- Department of Neurosurgery, Saiseikai Shiga Hospital, Imperial Gift Foundation Inc., Ritto, Shiga, Japan.
- Department of Neurology, Saiseikai Shiga Hospital, Imperial Gift Foundation Inc., Ritto, Shiga, Japan.
Correspondence Address:
Shigeomi Yokoya, Department of Neurosurgery, Saiseikai Shiga Hospital, Imperial Gift Foundation Inc., Ritto, Shiga, Japan.
DOI:10.25259/SNI_536_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shigeomi Yokoya1, Hidesato Takezawa2, Hideki Oka1, Akihiko Hino1. Recurrence of internal carotid artery dissection associated with elongated styloid process: A case report. 20-Sep-2021;12:473
How to cite this URL: Shigeomi Yokoya1, Hidesato Takezawa2, Hideki Oka1, Akihiko Hino1. Recurrence of internal carotid artery dissection associated with elongated styloid process: A case report. 20-Sep-2021;12:473. Available from: https://surgicalneurologyint.com/surgicalint-articles/11119/
Abstract
Background: An elongated styloid process is known to cause ischemic stroke. Previous reports claim that internal carotid artery (ICA) dissection due to the elongated styloid process has good outcomes when treated conservatively; however, long-term follow-up has not been attempted and recurrence in the later period has not been reported so far. We report a case of recurrence of symptoms over a decade after the initial onset.
Case Description: A 59-year-old man experienced a transient ischemic attack (TIA) 10 years ago. Six years ago, he experienced hemispheric TIA, and magnetic resonance angiography revealed a diminished signal of the left ICA; however, no further examination was performed. Four years ago, he experienced another transient amaurosis attack and was treated with antiplatelet therapy because no embolic source was detected using ultrasonography examination, and he was diagnosed with idiopathic ICA dissection. Recently, he experienced a third amaurosis fugax attack. Digital subtraction angiography and cone-beam computed tomography demonstrated left cervical ICA dissection due to elongated styloid process. He underwent surgical resection of the left styloid process and cervical stent placement. He had no ischemic attacks postoperatively.
Conclusion: The elongated styloid process may cause recurrent ischemic attacks over a decade due to ICA dissection.
Keywords: Elongated styloid process, Internal carotid artery dissection, Recurrence
INTRODUCTION
The elongated styloid process is one of the causative diseases of stroke, where ischemic neurologic symptoms are caused by the compression of the cervical internal carotid artery (ICA) because of the elongated styloid process or calcification of the stylohyoid ligament. ICA dissection or compression due to elongated styloid process is a rare condition; therefore, it is often misdiagnosed as idiopathic ICA dissection.
Most with ICA dissection due to elongated styloid process have been treated conservatively and have been reported to have a good course;[
We present a case of cervical ICA dissection due to elongated styloid process which recurred over a long period and repeatedly showed symptoms. We also review articles on the management of these uncommon lesions, particularly to the recurrence or deterioration of the lesions after conservative or endovascular treatment.
