- Department of Spine Surgery, Sancheti Institute of Orthopedics and Rehabilitation, Pune, Maharashtra, India.
Correspondence Address:
Rajendra Sakhrekar, Department of Spine Surgery, Sancheti Institute of Orthopedics and Rehabilitation, Pune, Maharashtra, India.
DOI:10.25259/SNI_442_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Rajendra Sakhrekar1, Ketan Khurjekar1, Shailesh Hadgaonkar1, Pramod Bhilare1, Parag Sancheti1, Ashok Shyam1. Recurrent solitary bone plasmacytoma: A case report. 19-Jul-2021;12:356
How to cite this URL: Rajendra Sakhrekar1, Ketan Khurjekar1, Shailesh Hadgaonkar1, Pramod Bhilare1, Parag Sancheti1, Ashok Shyam1. Recurrent solitary bone plasmacytoma: A case report. 19-Jul-2021;12:356. Available from: https://surgicalneurologyint.com/surgicalint-articles/10982/
Abstract
Background: Plasmacytoma is an hematological malignancy that originates in bone. It may involve a single skeletal location. Notably, these lesions can progress to involve multiple segments in 50% of cases, at which point they are classified as having multiple myeloma (MM).
Case Description: One year ago, this patient had undergone a D6 laminectomy and biopsy for plasmacytoma. Now at age 73, she newly presented with the onset of a progressive paraparesis of 4 weeks’ duration. On examination, she had 3/5 strength in both lower extremities accompanied by diffuse hyperreflexia, and bilateral Babinski signs. She underwent a D5-D7 decompression, D6 corpectomy with anterior mesh cage reconstruction, and a D3-D9 posterior fusion.
Conclusion: Patients originally treated for plasmacytoma present 50% of the time with the new onset of neurological symptoms and signs due to the subsequent evolution of MM. As these lesions may be refractory to radiation and/or chemotherapy, surgery is often warranted.
Keywords: Instability, Neurodeficit, Recurrence, Solitary bone plasmacytoma, Surgical management
INTRODUCTION
Plasmacytoma is an hematological malignancy that primarily originates in bone. It can occur as a single skeletal location, a factor which differentiates it from multiple myeloma (MM) (i.e., plasmacytoma progresses to involve multiple spinal segments in 50% of cases at which point it is relabeled resulting MM).[
CASE REPORT
A 73-year-old female had been treated for a D6 spinal plasmacytoma 1 year previously (i.e., utilizing a D6 laminectomy and biopsy). She now newly presented with the acute onset of a paraparesis (3/5 motor deficit in the lower extremities) of 4 weeks’ duration.
