Recanalization for straight sinus thrombosis through combined mechanical thrombectomy: A case report
- Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita Hospital, Narita City, Chiba, Japan.
Correspondence Address:
Yuhei Michiwaki, Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita Hospital, Narita City, Chiba, Japan.
DOI:10.25259/SNI_535_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yuhei Michiwaki, Fumitaka Yamane, Tatsuya Tanaka, Ryohei Sashida, Ren Fujiwara, Tomihiro Wakamiya, Kazuaki Shimoji, Eiichi Suehiro, Keisuke Onoda, Masatou Kawashima, Akira Matsuno. Recanalization for straight sinus thrombosis through combined mechanical thrombectomy: A case report. 08-Jul-2022;13:293
How to cite this URL: Yuhei Michiwaki, Fumitaka Yamane, Tatsuya Tanaka, Ryohei Sashida, Ren Fujiwara, Tomihiro Wakamiya, Kazuaki Shimoji, Eiichi Suehiro, Keisuke Onoda, Masatou Kawashima, Akira Matsuno. Recanalization for straight sinus thrombosis through combined mechanical thrombectomy: A case report. 08-Jul-2022;13:293. Available from: https://surgicalneurologyint.com/surgicalint-articles/11707/
Abstract
Background: Systemic anticoagulation has been the standard treatment for cerebral venous sinus thrombosis (CVT). Although endovascular treatments, including mechanical thrombectomy (MT), have been reported to be effective for CVT, no clear evidence has been established.
Case Description: A 51-year-old woman who had been administered oral contraceptive pills was transferred to our hospital with altered consciousness and disorientation. Computed tomography (CT) revealed a hyperdense signal in the straight sinus (StS), and CT angiography revealed a defect in the basal vein and StS, leading to a diagnosis of StS thrombosis. Although systemic anticoagulation through unfractionated heparin was performed, her neurological condition deteriorated, and venous ischemia was observed on CT the next day. She then underwent MT. Partial recanalization was achieved with an aspiration catheter and a stent retriever. Her neurological condition improved tremendously, and venous ischemia was reversed following MT. She was discharged 3 weeks later without neurological deficits with oral anticoagulant.
