- Department of Neurosurgery, Fukuoka University, Fukuoka, Japan.
Correspondence Address:
Kazunori Oda, Department of Neurosurgery, Fukuoka University, Fukuoka, Japan.
DOI:10.25259/SNI_267_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kana Takeda, Kazunori Oda, Hironori Fukumoto, Hiromasa Kobayashi, Takashi Morishita, Koichiro Takemoto, Mitsutoshi Iwaasa, Hiroshi Abe. Repeated coil embolization of traumatic basilar artery pseudoaneurysm accompanied by bilateral traumatic internal carotid artery stenosis following severe head injury in a pediatric patient: A case report and literature review. 08-Jun-2023;14:199
How to cite this URL: Kana Takeda, Kazunori Oda, Hironori Fukumoto, Hiromasa Kobayashi, Takashi Morishita, Koichiro Takemoto, Mitsutoshi Iwaasa, Hiroshi Abe. Repeated coil embolization of traumatic basilar artery pseudoaneurysm accompanied by bilateral traumatic internal carotid artery stenosis following severe head injury in a pediatric patient: A case report and literature review. 08-Jun-2023;14:199. Available from: https://surgicalneurologyint.com/surgicalint-articles/12356/
Abstract
Background: Few cases of pediatric traumatic intracranial aneurysms (pTICAs) in the posterior circulation involving the basilar artery (BA) following severe head trauma have been reported. Here, we describe a pediatric case of traumatic BA pseudoaneurysm accompanied by bilateral traumatic internal carotid artery (ICA) stenosis following blunt head trauma.
Case Description: A 16-year-old boy presented to our emergency department after being hit by a car. The patient was initially diagnosed with multiple skull base fractures underlying traumatic subarachnoid hemorrhage and left acute epidural hematoma. Seven days following emergency craniectomy, magnetic resonance imaging revealed bilateral ICA stenosis, BA stenosis, and BA pseudoaneurysm. We decided to perform coil embolization, resulting in body filling and a volume embolization ratio of 15.7%. Twenty-eight days after coil embolization, digital subtraction angiography revealed aneurysmal rupture. We performed repeated coil embolization, resulting in body filling and a volume embolization ratio of 20.9%.
