- Department of Neurosurgery, All India Institute of Medical Sciences, Raipur, Chhattisgarh, India.
- Department of Pediatrics, All India Institute of Medical Sciences, Raipur, Chhattisgarh, India.
Correspondence Address:
Charandeep Singh Gandhoke, Department of Neurosurgery, All India Institute of Medical Sciences, Raipur, Chhattisgarh, India.
DOI:10.25259/SNI_748_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Abbas Hibtullah Moaiyadi1, Mayank Tripathi1, Pavan Tulshiram Lanjewar1, Simran Kaur Syal2, Binoy Kumar Singh1, Shailendra Anjankar1, Charandeep Singh Gandhoke1. Remote supratentorial intraparenchymal bleed after posterior fossa surgery: A rare occurrence. 15-Mar-2024;15:83
How to cite this URL: Abbas Hibtullah Moaiyadi1, Mayank Tripathi1, Pavan Tulshiram Lanjewar1, Simran Kaur Syal2, Binoy Kumar Singh1, Shailendra Anjankar1, Charandeep Singh Gandhoke1. Remote supratentorial intraparenchymal bleed after posterior fossa surgery: A rare occurrence. 15-Mar-2024;15:83. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12805
Abstract
Background: Intraparenchymal hemorrhage at the operative site is one of the major complications of brain surgery. It is unusual to occur at a site remote from the operative site, but when it happens, it may cause significant morbidity and mortality.
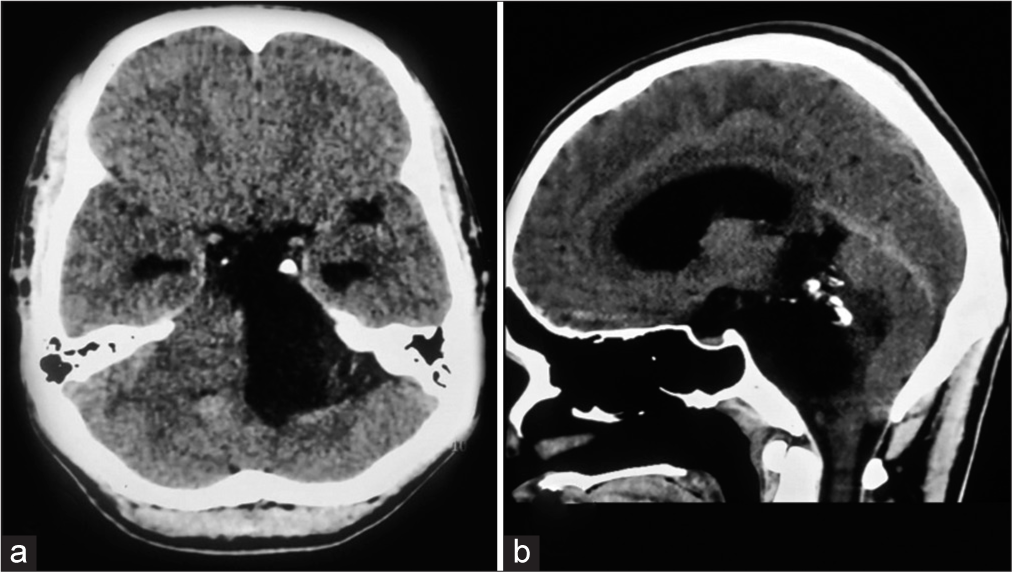
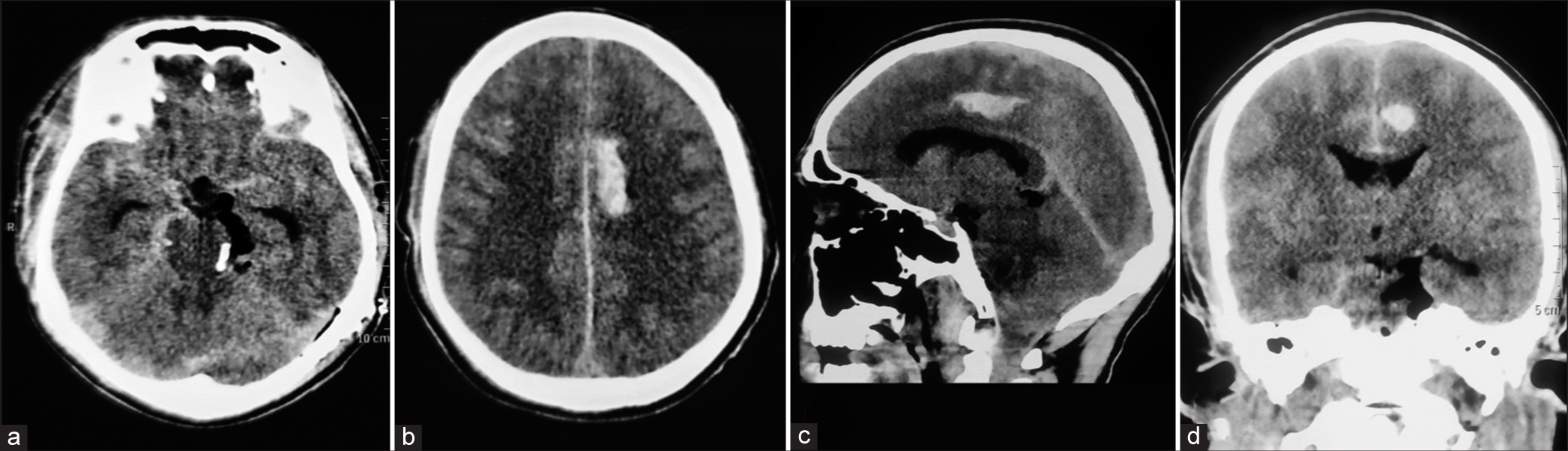
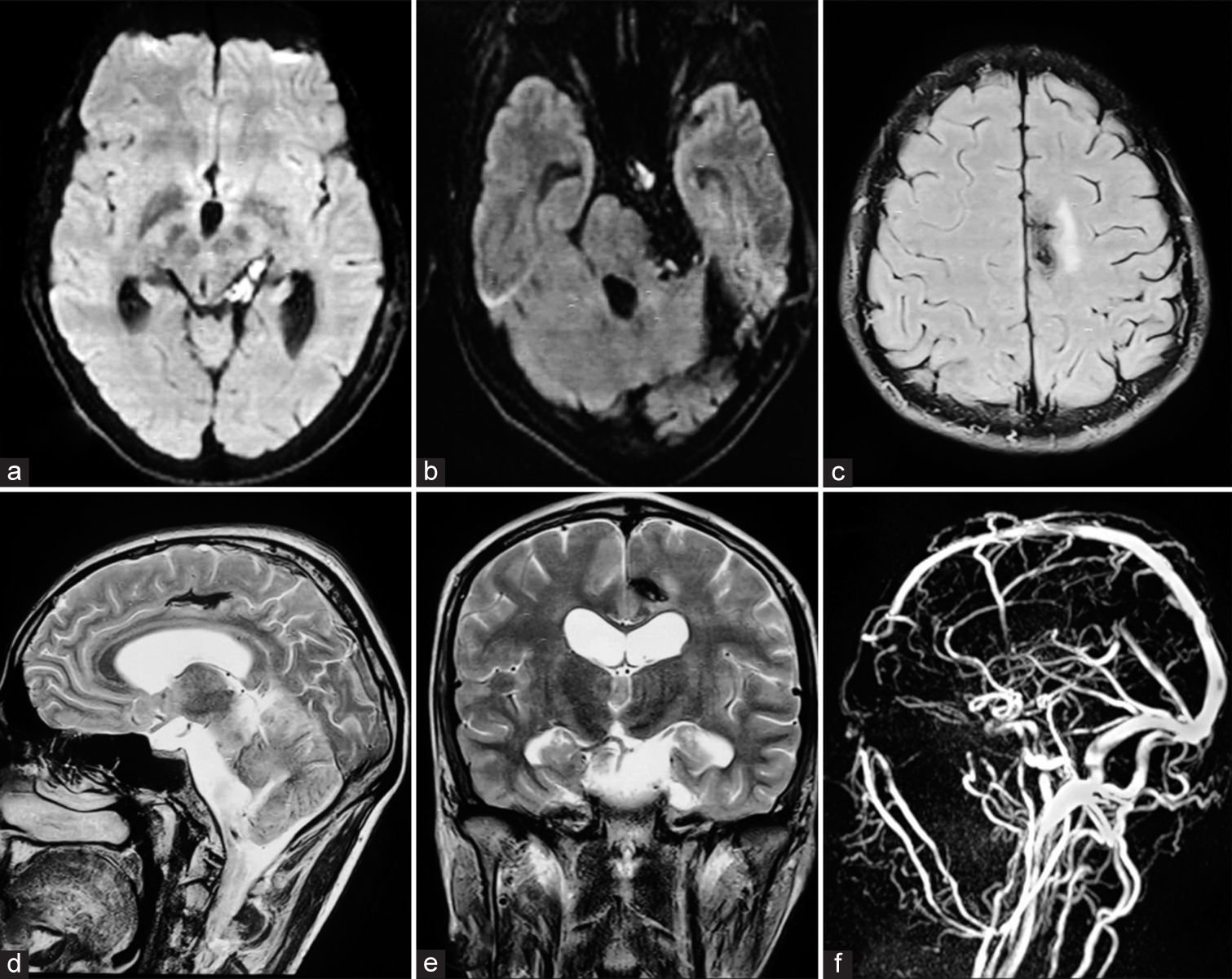
