- Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita, Japan
- Department of Neurosurgery, Narita Tomisato Tokushukai Hospital, Tomisato, Japan.
Correspondence Address:
Tatsuya Tanaka, Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita, Japan.
DOI:10.25259/SNI_389_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tatsuya Tanaka1, Ren Fujiwara2, Ryohei Sashida1, Yu Hirokawa1, Tomihiro Wakamiya1, Yuhei Michiwaki1, Kazuaki Shimoji1, Eiichi Suehiro1, Keisuke Onoda1, Fumitaka Yamane1, Akira Matsuno1. Rare complication of lumboperitoneal shunt with distal catheter migration into the inguinal hernia sac in two adults: A case report. 10-Nov-2023;14:392
How to cite this URL: Tatsuya Tanaka1, Ren Fujiwara2, Ryohei Sashida1, Yu Hirokawa1, Tomihiro Wakamiya1, Yuhei Michiwaki1, Kazuaki Shimoji1, Eiichi Suehiro1, Keisuke Onoda1, Fumitaka Yamane1, Akira Matsuno1. Rare complication of lumboperitoneal shunt with distal catheter migration into the inguinal hernia sac in two adults: A case report. 10-Nov-2023;14:392. Available from: https://surgicalneurologyint.com/surgicalint-articles/12634/
Abstract
Background: Despite the proven benefits of lumboperitoneal shunt (LPS) for idiopathic normal-pressure hydrocephalus, complications such as catheter migration remain a problem. Inguinal complications of the distal catheter are rare in adults, and their management is uncertain. Herein, we present two cases of distal catheter migration into the inguinal hernia sac after LPS in adults and recommend their management.
Case Description: An 86-year-old man presented with inguinal swelling. In another 82-year-old man who did not show any improvement after LPS, shunt angiography revealed LPS dysfunction due to lumbar catheter occlusion and distal LPS catheter in the right inguinal hernia sac, and lumbar catheter reconstruction was performed. Both patients did not have any symptoms, except inguinal swelling, and were followed up. After 2 weeks and 4 days, the distal catheter moved into the peritoneal cavity.
