- School of Medical Sciences, University of Manchester, Manchester, United Kingdom.
- Department of Neurosurgery, Salford Royal Foundation Trust, Salford, United Kingdom.
Correspondence Address:
Savan Shah, School of Medical Sciences, University of Manchester, Manchester, United Kingdom.
DOI:10.25259/SNI_467_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Savan Shah1, K. Joshi George2. Recommencement of anticoagulation/antiplatelet therapy following non-operative management of a Chronic Subdural Hematoma – Is there an optimal time frame?. 06-Sep-2021;12:456
How to cite this URL: Savan Shah1, K. Joshi George2. Recommencement of anticoagulation/antiplatelet therapy following non-operative management of a Chronic Subdural Hematoma – Is there an optimal time frame?. 06-Sep-2021;12:456. Available from: https://surgicalneurologyint.com/surgicalint-articles/11085/
Abstract
Background: There is no consensus among clinicians regarding recommencement of antithrombotic agents following conservative management of a Chronic Subdural Hematoma (cSDH). Thus, the primary objective of this study was to determine the most commonly recommended interval and whether the data reveal a general consensus that should be adopted.
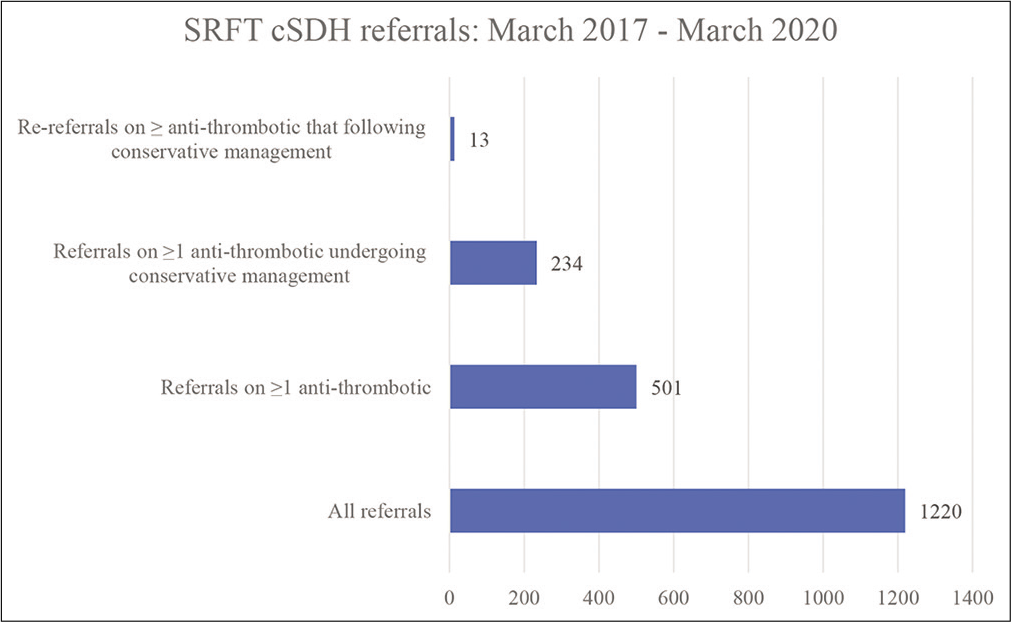
Methods: A retrospective analysis of Salford Royal Foundation Trust’s Neurosurgical referral database for patients referred with a cSDH between March 2017 and March 2020 was carried out. Patients were sorted by whether they were on blood-thinning medications.
Results: Over the 3-year period, there were a total of 1220 referral and 1099 patients. 502 (41.14%) of these referrals and 479 (43.59%) patients were on one more blood thinning agent. Of these patients 221 (46.13%) conservative management, there was a clear male predominance (M: F ≈ 2.5:1) in this cohort. 2 weeks was the most commonly advised time-frame (n = 76, 36.36%) to withhold. Of the 234 referrals, there were 13 (5.88%) re-referrals in total. Crucially, there was no significant difference in reaccumulation rates between patients asked to withhold their blood thinners for 2 weeks versus those asked to stop for longer than 2 weeks (P = 0.57).
