- Department of Medicine, Faculdade de Medicina do ABC, Santo André, Brazil.
- Department of Medicine, Pontifícia Universidade de São Paulo, Sorocaba, Brazil.
- Department of Molecular Biology, ABC Medical School, Santo André, Brazil.
- Department of Neurosurgery, Santa Paula Hospital, Sorocaba, Brazil.
- Department of Neurology of Pontifical Catholic University of Sao Paulo, Sorocaba, Brazil.
Correspondence Address:
Melissa Esposito Gomes Rigueiral, Department of Medicine, Faculdade de Medicina do ABC, Santo André, São Paulo, Brazil.
DOI:10.25259/SNI_330_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Melissa Esposito Gomes Rigueiral1, Fernanda Lopes Rocha Cobucci1, Pedro Henrique Simm Pires de Aguiar2, Raphael Vinicius Gonzaga Vieira4, Cesar Cozar Pacheco4, Roger Thomaz Rotta Medeiros4, Paulo Henrique Pires de Aguiar3,4,5. Rare complication of ventriculoperitoneal shunt: Ectopic distal catheter in a Grynfeltt hernia – case report. 19-Oct-2021;12:525
How to cite this URL: Melissa Esposito Gomes Rigueiral1, Fernanda Lopes Rocha Cobucci1, Pedro Henrique Simm Pires de Aguiar2, Raphael Vinicius Gonzaga Vieira4, Cesar Cozar Pacheco4, Roger Thomaz Rotta Medeiros4, Paulo Henrique Pires de Aguiar3,4,5. Rare complication of ventriculoperitoneal shunt: Ectopic distal catheter in a Grynfeltt hernia – case report. 19-Oct-2021;12:525. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11187
Abstract
Background: Ventriculoperitoneal shunts (VPSs) insertion is the most common used intervention in cases of hydrocephalus. The main postoperative complications are infections and catheter obstructions. Although the literature has well-documented cases describing migration of the distal catheter, this rare presentation can become more confusing when occurring in conjunction with some unusual preexistent morbidity in the patient, as a Grynfeltt hernia.
Case Description: This study reports a rare case of a VPS postoperative migration, in which the distal catheter exits the abdominal cavity through a Grynfeltt hernia. This condition was not discovered until the catheter fistulated through the overlying skin. The Grynfeltt hernia is the most uncommon among the lumbar ones and it’s asymptomatic in the majority of the cases, being hardly diagnosed.
Conclusion: The unusualness of the reported case deserves furthermore discussion to properly evaluate these underlying mechanisms of catheter migration.
Keywords: Catheter migration, Cerebrospinal fluid shunts, Grynfeltt hernia, Hydrocephalus, Postoperative complications, Ventriculoperitoneal shunt
INTRODUCTION
The cerebrospinal fluid (CSF) flow shunts are known as surgically implanted valvular drainage devices with the aim of directing CSF from the ventricles to the pleural cavity, the superior vein cava, and especially, the peritoneal cavity, regulating the intracranial pressure. Most distal terminations occur in the peritoneal cavity, characterizing the ventriculoperitoneal shunt (VPS).[
This procedure is usually indicated in cases of hydrocephalus and intraventricular hypertension. The VPS is composed of a system containing a proximal catheter, which is placed intraventricularly and connected to a valve, which is placed subgaleally, responsible for controlling the CSF drainage. The valve is then connected to a distal catheter that departs from the head region, crosses the thoracic region, just under the subcutaneous tissue, and reaches the peritoneal cavity, where the CSF will be absorbed.[
The most common complications in this procedure are infection (15%), obstruction and malfunction (33%), or shunt migration.[
This paper reports a rare complication, in which a VPS procedure evolved with exteriorization of the distal catheter in the thoracic-abdominal region and left flank with abscess formation in a Grynfeltt hernia found in the patient, also a very uncommon condition.