Conclusion: Inguinal complications due to the migration of the distal catheter into the inguinal hernia sac are rare in LPS because frequent movements of the distal catheter due to trunk rotation dislodge it from the inguinal hernia sac for a short period. Urgent surgery was not recommended because the catheter was moved in a short period and the patients did not wish to undergo hernia repair.
Keywords: Adult, Catheter migration, Complication, Hernia repair, Hydrocephalus, Inguinal hernia sac, Lumboperitoneal shunt
INTRODUCTION
A recent randomized controlled trial has reported that lumboperitoneal shunt (LPS) placement can be beneficial for patients with idiopathic normal-pressure hydrocephalus (iNPH).[
Herein, we report two cases of distal catheter migration into the inguinal hernia sac after LPS in adults.
CASE DESCRIPTION
Case one
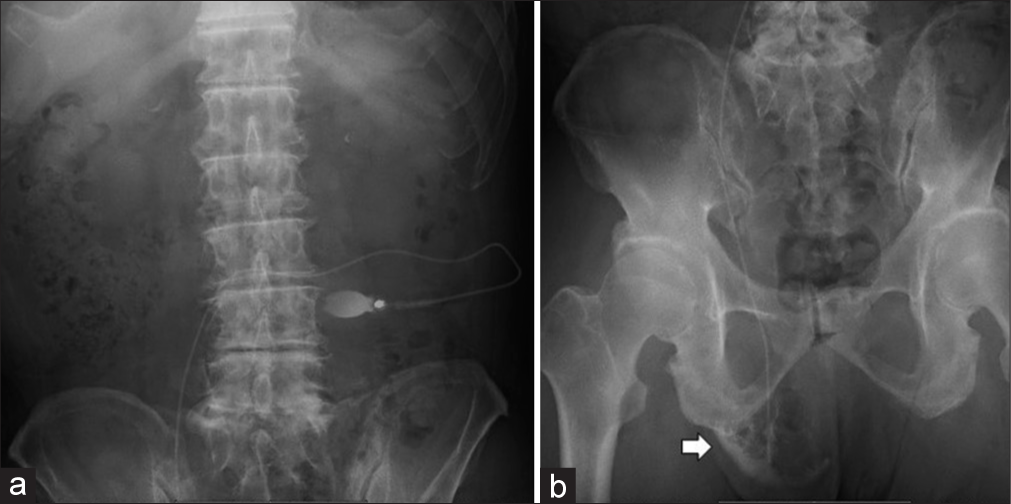
An 86-year-old man underwent LPS insertion for a confirmed diagnosis of iNPH after serial lumbar punctures and neurological assessments. No immediate complications were observed, and postoperative abdominal radiography confirmed the correct placement of the distal catheter [
Case two
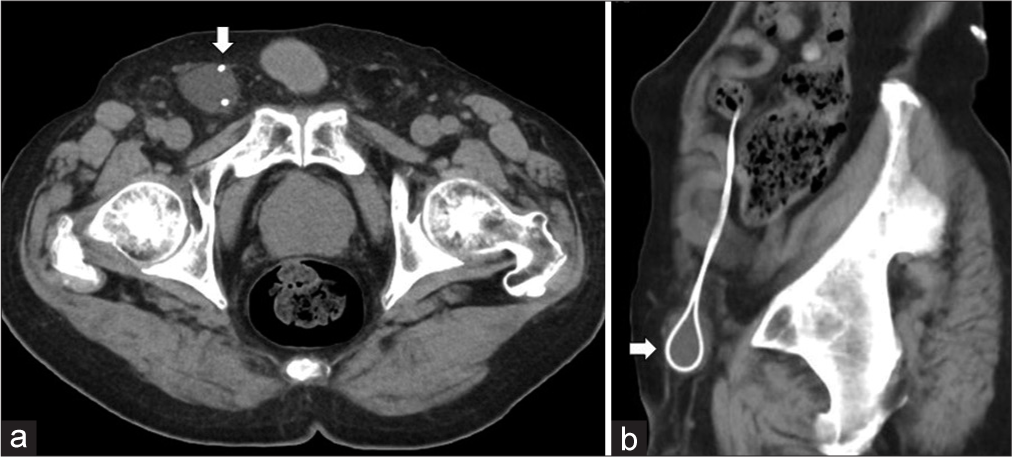
An 82-year-old man was referred to our hospital because his symptoms did not improve after LPS insertion. Head CT showed enlarged ventricles. Suspecting LPS failure, shunt angiography was performed, which showed an obstruction of the lumbar catheter and deviation of the distal catheter into the inguinal hernia sac [
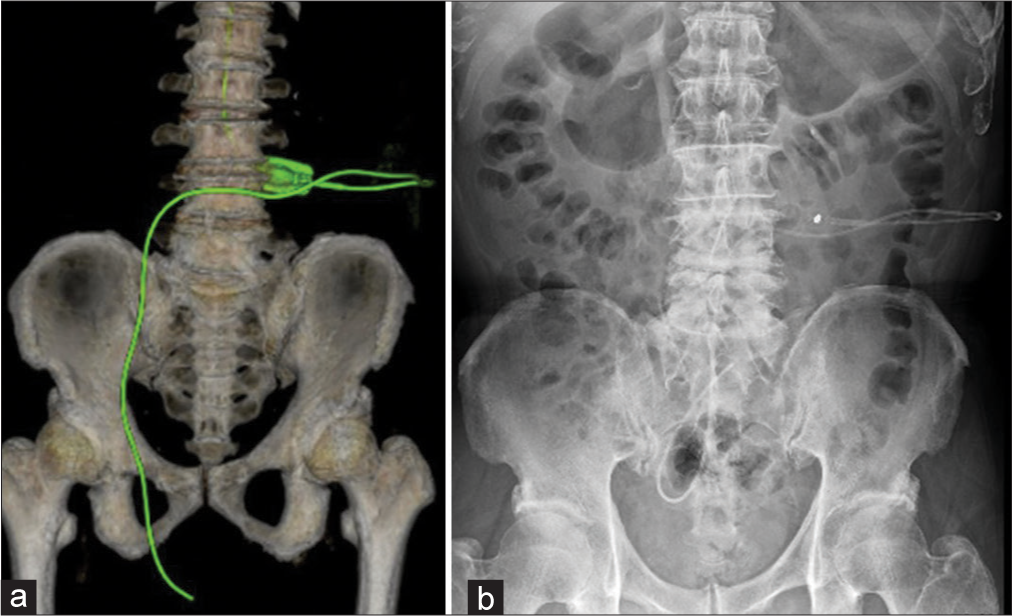
Three days later, lumbar catheter reconstruction was performed. Immediate postoperative three-dimensional CT showed a deviated abdominal catheter in the right inguinal hernia sac [
Figure 5:
(a) Three-dimensional computed tomography after lumbar catheter reconstruction showing a deviated abdominal catheter in the right inguinal hernia sac. The green structure showing the shunt system. (b) Abdominal radiography on the day after surgery showed a distal catheter in the intraperitoneal space.