Diagnostic studies
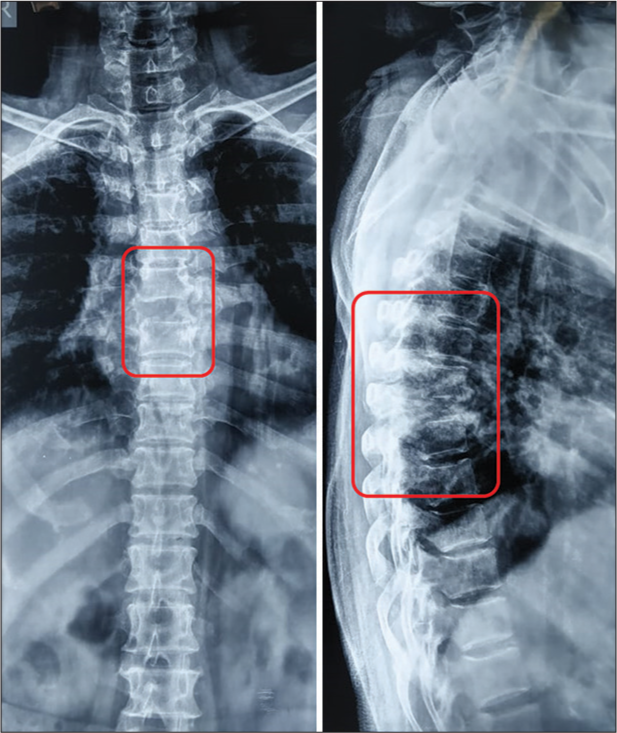
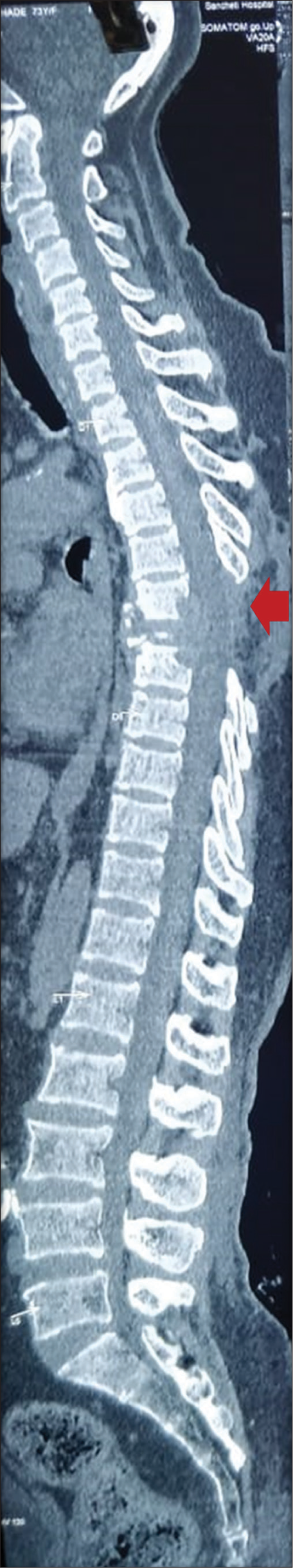
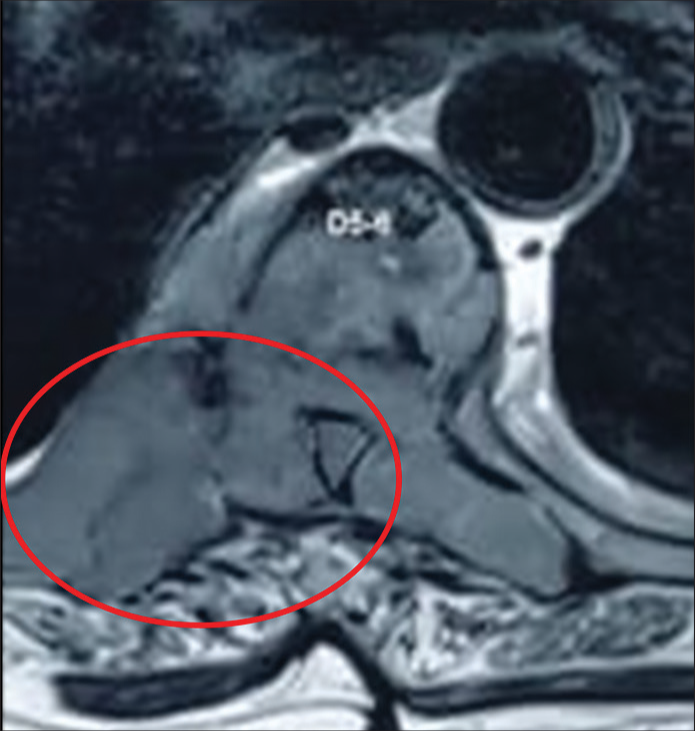
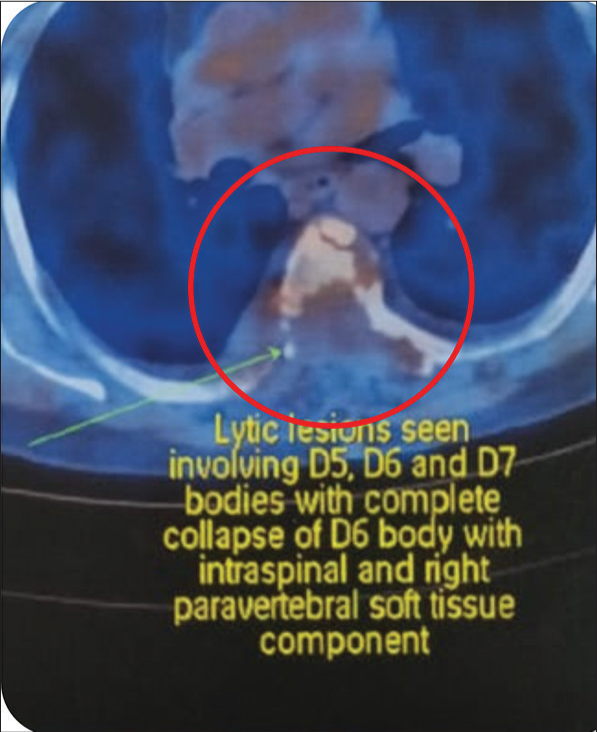
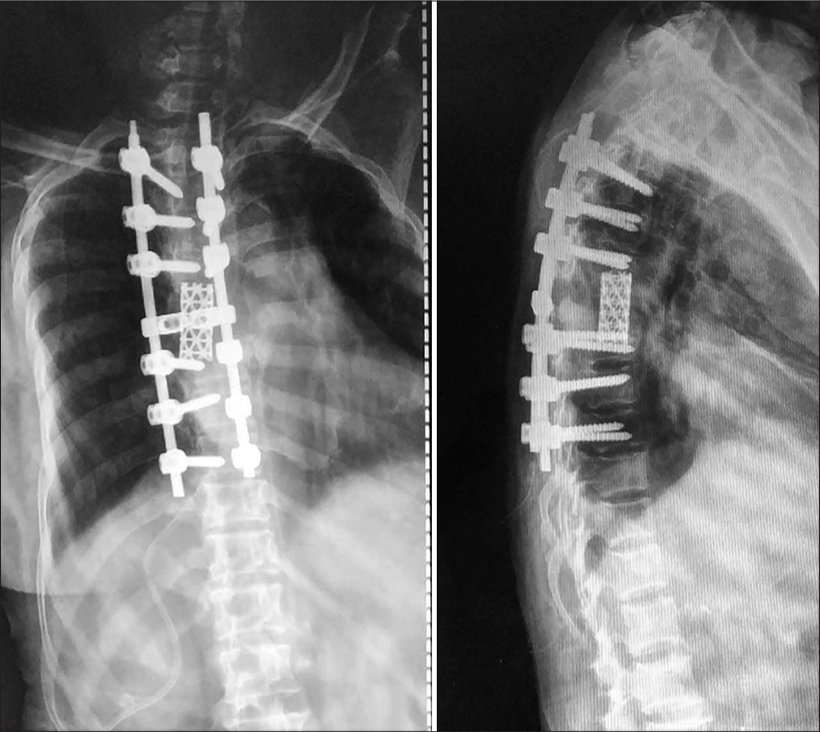
X-ray and MRI studies both showed a new, pathologic, unstable fracture of D6 involving all three columns; this resulted in significant collapse of the D6 vertebral body with focal kyphosis [
Surgery
Indications for urgent surgery included intractable pain and a progressive paraparesis of 4 weeks duration. It included a single-stage procedure; a D5-D7 decompression, D6 corpectomy with anterior mesh cage reconstruction, and a D3-D9 posterior fusion [
This stabilized the spinal column, while providing for sufficient resection and decompression of tumor. It was followed by adjuvant radiation therapy.
Pathology
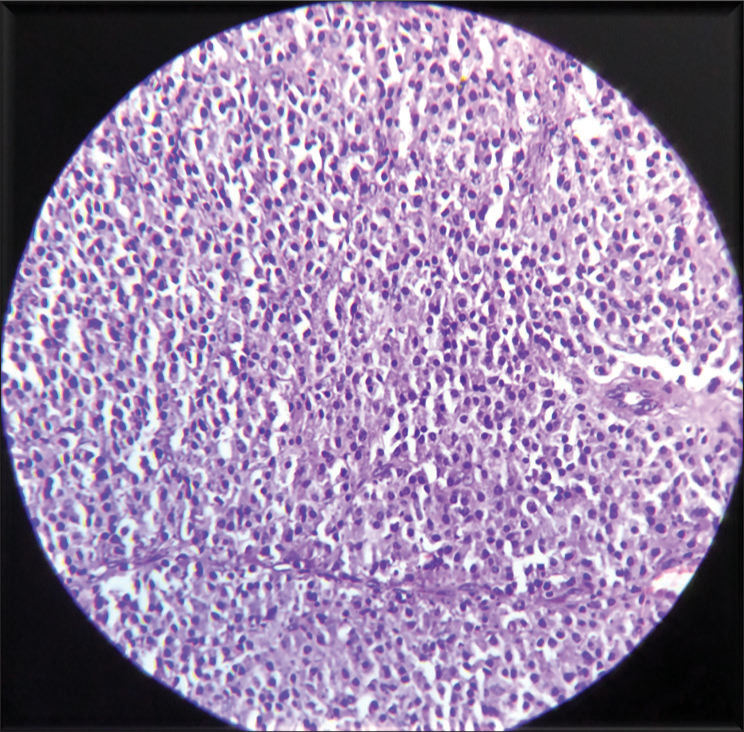
The biopsy confirmed the diagnosis of plasmacytoma, showing sheets and clusters of plasma cells including immature forms with focal nuclear pleomorphism [
Postoperative course
Postoperatively, her pain dramatically decreased; she was mobilized the day after surgery. She continued to improve up to 2 years following the surgery (i.e., VAS improved to 1/10 and ODI score to 4).
