- Department of Neurosurgery, University of Louisville, Louisville, Kentucky, United States.
DOI:10.25259/SNI_98_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Zaid Aljuboori, Maxwell Boakye. Rare dorsal thoracic arachnoid web mimics spinal cord herniation on imaging. 11-Apr-2020;11:66
How to cite this URL: Zaid Aljuboori, Maxwell Boakye. Rare dorsal thoracic arachnoid web mimics spinal cord herniation on imaging. 11-Apr-2020;11:66. Available from: https://surgicalneurologyint.com/surgicalint-articles/9955/
Abstract
Background: Dorsal arachnoid webs (DAWs) are rare clinical entities that can mimic other conditions on magnetic resonance imaging (MRI). Here, we present a case of DAW that was misdiagnosed on MR as a ventral cord herniation.
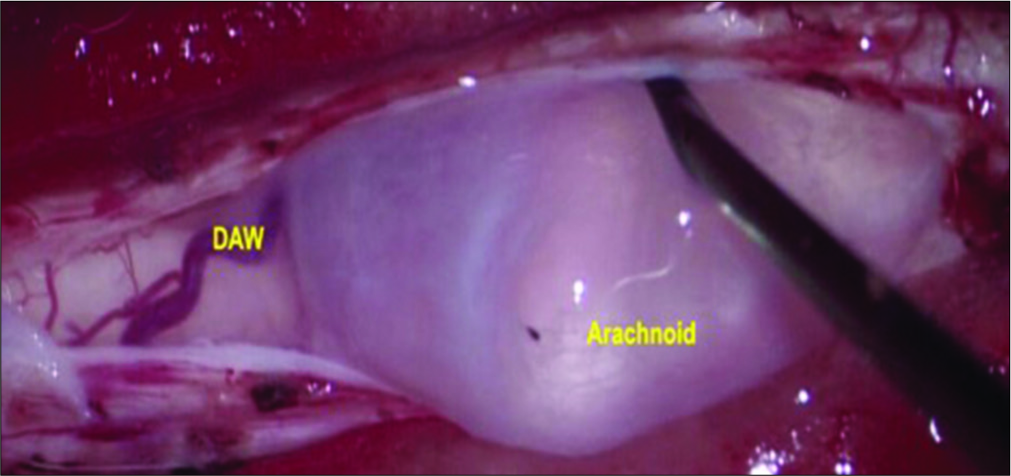
Case Description: A 35-year-old female presented with a 1-year history of lower extremity weakness and numbness. The MRI of the thoracic spine showed ventral cord displacement with syringomyelia. The computed tomography myelogram demonstrated ventral cord herniation. Intraoperatively, the patient had a dorsal thoracic web in the absence of cord herniation. Within 8 postoperative weeks, the patient had improved, and the follow-up MI showed a significant reduction in the syrinx size.
Conclusion: On MR scans, DAWs may look like ventral cord herniation. However, the positive “scalpel sign” and syrinx, the absence of an arachnoid cyst on myelography, and the findings on cine MR help differentiate DAWs from ventral cord herniation.