DISCUSSION
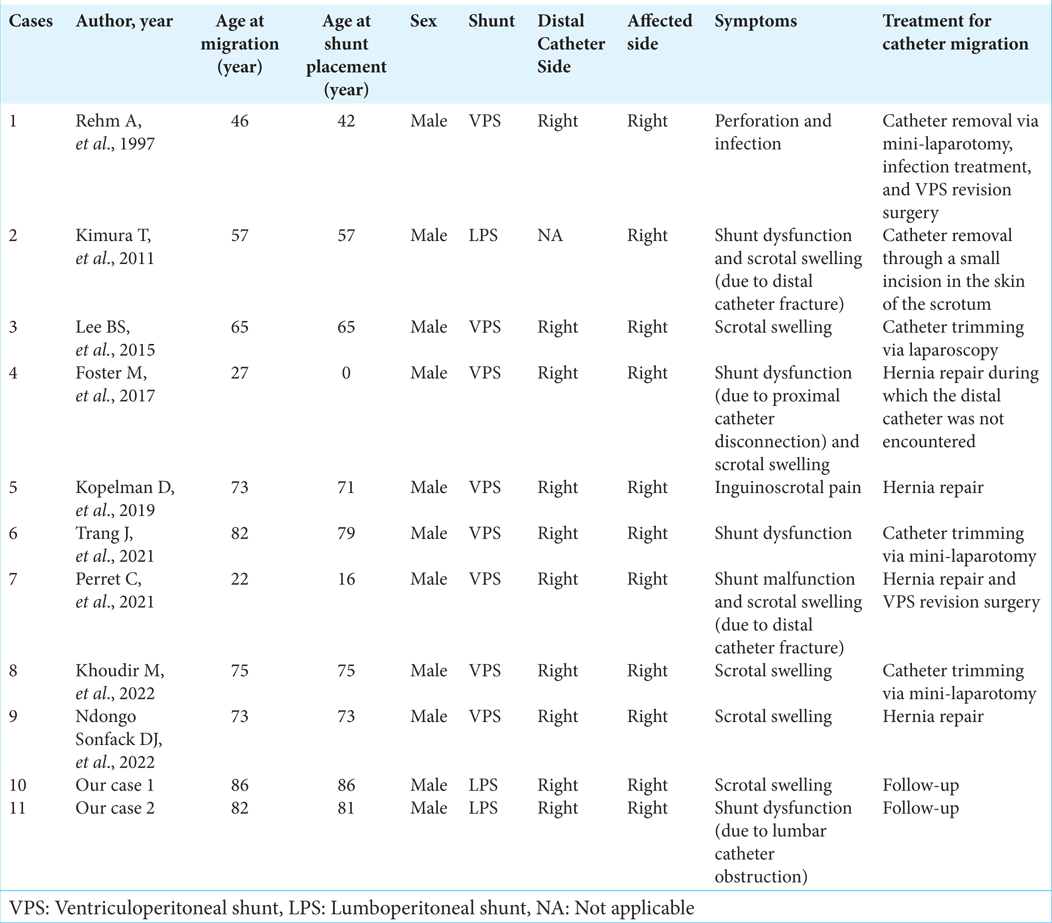
To the best of our knowledge, the migration of distal catheters into the inguinal region after VPS or LPS is more common in children and rare (nine cases only) in adults.[
Previous cases in adults are summarized in
All cases were male, and the distal side of the catheter was the affected side, except for one case in which data on the affected side were unavailable. The lifetime incidence of inguinal hernias, in which internal organs and fatty tissue protrude through the inguinal or femoral canal, is 27–43% in men and 3–6% in women.[
Symptoms included a scrotal mass, inguinal pain, intracranial hypertension due to shunt failure (e.g., headache, vomiting, and disturbed consciousness), perforation, and infection.[
In our cases, the LPS distal catheters migrated into the inguinal hernia sac without any symptoms, except groin swelling. The distal catheter was moved to the correct location during short-term follow-up without surgery.
Inguinal hernias are almost asymptomatic, and the management of inguinal hernias is surgical, regardless of whether they are symptomatic or not.[
Distal catheter migration into the abdominal wall is more common with LPS than with VPS because of more frequent movements of the distal catheter due to trunk rotation in LPS.[
Inguinal complications due to the migration of the distal catheter into the groin are rare in LPS because frequent movements of the distal catheter due to trunk rotation dislodge it from the inguinal hernia sac for a short period.