DISCUSSION
Incidence and location of SBP
SBP most commonly affects the axial skeleton (25–60%) and has a predilection for the thoracic spine. Further, SPB has a high risk of progression to MM.[
CT and MR studies of SBP
CT or MRI can detect the lesions and describe the tumor extent at its earlier stage. MRI has an important role in the description of the residual tumor, local relapse and tumor progression to MM after treatment.
Biopsy and treatment modalities
Biopsy and histopathology play an important role in the diagnosis and management of this disease. Notably, radiotherapy is considered the treatment of choice for SPB.[
CONCLUSION
Surgical management of plasmacytomas is advised in cases involving significant pathological fractures, cord compression, and/or instability contributing to severe neurological deficits.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Baba H, Maezawa Y, Furusawa N, Wada M, Kokubo Y, Imura S. Solitary plasmacytomas of the spine associated with neurological complications. Spinal Cord. 1998. 36: 4170-5
2. Dimopoulos M, Kiamouris C, Moulopoulos LA. Solitary bone plasmacytoma and extramedullary plasmacytoma. Curr Treatment Options Oncol. 2002. 3: 255-9
3. Dimopoulos M, Terpos E, Comenzo RL, Tosi P, Beksac M, Sezer O. International myeloma working group consensus statement and guidelines regarding the current role of imaging techniques in the diagnosis and monitoring of multiple Myeloma. Leukemia. 2009. 23: 1545-56
4. Dores GM, Landgren O, McGlynn KA, Curtis RE, Linet MS, Devesa SS. Plasmacytoma of bone, extramedullary plasmacytoma, and multiple myeloma: Incidence and survival in the United States, 1992-2004. Br J Haematol. 2009. 144: 86-94
5. He MX, Zhu MH, Zhang YM, Fu QG, Wu LL.editors. Solitary plasmacytoma of spine: A clinical, radiologic and pathologic study of 13 cases. 2009. 38: 307-11
6. Holland J, Trenkner DA, Wasserman TH, Fineberg B. Plasmacytoma: Treatment results and conversion to myeloma. Cancer. 1992. 69: 1513-7
7. Jyothirmayi R, Gangadharan VP, Nair MK. Radiotherapy in the treatment of solitary plasmocytoma. Br J Radiol. 1997. 70: 511-6
8. Ozsahin M, Tsang RW, Poortmans P, Belkacémi Y, Bolla M, Dinçbas FO. Outcomes and patterns of failure in solitary plasmacytoma: A multicentre rare cancer network study of 258 patients. Int J Radiat Oncol Biol Phys. 2006. 64: 210-7
9. Takahashi T, Koshu K, Tominaga T, Takahashi A, Yoshimoto T. Solitary plasmacytoma in the thoracic spine. Two case reports. Neurosurg Rev. 1998. 21: 121-5
10. Tsutsumi S, Yasumoto Y, Ito M. Solitary spinal extradural plasmacytoma: A case report and literature review. Clin Neuroradiol. 2013. 23: 5-9
11. Wiltshaw E. The natural history of extramedullary plasmacytoma and its relation to solitary myeloma of bone and myelomatosis. Medicine. 1976. 55: 217-38