CASE REPORT
A 37-year-old male patient was diagnosed with recurrent atypical clear cell meningioma of the foramen magnum, cervical spine (C1-C2 level), and lumbar spine, confirmed by magnetic resonance imaging (MRI). The preoperative MRI also revealed hydrocephalus decurrent of the tumor compression of the fourth ventricle. The first surgery procedure was performed in late 2014 to allocate a VPS system. After 1 month, in early 2015, resection surgery of the meningioma in the foramen magnum and in the cervical spine was executed. The patient had no neurologic complications in the immediate postoperative time in any of the two occasions.
However, he returned to outpatient clinic with dizziness and headache 20 days after the last surgery. A new brain MRI was performed and exhibited the ventricular catheter outside the ventricular space. Therefore, surgery was needed to relocate another catheter. Only the intracranial catheter was replaced and reconnected with the rest of the former system, which was still functional. The symptoms resolved after the procedure and the patient was discharged without further complications. Between 2015 and 2020, he maintained in observational follow-up with MRI.
In early 2020, as the cervical intradural extramedullary tumor portion revealed relapse in the MRI, a fourth surgical procedure was required. The same occurred with no obstacles in the postoperative time. At the end of the same year, the patient developed dermal-epidermal atrophy at the thoracic-abdominal level leading to an externalization of the distal catheter, resolved only with antibiotic therapy.
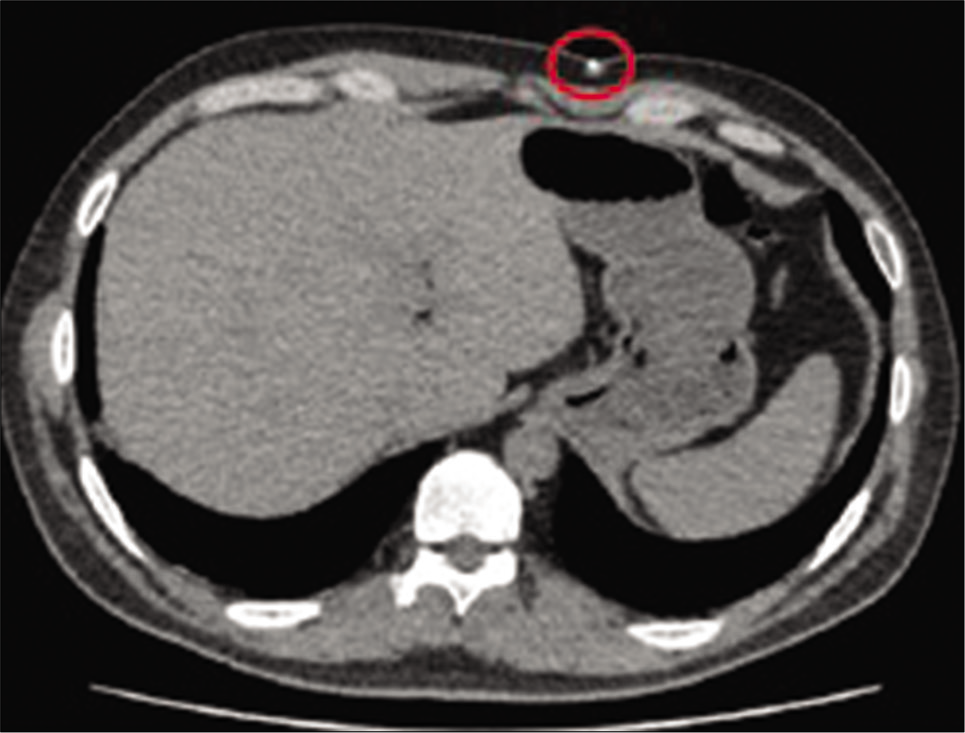
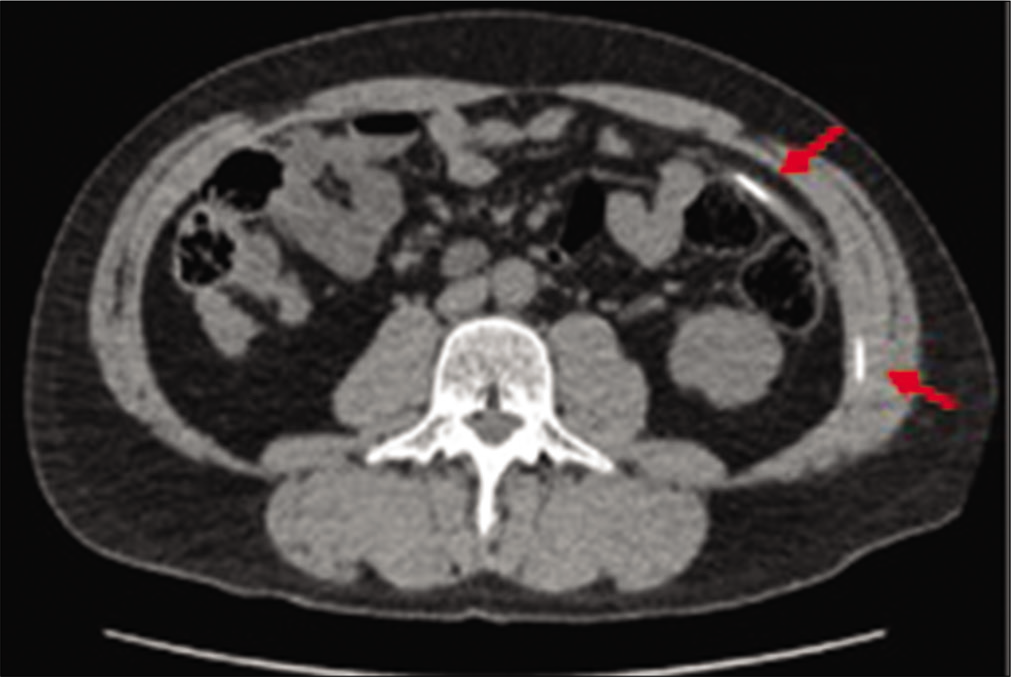
About 2 months after this incident, there was an alteration in the catheter’s trajectory, with the formation of an abscess in the left flank [
Figure 6:
Soft-tissue ultrasound image: skin and subcutaneous tissue presenting focal discontinuity of their planes, with associated inflammatory edema, forming an elongated pertum measuring about 4.2 cm depth × 0.7 cm in diameter and with apparent contiguity with the abdominal cavity. The echogenic linear image permeating the pertum may correspond to the shunt catheter with distal part subjacent to the skin.
Urgent surgery was indicated to remove the catheter and exchange it. During surgery, an attempt was made to find the tip of the catheter in the region of the left flank together with the general surgery team. The fistulous pathway was dissected, but it was not possible to identify the distal catheter. Thus, it was decided to section the catheter in the anterior thoracic region and pull the distal catheter to remove it. After removal, the proximal portion was tested with negative pressure to verify the functioning of the ventricular shunt system, however, there was no CSF drainage. Therefore, the proximal tip was closed and covered in the subcutaneous region of the anterior thorax. The abdominal region was left with a Penrose drain [