CASE DESCRIPTION
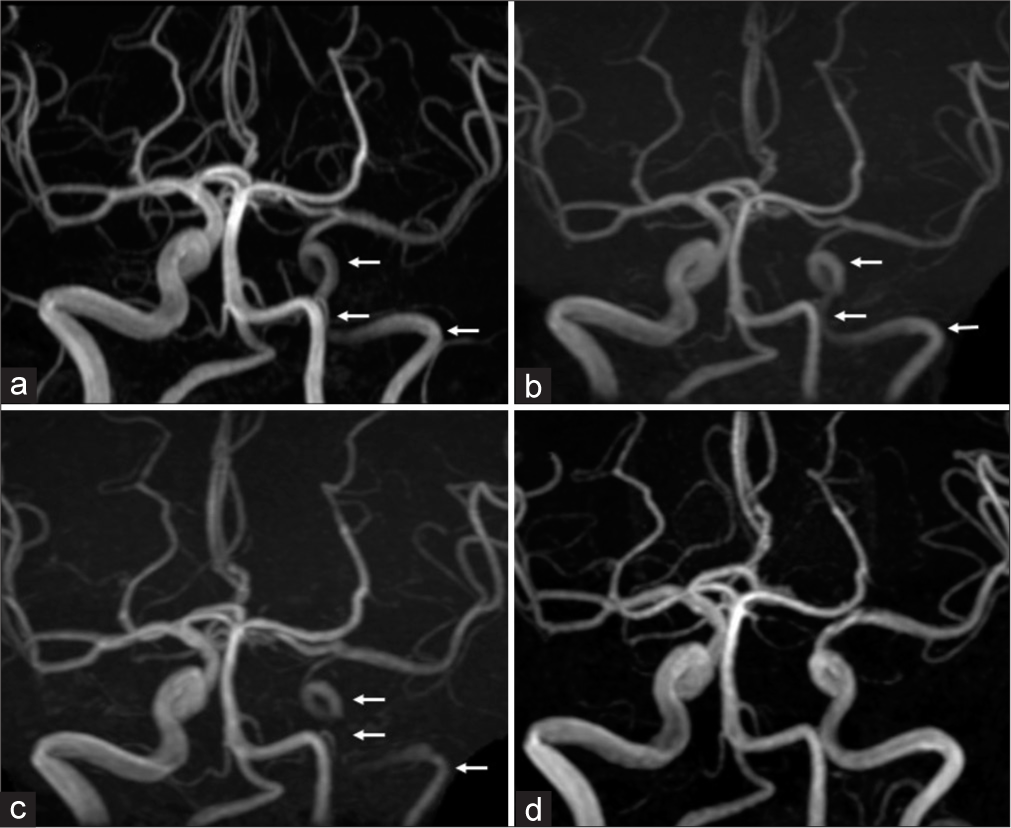
A 59-year-old man with a history of medically treated hypertension and hyperlipidemia had a transient ischemic attack (TIA) and was transferred to another hospital 10 years ago; however, the details about the case were unknown. Six years ago, he had a left transient amaurosis attack and magnetic resonance angiography (MRA) revealed a decreased signal of the left ICA [
Figure 1:
Magnetic resonance angiography (MRA) images of the patient. MRA obtained 6 years ago (a), 4 years ago (b), and preoperatively (c) demonstrating that the signal of the intracranial left internal carotid artery (ICA) is gradually reduced (white arrow). MRA obtained after the resection of styloid process and carotid artery stenting (CAS), demonstrated the improvement of the ICA signal (d).
Recently, the left amaurosis fugax reappeared, and the patient was referred to our hospital. Oral administration of clopidogrel (75 mg/day) and cilostazol tablets (100 mg/day) managed the amaurosis fugax. Due to repeated amaurosis attacks, with the ophthalmic assessments to exclude other ocular or retinal pathology, and gradually decreasing left ICA on MRA [