Case Description: We report the case of a 27-year-old male who presented with complaints of paresthesias over the left side of his face and decreased hearing from the left ear for two years. His radiology was suggestive of a large left cerebellopontine angle epidermoid cyst. The patient underwent left retro mastoid suboccipital craniotomy and near-total excision of the epidermoid cyst. The immediate postoperative non-contrast computed tomography scan of the brain was suggestive of no hematoma at the operated site but a remote left parafalcine frontoparietal intraparenchymal bleed, which was managed conservatively. At two months follow-up, he had no neuro deficits, and magnetic resonance imaging of the brain was suggestive of near-total excision of the epidermoid cyst with resolving left parafalcine frontoparietal bleed.
Conclusion: We report this case due to the unique case observation of an intracranial bleed at a remote site rather than at the operated site.
Keywords: Cerebellopontine (CP) angle epidermoid, Intraparenchymal bleed, Posterior fossa surgery, Remote, Supratentorial
INTRODUCTION
Intraparenchymal hemorrhage at the operative site is one of the major complications of brain surgery. It is unusual to occur at a site remote from the operative site, but when it happens, it may cause significant morbidity and mortality.
CASE DESCRIPTION
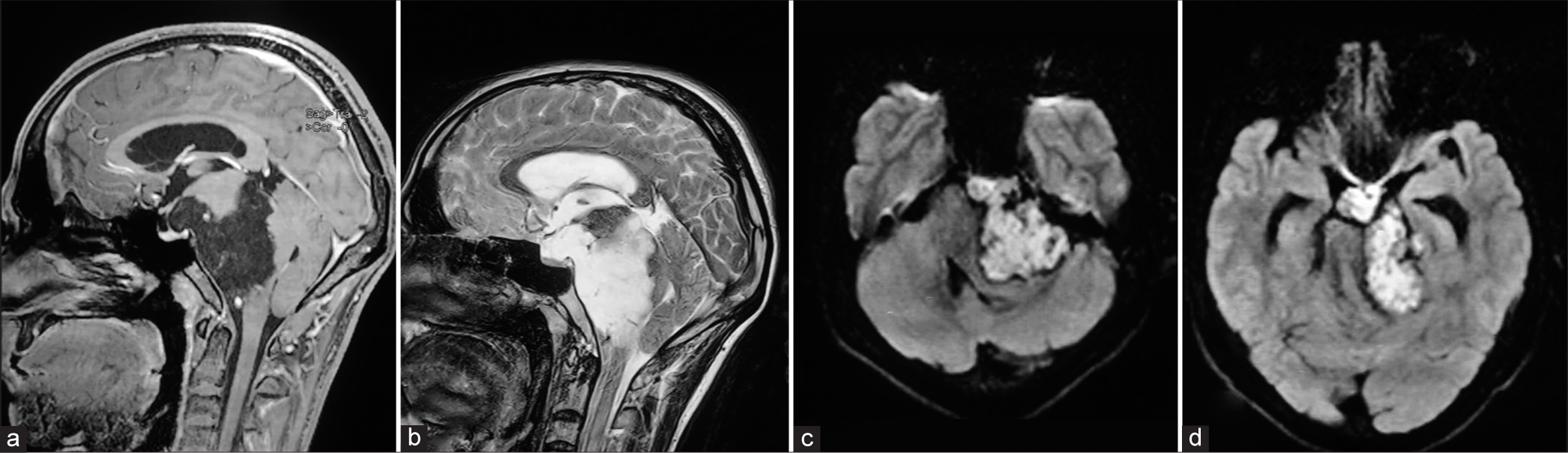
We report the case of a 27-year-old male who presented with complaints of paresthesias over the left side of his face and decreased hearing from the left ear for two years. Neurological examination revealed horizontal nystagmus, gait ataxia, and mild left sensorineural hearing loss. His radiology was suggestive