Conclusion: For the majority of bleeds, there is no clear benefit from asking patients to withhold their anticoagulant/antiplatelet for longer than 2 weeks. In cases, where it is deemed appropriate to stop for longer than 2 weeks, clear instructions should be provided and documented along with reasons behind the decision.
Keywords: Anticoagulation, Antiplatelet, Chronic subdural haematoma, Reaccumulation
INTRODUCTION
A chronic subdural hematoma describes a collection of old blood between the dura and arachnoid mater of the meninges due to a disruption of the bridging veins. It most often occurs secondary to minor head trauma and is primarily a pathology of the elderly, with an overall incidence of 17.6/100,000 of the population per year. This figure is constantly rising both overall, and in the elderly demographic.[
Surgical evacuation forms the cornerstone of management in the majority of patients, with burr-hole drainage opted for most commonly. As such, the majority of literature exploring the point at which anti-thrombotics should be restarted following a cSDH focuses on this population of patients[
Although the advised time interval is often arbitrarily selected, there are certain factors that are generally accounted for in the decision-making process. For instance, the size of the bleed is a key influence, with larger bleeds intuitively requiring longer periods off blood thinner’s than smaller ones. The original reason for anticoagulant (AC)/antiplatelet (AP) is another important aspect that must be accounted for. For instance, it is of greater importance for a patient with a mechanical heart valve to be restarted on their warfarin than a patient on Aspirin for primary prevention of a stroke. Finally, a prior history of trauma and if the patient’s INR was above the intended therapeutic range are also considerations which influence the final decision.
MATERIALS AND METHODS
Data collection
Salford Royal Foundation Trust’s (SRFT’s) provides neurosurgery services for the Greater Manchester region and is one of the largest neurosurgical centers in the United Kingdom. Accordingly, SRFT’s neurosurgical referral database from March 2017 to March 2020 formed the basis of data extraction. Inclusion criteria were diagnosis of cSDH, one or more long-term AC/AP agent and non-operative management. Data were gathered on a variety of circumstantial and demographic factors including age, comorbidities, blood-thinning agent prescribed, and advise given, whether there were plans to re-scan, whether they were re-referred and if so, when they were re-referred. Re-referrals were determined by whether there were amendments to each patient’s original referral notes that indicated the cSDH had reaccumulated or whether another set of referral notes for the patient were available on the database (indicating re-referral). All re-referred patients at SRFT would have had repeat computed tomography compared to the initial index scans to confirm recurrence.
Data interpretation
The collated data were sorted with various key data points extracted including total number of re-referrals, most frequently advised time interval to withhold medication, most common indication for AC/AP, most routinely prescribed agent, and whether plans were made to re-scan prior to restarting. A Chi-squared test was used to determine whether there was a statistically significant difference in reaccumulation rates in patients asked to stop their agent for 2 weeks versus those asked to stop their agent for longer than 2 weeks.
RESULTS
In total, there were 1220 referrals and 1099 patients referred to SRFT over the 3-year period. This distinction between referrals and patients is outlined as there are a number of patients within the dataset that have been referred more than once over the 3-year period. 501 of these referrals and 479 patients were on one or more anti-thrombotic agent. Crucially, there were 234 referrals and 221 patients that underwent conservative (non-operative) management [
Incidence
According to the Office for National Statistics 2019, the population of Greater Manchester is 2,835,686, where 450,787 over the age of 65.[
Patient characteristics
Participants’ ages ranged from 40 to 100 years (M = 83.3, SD = 8.9) with a statistically significant predominance of male referrals undergoing conservative management compared to females (M: F = 157:64, P =.00001). Of the 221 patients, 100 (45.29%) patients were on AC, 115 (52.04%) on AP (of which 7 were on dual AP), and 6 (2.71%) on both an AC and an AP. The most common indication for AC was AF (n = 75, 33.9%) with Warfarin representing the most frequently prescribed AC (n = 45, 23.08%). A prior cerebrovascular accident most frequently precluded the use of anti-platelets (n = 51, 23.08%), with Aspirin being used most routinely overall (n = 75, 33.94%).