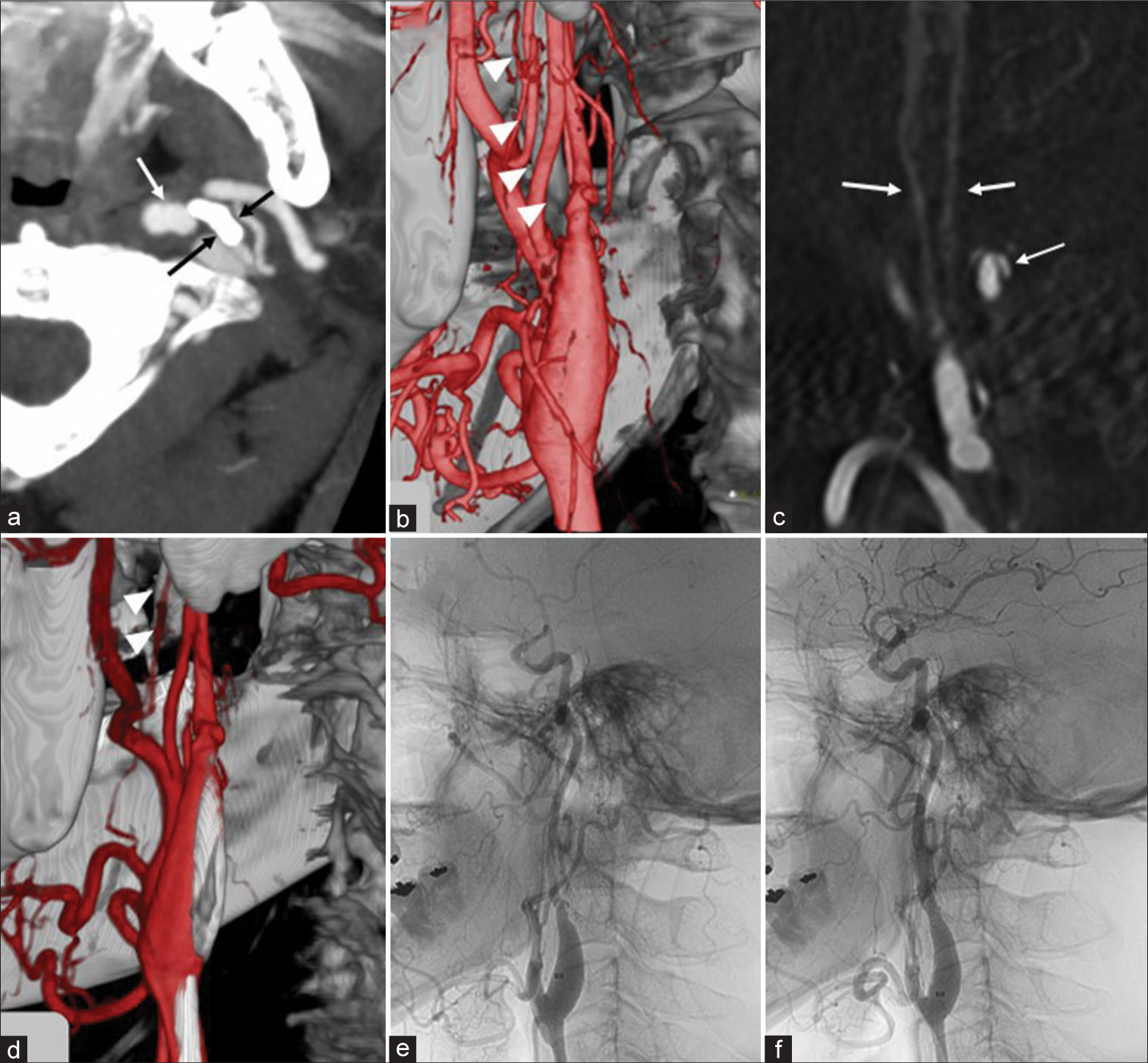
Figure 2:
CT angiography, cone-beam computed tomography (CT), and digital subtraction angiography (DSA) of the patient. Preoperative CT angiography, axial image, demonstrating that left elongated styloid process (black paired arrows) is directly impinging on the ICA (white arrow) (a). Preoperative fusion image (cone-beam CT and 3D-DSA) demonstrating the tapered and irregular stenosis of the left internal carotid artery (ICA). The tip of elongated styloid process was very close to the ICA (arrowheads), and the ICA showed severe luminal stenosis (b). Preoperative 3D-DSA (CT-like images), sagittal view, demonstrating the false lumen (white arrow) associated with the elongated styloid process (white paired arrows) (c). Fusion image (cone-beam CT and 3D-DSA) obtained after the resection of elongated styloid process demonstrated the shortening of the styloid process (arrowhead), and the tip was no longer close to the ICA (d). The ICA angiogram (lateral view) before (e) and after (f) the procedure of carotid artery stenting (CAS) demonstrated the resolution of the left ICA stenosis.