The decision of leaving the thoracic and cranial part of the VPS system was owning to an elevate risk of bleed in the entire system removal and the absence of the systemic and neurologic infectious signs. The aerobic and anaerobic cultures were negative which led to neurosurgical team to maintain the conservative conduct. The patient was kept under neurological and infectious surveillance, showing no signs of meningism. He was discharged after 5 days of hospitalization, with only a few scars in the thoracic-abdominal level [
DISCUSSION
There are several VPS complications described in the literature, which can be differentiated into mechanical and nonmechanical failures. The mechanical failures are: system obstruction, disconnection of the VPS parts and catheter migration. Among the known nonmechanical failures are usually: infections and complications in the distal compartment of the system, such as ascites, abdominal pseudocyst, herniations, intestinal obstructions, pleural effusion, in addition to other complications described in the literature, which are less frequently found.[
In the group of mechanical failures, catheter migrations are the most uncommon. This complication can be seen in both the distal and proximal parts of the device. Among the distal ones, some studies divide them into three types of occurrences: internal, external, and compound migration. Regarding internal migration, the catheter perforates the viscus without exteriorization. External migration, on the other hand, occurs when the catheter penetrates the body wall completely or subcutaneously. And finally, in compound migration, the catheter perforates the hollow organ and reaches a natural cavity in the body.[
Only one report was found in the literature about the migration of a distal catheter to the retroperitoneal region, and there was not fistulation to the external environment, which has migrated to the paraspinal muscles.[
The Grynfeltt hernia is characterized as a type of lumbar hernia that arises from a defect (acquired or congenital) in the fibromuscular fascia of the posterolateral abdominal wall, more precisely in the upper lumbar triangle (Grynfeltt space), resulting in the extrusion of intra- or extra-peritoneal organs. This group represents <1.5–2% of all abdominal wall hernias. Concerning the lumbar hernias as a whole, there are just over 300 cases in the English language medical literature.[
Delineated this outline, this case is potentially unprecedented in the literature once the catheter fistulized to the outside due to a rare preexisting Grynfeltt hernia in the patient, in addition to following a false pathway to the retroperitoneal region. Although, the specific mechanism of this unique situation has not yet been fully elucidated.