Conclusion: This was a relatively rare case with CVT confined to StS. Immediate combined MT for StS thrombosis can improve venous circulation, make the venous ischemia reversible, and improve patient outcomes, even if it results in partial recanalization.
Keywords: Case report, Mechanical thrombectomy, Recanalization, Sinus thrombosis, Straight sinus
INTRODUCTION
Cerebral venous sinus thrombosis (CVT), a rare cause of stroke, is mainly induced by oral contraceptive pills, pregnancy or puerperium, iron deficiency, infection, trauma, and potential hypercoagulable status, and has a risk of death or dependence.[
This report presents the case of a patient with straight sinus (StS) thrombosis treated with MT through the combined use of an aspiration catheter and a stent retriever. Following partial recanalization through MT, neurological conditions improved tremendously, and venous ischemia was reversed. This report suggests that immediate MT for StS thrombosis is effective even if it results in partial recanalization.
CASE DESCRIPTION
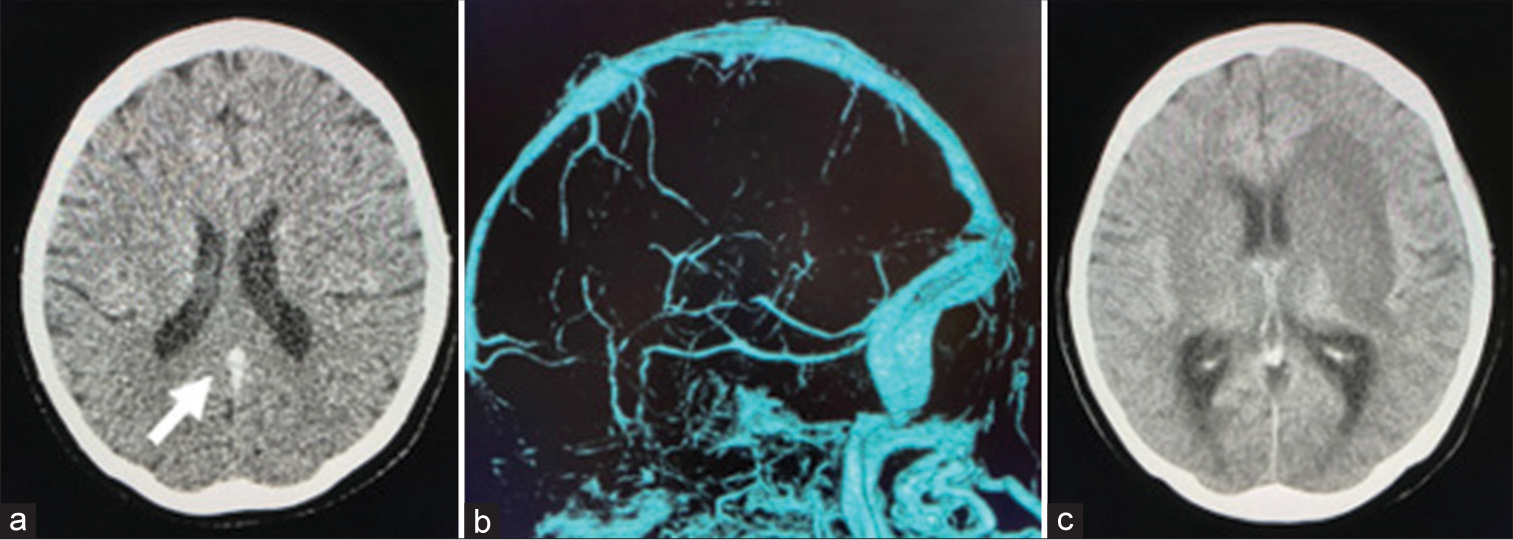
A 51-year-old woman who had been administered oral contraceptive pills for menstrual pain was transferred to our hospital because of altered consciousness, disorientation, and urinary incontinence. Her initial Glasgow Coma Scale (GCS) score was 14 (E4V4M6) on admission. Plain computed tomography (CT) showed a hyperdense signal at StS [
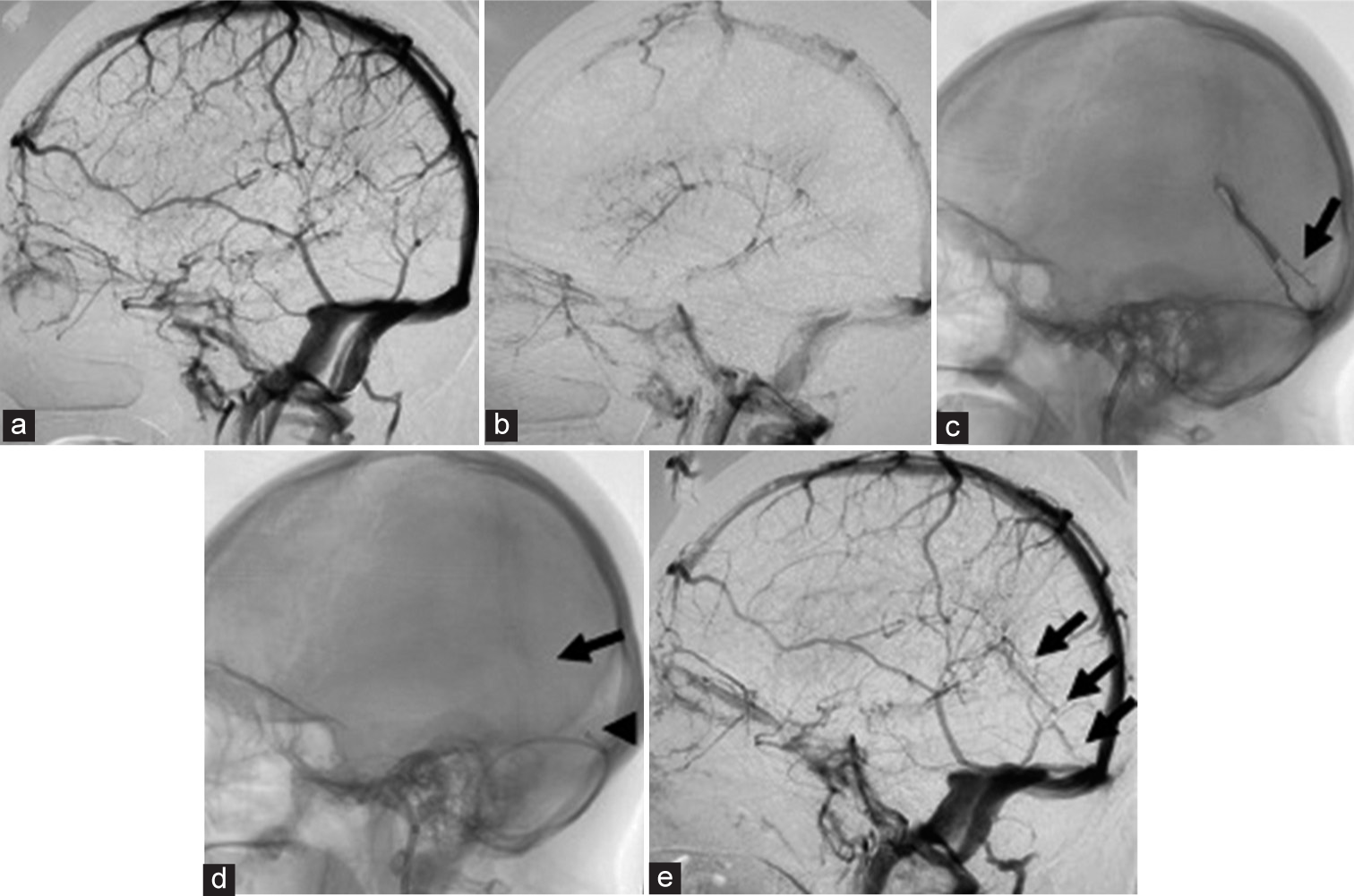
MT was performed under local anesthesia with sedation. A 6Fr guide sheath was inserted into the right femoral vein and positioned in the left jugular vein, and a 4Fr diagnostic catheter was inserted into the left femoral artery and positioned in the left internal carotid artery. Bilateral carotid and vertebral angiograms demonstrated venous flow defects in the BVR and StS [
Figure 2:
