- Department of Neurosurgery, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, New York, United States.
- Department of Radiology, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, New York, United States.
Correspondence Address:
Elad I. Levy, Departments of Neurosurgery and Radiology, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, New York, United States.
DOI:10.25259/SNI_917_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jaims Lim1, Elizabeth Nyabuto1, Kunal Vakharia1, Elad I. Levy1,2. Rare incidence of tension pneumocephalus 2 months after repeat microvascular decompression. 28-Jun-2021;12:311
How to cite this URL: Jaims Lim1, Elizabeth Nyabuto1, Kunal Vakharia1, Elad I. Levy1,2. Rare incidence of tension pneumocephalus 2 months after repeat microvascular decompression. 28-Jun-2021;12:311. Available from: https://surgicalneurologyint.com/surgicalint-articles/10925/
Abstract
Background: Tension pneumocephalus is a rare complication after intracranial procedures and craniotomy. We report a rare case of intraventricular and subdural tension pneumocephalus occurring 2 months after repeat right-sided microvascular decompression (MVD) for recurrent trigeminal neuralgia.
Case Description: The patient in this case was a 79-year-old woman who presented with acute-onset confusion, headaches, nausea, and vomiting. On computed tomography, substantial volumes of pneumocephalus in the fourth ventricle and subdural space at the site of the retrosigmoid exposure for the previous MVD were seen. She underwent emergent wound exploration, and no obvious dural defect or exposed mastoid air cells were identified. The dura was reopened, and the surgical site was copiously irrigated. Mastoid air cells were covered with ample amounts of bone wax, and the wound was closed. The patient recovered well postoperatively with complete resolution of the pneumocephalus by her 3-month follow-up evaluation.
Conclusion: It is important to assess for cerebrospinal fluid leakage and that air cells are sealed off before wound closure to prevent a pathway for air to egress into the surgical cavity and corridor.
Keywords: Cerebrospinal fluid leak, Complication, Microvascular decompression, Pneumocephalus, Retrosigmoid craniotomy
INTRODUCTION
Tension pneumocephalus is a potentially life-threatening complication due to entrapment of air in the intracranial space that usually occurs after a traumatic injury or intracranial surgery. Patients develop hydrocephalus and increased intracranial pressure and exhibit symptoms of confusion, declined level of consciousness, and other neurological deficits.[
CASE DESCRIPTION
A 79-year-old woman with a medical history of a right cavernous carotid aneurysm treated with stent placement in 2013, an abdominal aortic aneurysm, and transient ischemic attacks initially presented to an outside clinic with severe right facial pain near the upper incisor. Aside from the facial pain, the patient was neurologically intact with no other deficits. After an extensive negative dental evaluation to exclude secondary causes of her facial pain, the patient was prescribed gabapentin by her neurologist, with no relief. After her facial pain was refractory to trials of additional agents such as benzocaine, the patient was evaluated at the neurosurgical clinic. She underwent a right MVD procedure after brain magnetic resonance imaging (MRI) revealed that the right superior cerebellar artery was adjacent and intertwined with the trigeminal nerve. The procedure was completed at our tertiary care center without any periprocedural complications, and the patient was seen at her 1-month follow-up appointment with complete resolution of her right facial pain.
Two years later, the patient represented to the neurosurgical clinic with recurrence of right trigeminal neuralgia. The pain was across the V2 and V3 distributions of the right face with associated lancinating, typical trigeminal periauricular pain triggered by talking and eating. After discussing treatment options including radiation, ablative therapies, and redo MVD, she chose to undergo repeat MVD, mainly due to the delayed effectiveness of radiation. The procedure was completed through the previous surgical corridor and was well tolerated and without periprocedural complications. At the patient’s 1-month follow-up appointment, the trigeminal neuralgia had completely resolved, but she complained of the right facial numbness that affected her ability to chew and speak. Otherwise, she was doing well overall and was carrying out her daily activities without difficulty. The patient was recommended to follow-up again in 3 months and meanwhile obtain a nutrition and speech consultation for further recommendations regarding her facial numbness.