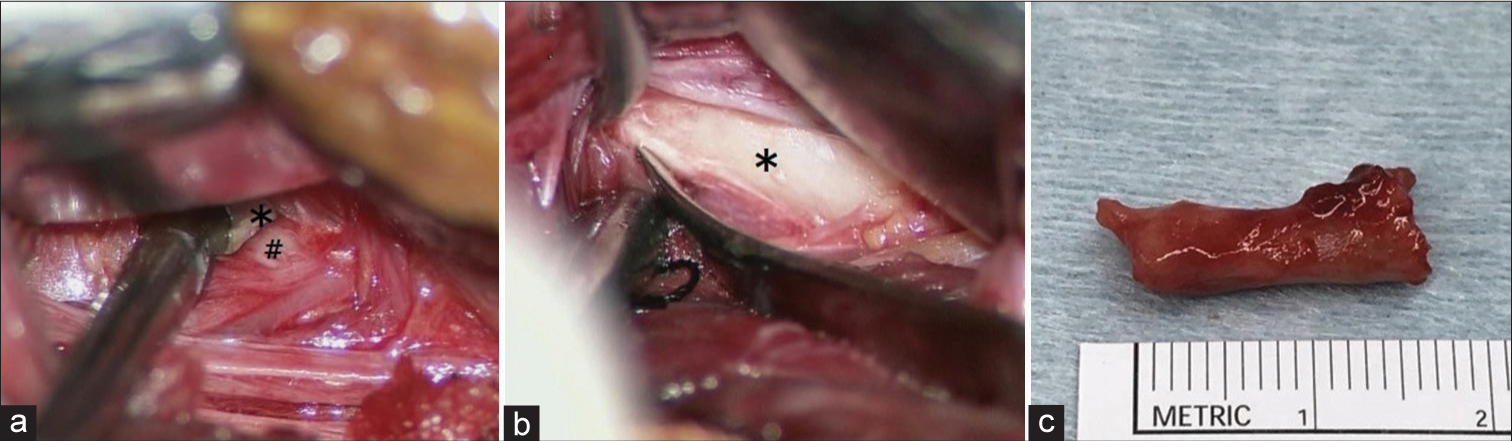
The patient underwent left styloid resection through transcervical approach. In the surgery, we confirmed that the tip of the styloid process was very close to the ICA [
Figure 3:
Intraoperative photographs during resection of the elongated styloid process. Using the infradigastric muscle approach, the tip of the styloid process (*) and cervical ICA (#) is in contact with each other (a). Using the supradigastric approach, the bony structure was stripped of from its periosteum and muscle (b), and the tip that is approximately 2 cm of the process was amputated and removed (c).