(a) Carotid artery angiogram (CAG) revealing venous flow defect of the basal vein and straight sinus (StS). (b) Late venous phase of CAG demonstrating deep venous congestion. (c) Venography from StS revealing a filling defect of the StS near the confluence (arrow). (d) Mechanical thrombectomy through combined use of an aspiration catheter (arrowhead) and stent retriever (arrow). (e) Postthrombectomy CAG revealing partial recanalization of the StS (arrow).
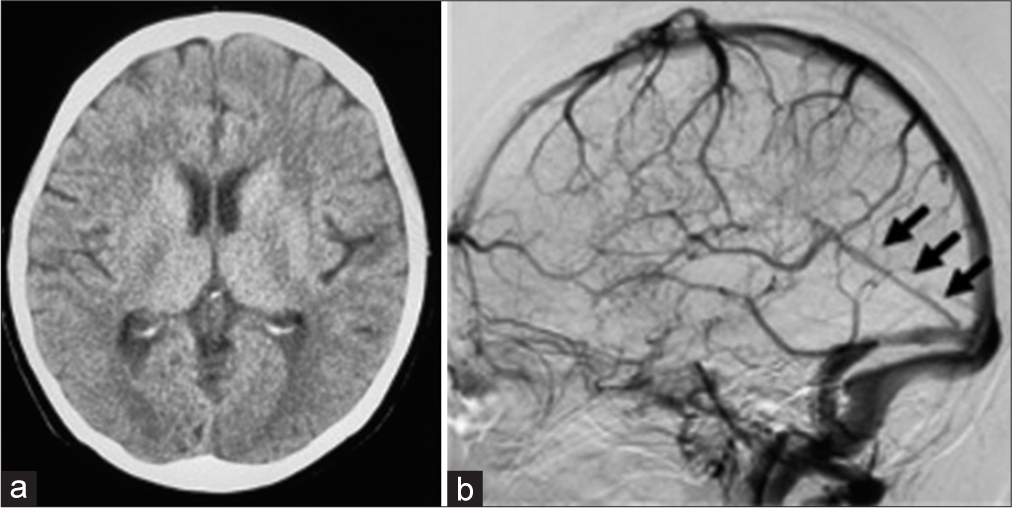
After MT, unfractionated heparin (dose: 10,000–20,000 units per day) therapy was continued for 1 week followed by oral anticoagulation medication. Her consciousness level improved tremendously (GCS: 15) the day after MT. Neuroimaging performed 2 weeks after MT demonstrated improvement of venous ischemia [
DISCUSSION
According to the International Study on Cerebral Venous and Dural Sinus Thrombosis (ISCVT), CVT has a 4.3% risk of death and an 18.9% risk of dependence.[
The standard treatment for CVT is systemic anticoagulation,[
This case report provides two important findings. First, MT through a combination technique using an aspiration catheter and stent retriever was effective for the recanalization of relatively rare StS thrombosis. Second, even partial recanalization of the occluded StS could improve cerebral venous circulation and patient outcomes if complete recanalization was not achieved.
Combined MT through an aspiration catheter and stent retriever, which was performed in the present case, has been reported as an effective strategy for CVT in some studies.[
Some systematic reviews reported high complete recanalization rates of 74% and 69%,[
The present patient did not undergo ET because significant recanalization was achieved with MT alone. However, there is a lack of consensus regarding the efficacy and safety of ET for CVT. The previous systematic reviews reported high complete recanalization rates, including cases of ET for CVT, at approximately 71% and 88%.[
The major reason for the favorable outcome in the present case was the immediate decision to perform MT and successful recanalization without complications reversing the venous ischemia.