The patient had been doing well with slow improvement in her facial numbness until 1 month after her recent follow-up visit when she acutely presented to an outside hospital emergency department with confusion, severe headaches, nausea, and vomiting. She was transferred to our center. On initial evaluation, the patient was able to report that her facial pain was almost completely resolved but complained of a severe bifrontal headache. Aside from being disoriented to place and time, the patient was neurologically intact with respect to motor and sensory function. She did not have any recent trauma or other injuries and also denied any preceding symptoms in the days before her presentation. A noncontrast computed tomography (CT) scan of the head revealed significant volumes of air intraventricularly and in the subdural space, predominantly in the infratentorial space as well as small volumes in the inferior frontal spaces [
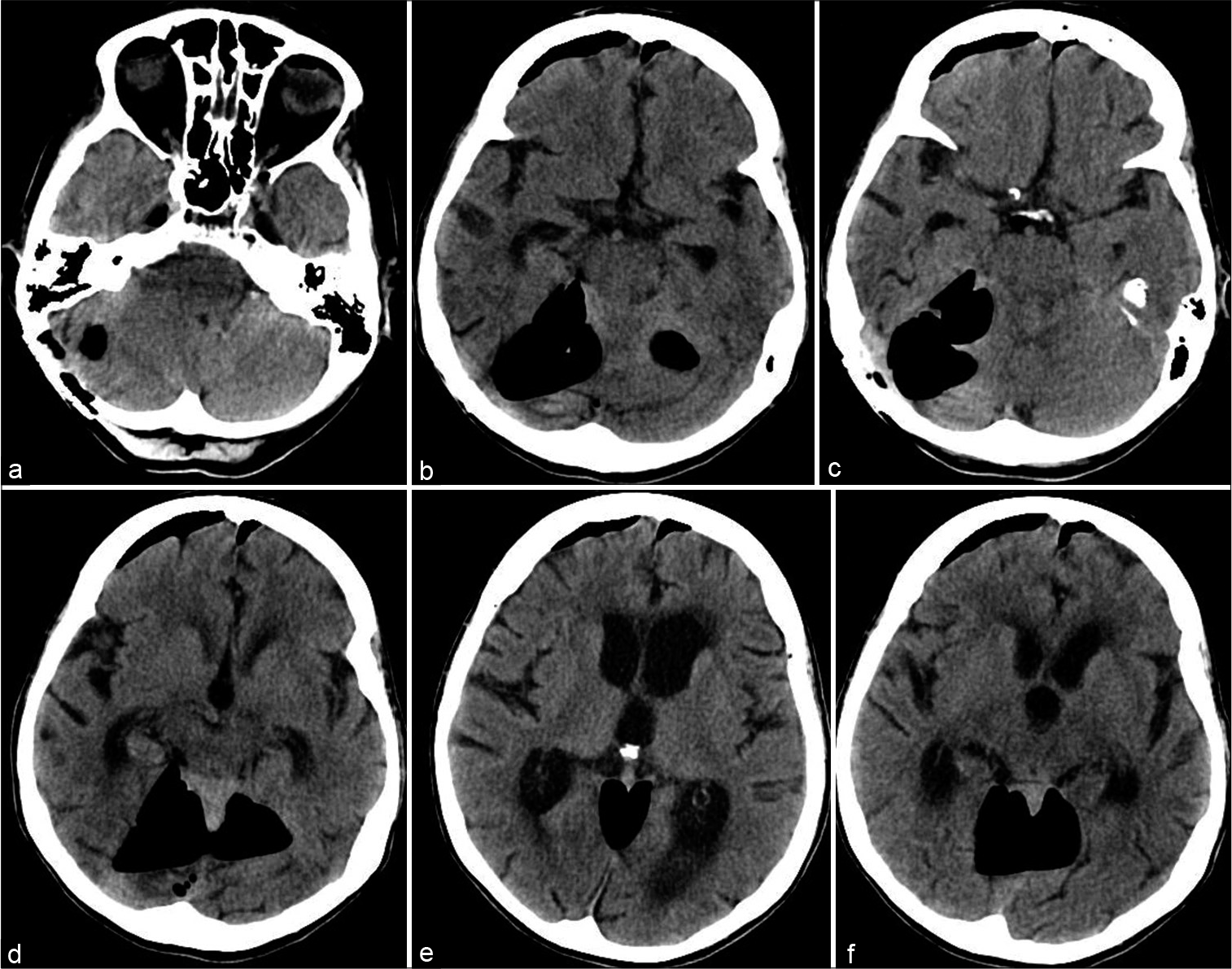
Figure 1:
Tension pneumocephalus after repeat microvascular decompression. (a-f) Respectively, caudal to rostral serial computed tomography images of the head without contrast material obtained preoperatively showing significant pneumocephalus in the posterior fossa in the previous microvascular decompression surgical corridor as well as the bilateral inferior frontal areas.