In addition, the patient underwent stent placement (Stent: Precise 6 × 20) since we considered that the residual severe stenosis caused by the left cervical ICA dissection could lead to further ischemic events [
DISCUSSION
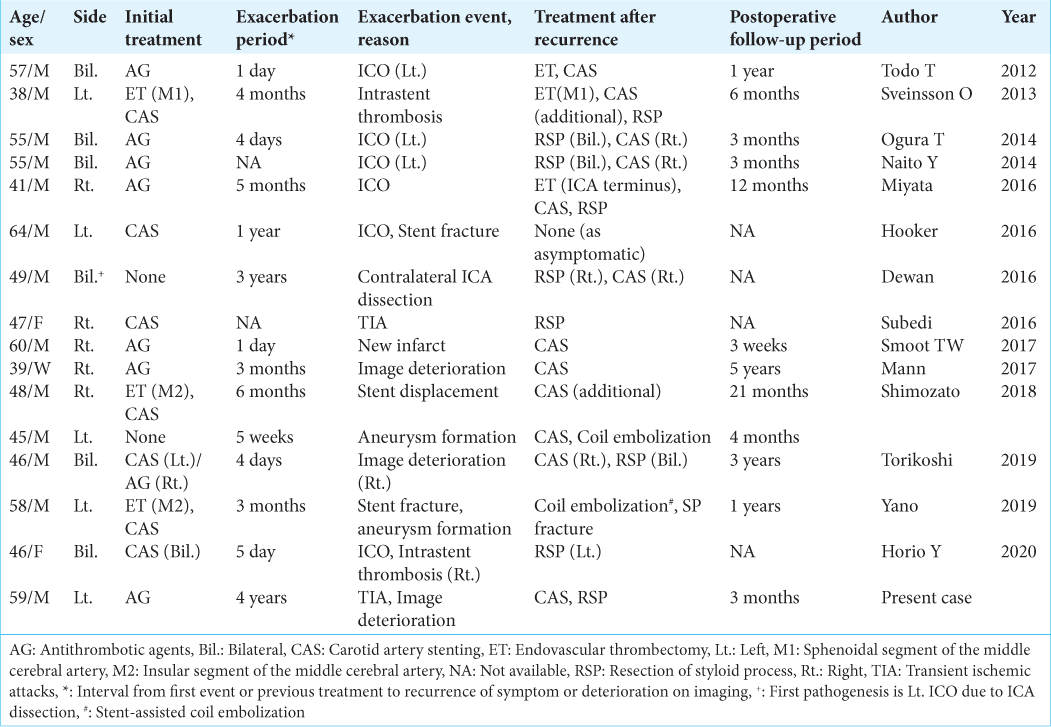
We present a case of recurrent ischemic symptoms after 10 years caused by cervical ICA dissection due to elongated styloid process, although without an accurate diagnosis. To the best of our knowledge, 15 cases of progression or recurrence after initial therapy due to elongated styloid process have been described so far [
First, clinicians must distinguish between “idiopathic” ICA dissection and “traumatic” ICA dissection caused by the elongated styloid process. Otherwise, preventable embolic stroke may reoccur. Several reported cases of ICA dissection with elongated styloid process have recurred or worsened even after diagnosis and administration of oral antithrombotic agents [
Cervical ICA dissection due to the elongated styloid process can cause recurrent ischemic events in the long term, and long-term follow-up may be necessary, even if conservative treatment does not cause a short-term recurrence. Although most cases of ICA dissection recurrence due to elongated styloid process occur in the acute phase [
Many reports have indicated that conservative treatments such as antithrombotic therapy, with or without cervical rest, are effective.[
Second, considering the risk of recurrence, it may be justified to consider surgical treatment aggressively – especially for elongated styloid process resection – when diagnosing a patient with ICA dissection associated with the elongated styloid process. Most acute treatments for the progression have been performed by carotid artery stenting (CAS); however, the few complications followed by CAS may be due to the stent being affected by elongated styloid process such as stent fracture, intrastent thrombosis, and stent displacement [
CONCLUSION
Clinicians should take into consideration the possibility of elongated styloid process when diagnosing spontaneous cervical ICA dissection to prevent the occurrence of future ischemic events.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aldakkan A, Dunn M, Warsi NM, Mansouri A, Marotta TR. Vascular eagle’s syndrome: Two cases illustrating distinct mechanisms of cerebral ischemia. J Radiol Case Rep. 2017. 11: 1-7
2. Atkinson JL, Piepgras DG, Huston J, Mokri B. Cervical artery dissections: Evidence for redissection in previously dissected arteries: Report of three cases. Neurosurgery. 2002. 51: 797-801
3. Bassetti C, Carruzzo A, Sturzenegger M, Tuncdogan E. Recurrence of cervical artery dissection. A prospective study of 81 patients. Stroke. 1996. 27: 1804-7
4. Dewan MC, Morone PJ, Zuckerman SL, Mummareddy N, Ghiassi M, Ghiassi M. Paradoxical ischemia in bilateral Eagle syndrome: A case of false-localization from carotid compression. Clin Neurol Neurosurg. 2016. 141: 30-2
5. Hooker JD, Joyner DA, Farley EP, Khan M. Carotid stent fracture from stylocarotid syndrome. J Radiol Case Rep. 2016. 10: 1-8