Keywords: Cerebrospinal fluid, Cyst, Dorsal arachnoid webs, Herniation, Magnetic resonance imaging, Spinal cord, Ventral
INTRODUCTION
Dorsal arachnoid webs (DAWs) are rare clinical entities, of unknown etiology, that usually affect the thoracic spine. In theory, they may represent the remnant lining of previously ruptured arachnoid cysts or their precursors.[
Case summary
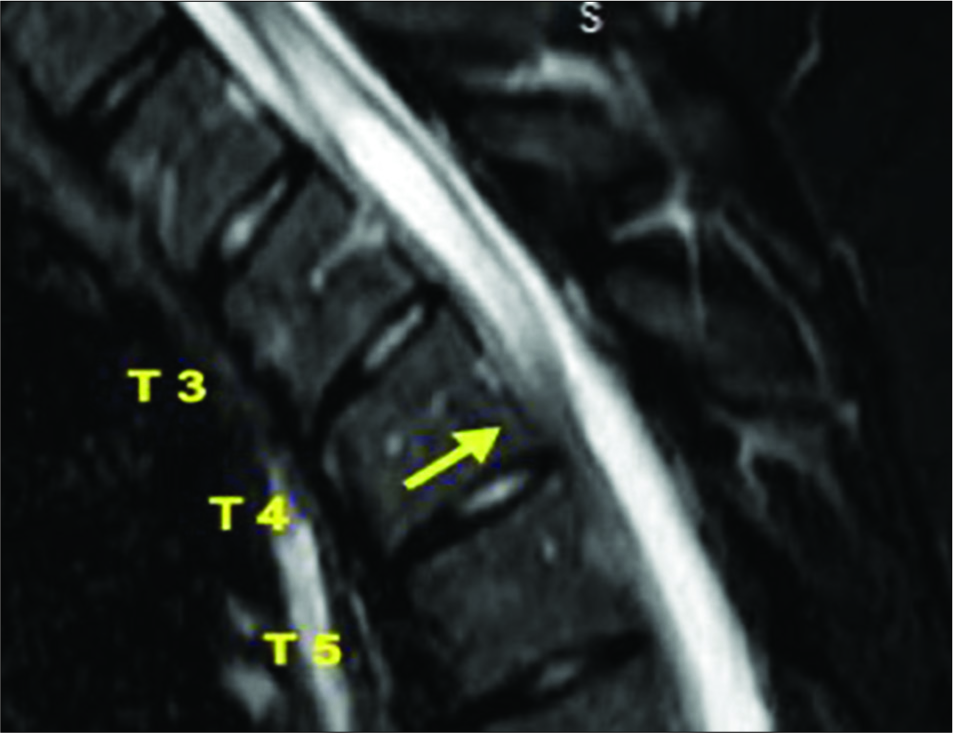
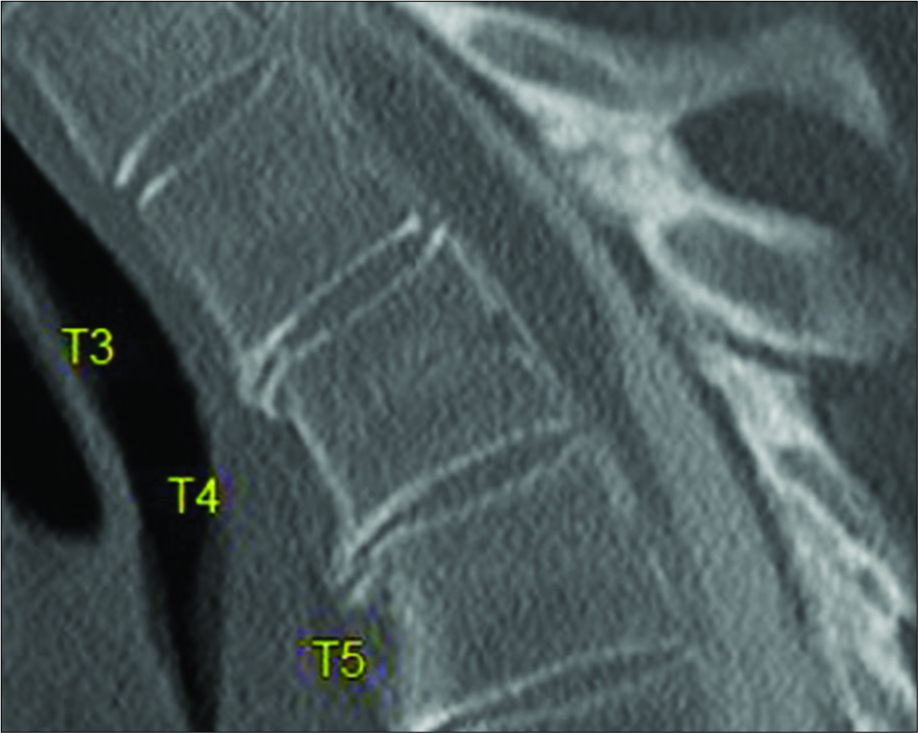
A 35-year-old female presented with a 1-year history of progressive upper back pain, bilateral lower extremity weakness, and numbness. The thoracic MRI images showed a focal area of ventral cord displacement (e.g. the “scalpel sign” at T4) and a T2-T4 syringomyelia. The CT myelogram documented a possible ventral dural defect supporting the diagnosis of ventral cord herniation [
DISCUSSION
DAWs of the spine are rare and typically contribute to progressive myelopathy.[
Magnetic resonance imaging
For DAW, SAC, and VSCH, thoracic MRI’s usually shows an enlarged dorsal subarachnoid space with ventral shifting of the spinal cord. With DAWs, there may also be accompanying attenuation of the CSF signal dorsal to the cord on T2-weighted images (e.g. CSF flow artifact). Also, a dorsal indentation of cord (e.g., the “scalpel sign”) and/ or an abnormal lesion on T-2 axial images in the dorsal subarachnoid space.[
Computed tomography myelogram
For DAW, there are no pathognomonic signs on CT myelogram.[
Combined MR and Myelo-CT in the Diagnosis of DAW, SAC, and VSCH
Combined, MR and myelo-CT studies better help differentiate DAW from SAC and VSCH. Reardon et al. indicated that the presence of the positive “scalpel sign” on MRI was highly suggestive for DAWs, as was the accompanying documentation of a syrinx.[
Here, although the MRI showed a positive “scalpel sign” consistent with a DAW, the CT myelogram was interpreted as showing a VSCH. Notably, this “misdiagnosis” could have significantly impacted surgery, as DAWs are usually approached posteriorly, while VSCH is more frequently approached anteriorly.