In our cases, no surgery was performed because the catheter was moved in a short period and the patients did not wish to undergo hernia repair. However, careful follow-up is necessary because the shunt always depends on the spinal fluid absorbency of the peritoneal cavity, and there is a low risk of perforation of the thin and enlarged inguinal skin.
CONCLUSION
In adults, distal catheter migration into the inguinal hernia sac is a rare complication of LPS. Inguinal complications are rare in LPS because frequent movements of the distal catheter due to trunk rotation dislodge it from the inguinal hernia sac for a short period. Urgent surgery was not recommended because the catheter was moved in a short period and the patients did not wish to undergo hernia repair.
Asymptomatic patients should be followed initially because of the risk of shunt infection owing to aggressive surgical treatment. Careful follow-up is necessary because the shunt always depends on cerebrospinal fluid absorbency of the peritoneal cavity and the risk of perforation of the thin and enlarged inguinal skin is low.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Foster M, Wilson G, Jenkinson MD, Buxton N. A rare case of ventriculoperitoneal shunt malfunction due to scrotal migration of the peritoneal catheter. Br J Neurosurg. 2019. 33: 566-7
2. HerniaSurge Gro. International guidelines for groin hernia management. Hernia. 2018. 22: 1-165
3. Kazui H, Miyajima M, Mori E, Ishikawa M, SINPHONI-2 Investigators. Lumboperitoneal shunt surgery for idiopathic normal pressure hydrocephalus (SINPHONI-2): An open-label randomised trial. Lancet Neurol. 2015. 14: 585-94
4. Khoudir M, Harris L, Toescu SM, Vaqas B. Scrotal migration of a ventriculoperitoneal shunt in an adult. A case report and literature review. Brain Spine. 2022. 2: 100898
5. Kimura T, Tsutsumi K, Morita A. Scrotal migration of lumboperitoneal shunt catheter in an adult--case report. Neurol Med Chir (Tokyo). 2011. 51: 861-2
6. Kopelman D, Shalabi F, Hatoum OA. Migration of a ventriculoperitoneal shunt into an inguinal hernia sac in an adult patient. ANZ J Surg. 2019. 89: E48
7. Lee BS, Vadera S, Gonzalez-Martinez JA. Rare complication of ventriculoperitoneal shunt, Early onset of distal catheter migration into scrotum in an adult male: Case report and literature review. Int J Surg Case Rep. 2015. 6C: 198-202
8. Miyajima M, Kazui H, Mori E, Ishikawa M. One-year outcome in patients with idiopathic normal-pressure hydrocephalus: Comparison of lumboperitoneal shunt to ventriculoperitoneal shunt. J Neurosurg. 2016. 125: 1483-92
9. Ndongo Sonfack DJ, Tarabay B, Shedid D, Yuh SJ. Unusual presentation of a common neurosurgical shunt procedure in an adult patient. SAGE Open Med Case Rep. 2022. 10: 2050313X221129770
10. Paff M, Alexandru-Abrams D, Muhonen M, Loudon W. Ventriculoperitoneal shunt complications: A review. Interdiscip Neurosurg. 2018. 13: 66-70
11. Perret C, Bertani R, Pilon B, Koester SW, Schiavini HC. Acute hydrocephalus following a spontaneous ventriculoperitoneal shunt catheter fracture with scrotal migration. Cureus. 2021. 13: e14554
12. Rehm A, Bannister CM, Victoratos G. Scrotal perforation by a ventriculoperitoneal shunt. Br J Neurosurg. 1997. 11: 443-4
13. Tanaka T, Goto H, Momozaki N, Honda E. Creating of. “fascial sheath” around subcutaneous lumboperitoneal shunt catheters largely prevents postoperative subcutaneous shunt catheter migration. Surg Neurol Int. 2022. 13: 528
14. Tanaka T, Goto H, Momozaki N, Honda E. Incidence of radiculopathy following lumboperitoneal shunt placement without fluoroscopy for normal pressure hydrocephalus. Surg Neurol Int. 2022. 13: 437
15. Trang J, McHarg D, Owler B. Migration of distal ventriculoperitoneal shunt catheter into an inguinal hernia sac in an adult patient: A case report and literature review. ANZ J Surg. 2021. 91: 2538-40