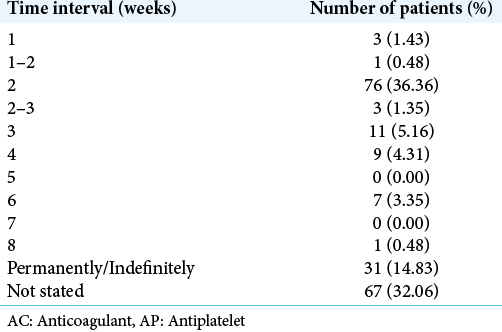
For the remaining analyses, the patient that was re-referred twice will be counted as two separate referrals as the patient had a discrete second cSDH while on an AC. As expected, the most common advice given was to stop the AC (n = 209, 94.14%). The remaining 13 patients were advised to either continue their medication (n = 8, 3.60%), switch to another agent (n = 2, 0.90%), or had no advice documented on their referral notes (n = 3, 1.35%). Of those asked to withhold their AC/AP, a re-scan was planned for 87 of the patients (39.19%). The re-scan was planned prior to re-starting the anti-thrombotic in the majority of cases (n = 68, 78.16%) with the remaining patients either having no mention of when the re-scan was planned (n = 12, 13.79%), or with a scan planned at a point in time separate to planned recommencement (n = 7, 8.05%). The most commonly advised time interval was 2 weeks (n = 76, 36.36%). Unfortunately, a large proportion of patients asked to withhold AC/AP had no specified time interval on the referral notes and were thus classified as “not stated” (n = 67, 32.06%). Of the remaining patients, advise was given to stop for <2 weeks, longer than 2 weeks or permanently/indefinitely [
Reaccumulation rates
Over the 3-year period, there were 13 (5.88%) re-referrals among conservatively managed patients on an anti-thrombotic [
Risk factors for reaccumulation
Information on multiple patient and circumstantial factors available from the referral notes were analyzed to identify any potential risk factors for recurrence. However, no such risk factors were identified.
DISCUSSION
In line with prior literature, this study found a higher incidence of cSDH in general and in patients over the age of 65 compared to a decade ago. It also demonstrated a higher incidence of cSDH among male versus female patients, congruent with prior studies. Crucially, we found that there was no significant difference in reaccumulation rate between patients asked to withhold their anti-thrombotic for 2 weeks versus those asked to stop for longer than 2 weeks.
A 2002 study conducted in North Wales found an incidence of 8.2/100,000 over the age of 65[
The discrepancy in male-female prevalence can be attributed to a multitude of factors. A retrospective study conducted by Jae-Sang et al. (2014) suggests that gender differences in cranial size and asymmetry may contributes to higher incidence of cSDH in male versus female patients. A variety of additional contributing factors have been described in literature including a higher probability of injury in males as well as estrogen and progesterone exerting a neuroprotective function in females.[
Unfortunately, the absence of literature investigating optimal time frames for resumption following conservative management of cSDH makes it difficult to conduct any comparative analysis. However, multiple studies have looked into this following operative management. A similar retrospective study of 596 patients following operative management found a recurrence rate of 22.17%.[
To the best of our knowledge, this is also the first study of this magnitude to focus solely on patients undergoing conservative management. This is of particular importance given the phenomenon of population ageing and the rise in anti-thrombotic prescription in the prophylactic management of a number of cardiovascular disorders. In some of these cases, surgical management will either be not needed, or deemed too risky, resulting in a higher proportion of patients suitable for conservative management. This probability stresses the importance of optimizing how we manage this subset of patients in the coming years and ensure that advice provided is founded on a solid evidence-base.