CONCLUSION
DAWs of the spine are rare and share similar clinical and radiographic features with SAC and VSCH. The presence of a positive “scalpel sign” and a syrinx on MRI in the absence of an arachnoid cyst on myelography is highly suggestive/ confirmatory for DAWs.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Chang HS, Nagai A, Oya S, Matsui T. Dorsal spinal arachnoid web diagnosed with the quantitative measurement of cerebrospinal fluid flow on magnetic resonance imaging. J Neurosurg Spine. 2014. 20: 227-33
2. Chellathurai A, Balasubramaniam S, Gnanasihamani S, Ramasamy S, Durairajan J. Pathophysiology and grading of the ventral displacement of dorsal spinal cord spectrum. Asian Spine J. 2018. 12: 224-31
3. Fam MD, Woodroffe RW, Helland L, Noeller J, Dahdaleh NS, Menezes AH. Spinal arachnoid cysts in adults: Diagnosis and management. A single-center experience. J Neurosurg Spine. 2018. 29: 711-9
4. Nisson PL, Hussain I, Hartl R, Kim S, Baaj AA. Arachnoid web of the spine: A systematic literature review. J Neurosurg Spine. 2019. 2019: 1-10
5. Reardon MA, Raghavan P, Carpenter-Bailey K, Mukherjee S, Smith JS, Matsumoto JA. Dorsal thoracic arachnoid web and the “scalpel sign”: A distinct clinical-radiologic entity. AJNR Am J Neuroradiol. 2013. 34: 1104-10
6. Summers JC, Balasubramani YV, Chan PC, Rosenfeld JV. Idiopathic spinal cord herniation: Clinical review and report of three cases. Asian J Neurosurg. 2013. 8: 97-105
7. Tekkok IH. Spontaneous spinal cord herniation: Case report and review of the literature. Neurosurgery. 2000. 46: 485-91
8. Yamaguchi S, Hida K, Takeda M, Mitsuhara T, Morishige M, Yamada N. Visualization of regional cerebrospinal fluid flow with a dye injection technique in focal arachnoid pathologies. J Neurosurg Spine. 2015. 22: 554-7