6. Horio Y, Fukuda K, Miki K, Hirao N, Iwaasa M, Abe H. Dynamic assessment of internal carotid artery and elongated styloid process in a case of bilateral carotid artery dissection. Surg Neurol Int. 2020. 11: 163
7. Ikenouchi H, Takagi M, Nishimura A, Yamaguchi E, Koge J, Saito K. Bilateral carotid artery dissection due to eagle syndrome in a patient with vascular ehlers-danlos syndrome: A case report. BMC Neurol. 2020. 20: 285
8. Miyata H, Nakahara I, Ohta T, Matsumoto S, Sadamasa N, Ishibashi R. A case of internal carotid artery dissection caused by an elongatedstyloid process: Successful treatment with carotid artery stenting and partial resection of the styloid process. Surg Cereb Stroke. 2016. 44: 145-50
9. Muthusami P, Kesavadas C, Sylaja PN, Thomas B, Harsha KJ, Kapilamoorthy TR. Implicating the long styloid process in cervical carotid artery dissection. Neuroradiology. 2013. 55: 861-7
10. Ohara N, Sakaguchi M, Okazaki S, Nagano K, Kitagawa K. Internal carotid artery dissection caused by an elongated styloid process: Usefulness of transoral ultrasonography. J Stroke Cerebrovasc Dis. 2012. 21: 918.e7-8
11. Ohta T, Hotta J, Yamauchi T, Ozawa H, Kubokura T. Recurrence of bilateral spontaneous cervical internal carotid artery dissection after a 12-year-interval: A case report. No To Shinkei. 2004. 56: 705-9
12. Raser JM, Mullen MT, Kasner SE, Cucchiara BL, Messé SR. Cervical carotid artery dissection is associated with styloid process length. Neurology. 2011. 77: 2061-6
13. Renard D, Azakri S, Arquizan C, Swinnen B, Labauge P, Thijs V. Styloid and hyoid bone proximity is a risk factor for cervical carotid artery dissection. Stroke. 2013. 44: 2475-9
14. Schievink WI, Mokri B, O’Fallon WM. Recurrent spontaneous cervical-artery dissection. N Engl J Med. 1994. 330: 393-7
15. Shindo T, Ito M, Matsumoto J, Miki K, Fujihara F, Terasaka S. A case of juvenile stroke due to carotid artery dissection from an elongated styloid process-revisiting conservative management. J Stroke Cerebrovasc Dis. 2019. 28: 104307
16. Soo OY, Chan YL, Wong KS. Carotid artery dissection after prolonged head tilting while holding a newborn baby to sleep. Neurology. 2004. 62: 1647-8
17. Sveinsson O, Kostulas N, Herrman L. Internal carotid dissection caused by an elongated styloid process (eagle syndrome). BMJ Case Rep. 2013. 2013: bcr2013009878
18. Torikoshi S, Yamao Y, Ogino E, Taki W, Sunohara T, Nishimura M. A staged therapy for internal carotid artery dissection caused by vascular eagle syndrome. World Neurosurg. 2019. 129: 133-9
19. Yamamoto S, Todo K, Kawamoto M, Kohara N. Carotid artery dissection associated with an elongated styloid process. Intern Med. 2013. 52: 1005-6
20. Yano T, Sasaki I, Kiyohara K, Kawanishi M. Carotid stent fracture due to eagle syndrome after endovascular stenting for the treatment of acute ischemic stroke caused by internal carotid artery dissection: Case report. J Neuroendovasc Ther. 2019. 13: 454-61
21. Zuber M, Meder JF, Mas JL. Carotid artery dissection due to elongated styloid process. Neurology. 1999. 53: 1886-7