Retrospective studies have certain intrinsic limitations which were evident in the present study. For instance, omission of key information provided in certain referral notes exemplifies a key limitation of this study. While some specifically mentioned the advice provided to the patient and the agent they had been asked to withhold, a significant proportion of notes had “not stated” this key information and failed to mention when the patient should re-start. This limited the overall data available to be used for statistical analysis. A significant amount of healthcare time is often spent on clarifying this time frame in the form of letters or calls to clinicians. It is also noteworthy to mention that it’s difficult to conclude with absolute certainty that cSDH recurrence in patients on AC/AP was due to the fact that they were on these medication as opposed to other factors such as excessive brain shrinkage or vascular malformations. Furthermore, in the vast majority of cases, information concerning whether coagulation status was checked before restarting anti-thrombotic agents was unavailable. However, the assumption was made that it would have normalized within the chosen time-frame. In addition, this study fails to account for the group of patients that may have experienced a thromboembolic event whilst asked to withhold their AC/ AP which is the other key variable to account for when advising patients. Nevertheless, in our experience, patients who do have a thromboembolic event whilst being off their antithrombotic are generally referred back for further advice. As such, this information would be available on the database and would have been picked up if present.
A prospective study investigating the precise optimal timing for with-holding of AC/AP agents is needed to build on the findings of this study. In particular, a more detailed analysis of reaccumulation rates in patients asked to withhold for <2 weeks (e.g., 10 day or 1 week) is required. Nevertheless, the present findings and the scale of the study serves as an appropriate starting point to build on.
CONCLUSION
A significant proportion of chronic subdural hematomas on antithrombotic agents are managed nonoperatively. Our approach toward advising patients in withholding their agent must be well-defined, evidence-based and mindful of the potential risk of both reaccumulation and thromboembolic events. This study suggests that for the majority of patients, there is no clear benefit in advising patients to cease AC/ AP for longer than 2 weeks. However, further prospective studies are required to consolidate this finding before developing evidence-based guidelines. The rising incidence of this geriatric complication highlights the need for such prospective studies.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adhiyaman V, Chatterjee I. Increasing incidence of chronic subdural haematoma in the elderly. QJM. 2017. 110: 775
2. Asghar M, Adhiyaman V, Greenway MW, Bhowmick BK, Bates A. Chronic subdural haematoma in the elderly-a North Wales experience. J R Soc Med. 2002. 95: 290-2
3. . Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/annualmidyearpopulationestimates/mid2019estimates [Last accessed on 2021 May 10].
4. Balser D, Farooq S, Mehmood T, Reyes M, Samadani U. Actual and projected incidence rates for chronic subdural hematomas in United States veterans administration and civilian populations. J Neurosurg. 2015. 123: 1209-15
5. Chari A, Morgado TC, Rigamonti D. Recommencement of anticoagulation in chronic subdural haematoma: A systematic review and meta-analysis. Br J Neurosurg. 2014. 28: 2-7
6. Ma C, Wu X, Shen X, Yang Y, Chen Z, Sun X. Sex differences in traumatic brain injury: A multi-dimensional exploration in genes, hormones, cells, individuals, and society. Chin Neurosurg J. 2019. 5: 24
7. Markwalder TM. Chronic subdural hematomas: A review. J Neurosurg. 1981. 54: 637-45
8. Oh HJ, Lee KS, Shim JJ, Yoon SM, Yun IG, Bae HG. Postoperative course and recurrence of chronic subdural hematoma. J Korean Neurosurg Soc. 2010. 48: 518-23
9. Oh JS, Shim JJ, Yoon SM, Lee KS. Influence of gender on occurrence of chronic subdural hematoma; is it an effect of cranial asymmetry?. Korean J Neurotrauma. 2014. 10: 82-5
10. Rauhala M, Luoto TM, Huhtala H, Iverson GL, Niskakangas T, Öhman J. The incidence of chronic subdural hematomas from 1990 to 2015 in a defined Finnish population. J Neurosurg. 2019. 132: 1147-57
11. . United Nations Department of Economic and Social Affairs, Population Division. World Population Ageing 2019. 2019. p.
12. Wang Y, Zhou J, Fan C, Wang D, Jiao F, Liu B. Influence of antithrombotic agents on the recurrence of chronic subdural hematomas and the quest about the recommencement of antithrombotic agents: A meta-analysis. J Clin Neurosci. 2017. 38: 79-83
13. Zanaty M, Park BJ, Seaman SC, Cliffton WE, Woodiwiss T, Piscopo A. Predicting chronic subdural hematoma recurrence and stroke outcomes while withholding antiplatelet and anticoagulant agents. Front Neurol. 2020. 10: 1401