CONCLUSION
We emphasize the unusualness of the reported case, once it associates a retroperitoneal pathway poorly described in the literature with fistulization of the distal VPS catheter through a rare Grynfeltt hernia. Thus, this condition deserves furthermore discussion in the future to properly evaluate these mechanisms.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Allouh MZ, Al Barbarawi MM, Asfour HA, Said RS. Migration of the distal catheter of the ventriculoperitoneal shunt in hydrocephalus. Clin Anat. 2017. 30: 821-30
2. Çakin H, Kaplan M, Öztürk S, Kazez A. Intrathoracic migration of ventriculoperitoneal shunt through the Morgagni’s hernia in case with Down syndrome: A rare shunt complication. Neurol India. 2013. 61: 552-3
3. Ferras M, McCauley N, Stead T, Ganti L, Desai B. Ventriculoperitoneal shunts in the emergency department: A review. Cureus. 2020. 12: e6857
4. Furtado LM, da Costa Val Filho JA, Faleiro RM, Vieira JA, Dos Santos AK. Abdominal complications related to ventriculoperitoneal shunt placement: A comprehensive review of literature. Cureus. 2021. 13: e13230
5. Gatto LA, Mathias R, Tuma R, Abdalla R, de Aguiar PH. Rare complication of ventriculoperitoneal shunt: Catheter protrusion to subcutaneous tissue-case report. Surg Neurol Int. 2016. 7: S1142-6
6. Greene C, Valerie E. Retroperitoneal, paraspinal migration of distal ventriculoperitoneal shunt catheter: A peculiar complication of cerebrospinal fluid shunt. Pediatr Neurosurg. 2013. 49: 86-8
7. Handa R, Kale R, Harjai MM. Unusual complication of ventriculoperitoneal shunt: Anal extrusion. Med J Armed Forces India. 2007. 63: 82-4
8. Harischandra L, Sharma A, Chatterjee S. Shunt migration in ventriculoperitoneal shunting: Comprehensive review of literature. Neurol India. 2019. 67: 85-99
9. Juca CE, Neto AL, de Oliveira RS, Machado HR. Treatment of hydrocephalus by ventriculoperitoneal shunt: analysis of 150 consecutive cases in the Hospital of the Faculty of Medicine of Ribeirao Preto. Acta Cir Bras. 2002. 17: 59-63
10. Miyake H. Shunt devices for the treatment of adult hydrocephalus: Recent progress and characteristics. Neurol Med Chir (Tokyo). 2016. 56: 274-83
11. Navarro JN, Chaves RA, Alves TPV. Ventriculoperitoneal Shunt: Unexpected Distal Catheter Migration. 2016. 3:
12. Thor K. Lumbar hernia. Acta Chir Scand. 1985. 151: 389-90
13. Voronaya AL, Filho EL, Benayon JC, de Souza Stone AF, dos Santos Mendonça PR, da Cunha DG. Grynfelt’s hernia. Case Rep Cir. 2017. 1: 1-5