CONCLUSION
Immediate combined MT for patients with StS thrombosis who deteriorate despite anticoagulation is an effective treatment option that provides favorable outcomes, even if it results in partial recanalization.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
References
1. Canhão P, Falcão F, Ferro JM. Thrombolytics for cerebral sinus thrombosis: A systematic review. Cerebrovasc Dis. 2003. 15: 159-66
2. Coutinho JM, Zuurbier SM, Bousser MG, Ji X, Canhão P, Roos YB. Effect of endovascular treatment with medical management vs standard care on severe cerebral venous thrombosis: The TO-ACT randomized clinical trial. JAMA Neurol. 2020. 77: 966-73
3. de Bruin S, de Haan R, Stam J. Clinical features and prognostic factors of cerebral venous sinus thrombosis in a prospective series of 59 patients. J Neurol Neurosurg Psychiatry. 2001. 70: 105-8
4. Ferro JM, Bousser MG, Canhão P, Coutinho JM, Crassard I, Dentali F. European stroke organization guideline for the diagnosis and treatment of cerebral venous thrombosis endorsed by the European academy of neurology. Eur J Neurol. 2017. 24: 1203-13
5. Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F, ISCVT Investigators. Prognosis of cerebral vein and dural sinus thrombosis results of the international study on cerebral vein and Dural Sinus thrombosis (ISCVT). Stroke. 2004. 35: 664-70
6. Girot M, Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F. Predictors of outcome in patients with cerebral venous thrombosis and intracerebral hemorrhage. Stroke. 2007. 38: 337-42
7. Ilyas A, Chen CJ, Raper DM, Ding D, Buell T, Mastorakos P. Endovascular mechanical thrombectomy for cerebral venous sinus thrombosis: A systematic review. J Neurointerv Surg. 2017. 9: 1086-92
8. Lee SK, Mokin M, Hetts SW, Fifi JT, Bousser MG, Fraser JF. Current endovascular strategies for cerebral venous thrombosis: Report of the SNIS standards and guidelines committee. J Neurointerv Surg. 2018. 10: 803-10
9. Li X, Li T, Fan Y. Efficacy of intravascular mechanical thrombectomy combined with thrombolysis and anticoagulant therapy in the treatment of cerebral venous sinus thrombosis and its effect on neurological function and coagulation indices. Am J Transl Res. 2021. 13: 6921-8
10. Mascitelli JR, Pain M, Zarzour HK, Baxter P, Ghatan S, Mocco J. Sinus thrombectomy for purulent cerebral venous sinus thrombosis utilizing a novel combination of the Trevo stent retriever and the Penumbra ACE aspiration catheter: The stent anchor with mobile aspiration technique. J Neurointerv Surg. 2016. 8: e24
11. Raychev R, Tateshima S, Rastogi S, Balgude A, Yafeh B, Saver JL. Successful treatment of extensive cerebral venous sinus thrombosis using a combined approach with Penumbra aspiration system and Solitaire FR retrieval device. J Neurointerv Surg. 2014. 6: e32
12. Salottolo K, Wagner J, Frei DF, Loy D, Bellon RJ, McCarthy K. Epidemiology, endovascular treatment, and prognosis of cerebral venous thrombosis: US Center Study of 152 Patients. J Am Heart Assoc. 2017. 6: e005480
13. Saposnik G, Barinagarrementeria F, Brown RD, Bushnell CD, Cucchiara B, Cushman M. Diagnosis and management of cerebral venous thrombosis: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011. 42: 1158-92
14. Shaikh H, Pukenas BA, McIntosh A, Licht D, Hurst RW. Combined use of Solitaire FR and Penumbra devices for endovascular treatment of cerebral venous sinus thrombosis in a child. J Neurointerv Surg. 2015. 7: e10
15. Siddiqui FM, Banerjee C, Zuurbier SM, Hao Q, Ahn C, Pride GL. Mechanical thrombectomy versus intrasinus thrombolysis for cerebral venous sinus thrombolysis: A non-randomized comparison. Interv Neuroradiol. 2014. 20: 336-44
16. Siddiqui FM, Dandapat S, Banerjee C, Zuurbier SM, Johnson M, Stam J. Mechanical thrombectomy in cerebral venous thrombosis: Systematic review of 185 cases. Stroke. 2015. 46: 1263-8
17. Styczen H, Tsogkas I, Liman J, Maus V, Psychogios MN. Endovascular mechanical thrombectomy for cerebral venous sinus thrombosis: A single-center experience. World Neurosurg. 2019. 127: e1097-103
18. Taniguchi S, Harada K, Kajihara M, Fukuyama K. Combined use of stent-retriever and aspiration thrombectomy for cerebral venous sinus thrombosis involving the straight sinus: A case report. Interv Neuroradiol. 2017. 23: 605-8