mascarenhas L, Soares-Fernandes JP, Silva A. Primary spinal glioblastoma: A case report and review of the literature. Oncol Lett. 2013. 5: 992-6
6. Mori K, Imai S, Shimizu J, Taga T, Ishida M, Matsusue Y. Spinal glioblastoma multiforme of the conus medullaris with holocordal and intracranial spread in a child: A case report and review of the literature. Spine J. 2012. 12: e1-6
7. Perkins SM, Rubin JB, Leonard JR, Smyth MD, El Naqa I, Michalski JM. Glioblastoma in children: A single-institution experience. Int J Radiat Oncol Biol Phys. 2011. 80: 1117-21
8. Scarrow AM, Rajendran P, Welch WC. Glioblastoma multiforme of the conus medullaris. Clin Neurol Neurosurg. 2000. 102: 166-7
9. Singh PK, Singh VK, Tomar J, Azam A, Gupta S, Kumar S. Spinal glioblastoma multiforme: Unusual cause of post-traumatic tetraparesis. J Spinal Cord Med. 2009. 32: 583-6
10. Stupp R, Hegi ME, Mason WP. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009. 10: 459-66