of a large extra-axial lesion in the left cerebellopontine (CP) angle with diffusion restriction. The lesion was encasing the cisternal segment of the left 7th–8th cranial nerves and was indenting the left middle cerebellar peduncle. Superiorly, the lesion was extending into the left half of the ambient and quadrigeminal cisterns and anteriorly, the lesion was bulging into the suprasellar cistern. His imaging was suggestive of a left CP angle epidermoid cyst [
Figure 1:
Preoperative magnetic resonance imaging of the brain revealed (a) T1 hypointense, (b) T2 hyperintense lesion in the left cerebellopontine angle cistern with (c and d) diffusion restriction and extensions into the ambient, quadrigeminal, and suprasellar cisterns with no postcontrast enhancement suggestive of epidermoid cyst.
DISCUSSION
Haines et al., in their paper, reported the incidence of supratentorial hemorrhage after posterior fossa surgeries was 0.6%.[
The sitting position during surgery can reduce arterial blood flow, resulting in ischemia.[ Excessive drainage of cerebrospinal fluid during surgery (probable pathophysiology in our case) and also through the Romo Vac drain from a small dural leak after surgery can lead to intracranial hypotension and remote site bleed.[ Supratentorial bleeds after posterior fossa surgery can occur secondary to a rapid elevation of the arterial pressure.[ There is the possibility of dural venous sinus thrombosis due to sinus injury leading to venous hypertension and parenchymal bleed.