The patient was seen in clinic at the 2-week follow-up and was found to have continued residual numbness in the right face but otherwise did not have other neurological deficits. At the 3-month follow-up, brain MRI demonstrated completely resolved pneumocephalus [
Written consent was obtained from the patient and health-care proxy for all procedures. Institutional Review Board approval was deemed unnecessary.
DISCUSSION
Supratentorial craniotomies carry a very high risk of clinically insignificant pneumocephalus postoperatively.[
Our patient likely had a small amount of mastoid air cells that were exposed and not adequately covered during the initial operation and closure. This had likely provided a route for air introduction into the postoperative cavity. Although there was verification of a watertight dural closure before the titanium mesh cranioplasty, there was likely a concomitant, small, dural opening that allowed air to progressively egress into the intracranial space. Small amounts of air likely accumulated overtime until a sufficient amount had aggregated and completely occupied the entire fourth ventricular space, causing hydrocephalus to occur and resulting in the patient’s acute presentation of confusion, headaches, nausea, and vomiting. Ample rewaxing of the mastoid air cells and craniotomy boundaries sealed the exposed air cells, leading to resolution of the pneumocephalus.
CONCLUSION
Tension pneumocephalus is a rare complication that can occur after intracranial procedures and craniotomies. It is important to assess for CSF leakage and it is critical that air cells are sealed off before wound closure to prevent a pathway for air to egress into the surgical cavity and corridor.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
Potential conflicts of interest – Dr. Levy: Shareholder/ Ownership interests: NeXtGen Biologics, RAPID Medical, Claret Medical, Cognition Medical, Imperative Care (formerly the Stroke Project), Rebound Therapeutics, StimMed, Three Rivers Medical; National Principal Investigator/Steering Committees: Medtronic (merged with Covidien Neurovascular) SWIFT Prime and SWIFT Direct Trials; Honoraria: Medtronic (training and lectures); Consultant: Claret Medical, GLG Consulting, Guidepoint Global, Imperative Care, Medtronic, Rebound, StimMed; Advisory Board: Stryker (AIS Clinical Advisory Board), NeXtGen Biologics, MEDX, Cognition Medical, Endostream Medical; Site Principal Investigator: CONFIDENCE study (MicroVention), STRATIS Study – Sub I (Medtronic).
References
1. Gal TJ, Bartels LJ. Use of bone wax in the prevention of cerebrospinal fluid fistula in acoustic neuroma surgery. Laryngoscope. 1999. 109: 167-9
2. Reasoner DK, Todd MM, Scamman FL, Warner DS. The incidence of pneumocephalus after supratentorial craniotomy. Observations on the disappearance of intracranial air. Anesthesiology. 1994. 80: 1008-12
3. Steele WJ, Barber SM, Lee AG, West GA. Isolated, transient, pneumocephalus-induced oculomotor neuropathy after microvascular decompression of the trigeminal nerve. World Neurosurg. 2016. 88: 690.e17-22
4. Young M, Putty M, Schaible K. Spontaneous intraventricular tension pneumocephalus: Case report and review of the literature. World Neurosurg. 2018. 114: 317-22