[ There can be occlusion of the internal carotid or vertebral arteries in the neck by improper positioning of the head, leading to intraoperative ischemia and hemorrhage within the infarcted brain after repositioning of the patient.[ Coagulation disorders can be the cause of remote intraparenchymal bleed and need to be ruled out.[
CONCLUSION
We reported this case due to the unique case observation of an intracranial bleed at a remote site rather than at the operated site which in our case, was probably due to excessive drainage of cerebrospinal fluid during surgery.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Agrawal A, Kakani A, Ray K. Extensive supratentorial hemorrhages following posterior fossa meningioma surgery. J Surg Tech Case Rep. 2010. 2: 87-9
2. Cartier-Giroux J, Mohr G, Sautreaux JL. Supratentorial hemorrhage of hypertensive origin during operation: An unusual complication of surgery on the posterior fossa in the sitting position. Neurochirurgie. 1980. 26: 291-4
3. Cloft HJ, Matsumoto JA, Lanzino G, Cail WS. Posterior fossa hemorrhage after supratentorial surgery. AJNR Am J Neuroradiol. 1997. 18: 1573-80
4. De Albuquerque LA, Dourado JC, Almeida JP, Costa BS. Multiple supratentorial intraparenchymal hemorrhage after posterior fossa surgery. Surg Neurol Int. 2015. 6: S104-9
5. Haines SJ, Maroon JC, Jannetta PJ. Supratentorial intracerebral hemorrhage following posterior fossa surgery. J Neurosurg. 1978. 49: 881-6
6. Salunke P, Malik V, Kovai P, Aggarwal A, Khandelwal NK. Delayed supratentorial intracerebral hemorrhage following posterior fossa surgery. Asian J Neurosurg. 2016. 11: 315