Conclusion: We reported a pediatric case of traumatic BA pseudoaneurysm accompanied by bilateral traumatic ICA stenosis following a severe head injury treated with repeated coil embolization. Considering the risk of further brain injury due to high incidence of rupture, early vascular survey and appropriate treatment may be the most important prognostic factors in pTICAs.
Keywords: Basilar artery, Coil enbolization, Head injury, Neurosurgery, Pediatric, Pseudoaneurysm, Trauma, Traumatic intracranial aneurysm, Traumatic pseudoaneurysm
INTRODUCTION
Pediatric intracranial aneurysms are caused by infection, trauma, or congenital factors. Pediatric traumatic intracranial aneurysms (pTICAs) account for less than 5% of all intracranial aneurysms and can result from penetrating or severe head trauma.[
CASE PRESENTATION
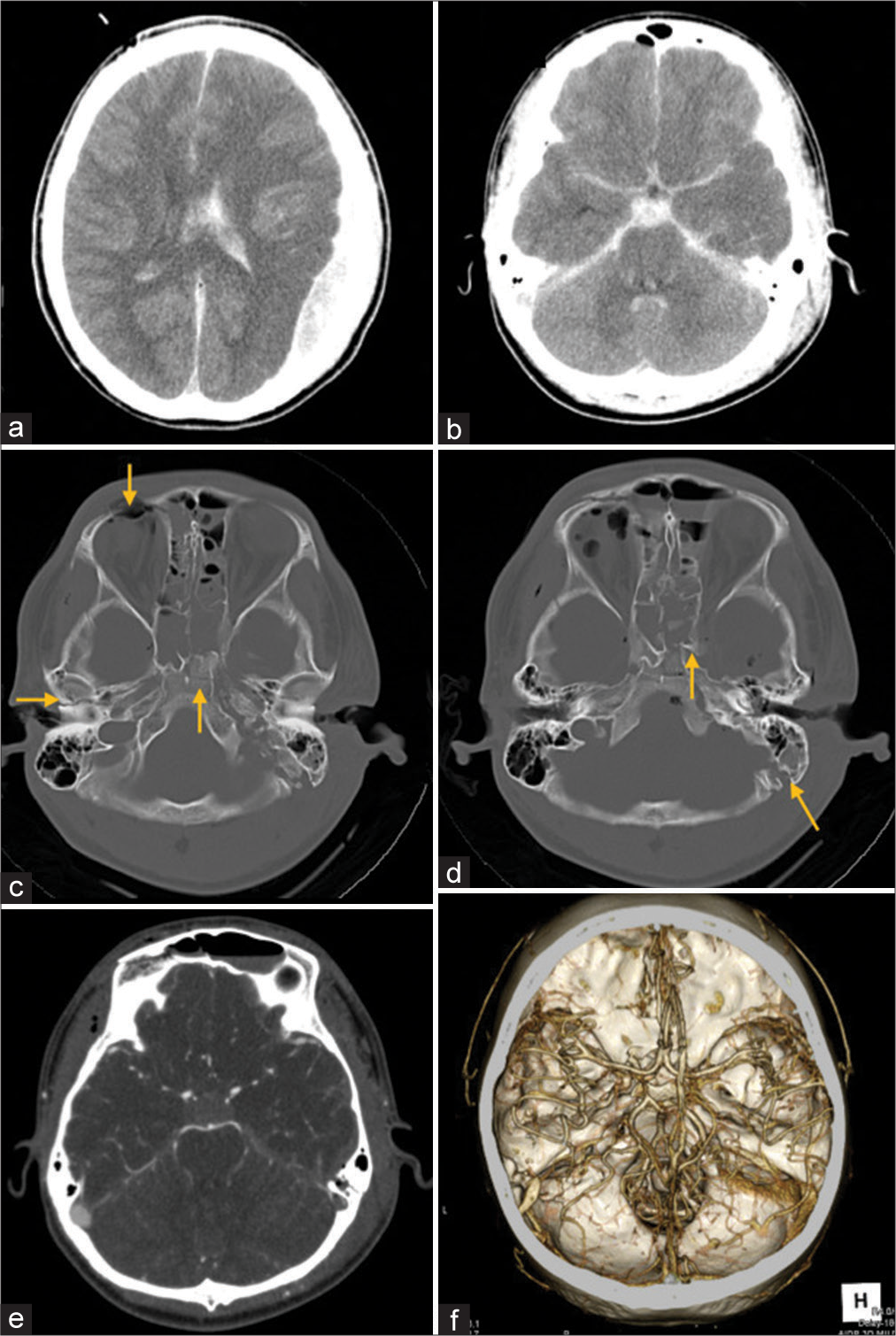
A 16-year-old boy presented to our emergency department after being hit by a car coming from the left while riding a bicycle at an intersection and being thrown off the road by approximately 10 m. The patient presented with a Glasgow coma scale (GCS) score of 4 (E1V2M1) with anisocoria (3.5/diffuse), and both direct and indirect light reflexes absent. Head computed tomography (CT) revealed multiple skull base fractures underlying traumatic subarachnoid hemorrhage and left acute epidural hematoma [
Figure 1:
Head computed tomography (CT) shows multiple skull base fractures underlying traumatic subarachnoid hemorrhage and left acute epidural hematoma (a and b). The skull fractures involve the right frontal bone, right pyramidal bone, clivus, left anterior clinoid process, and left mastoid process (c and d; orange arrow). Contrast-enhanced CT of the head shows no obvious aneurysm (e and f).
Emergency craniotomy was performed to remove the hematoma, and craniectomy was added for decompression. Postoperative management included deep sedation, hyperventilation, and hyperosmolar therapy to control intracranial pressure. Deep sedation was terminated on day 5, but the patient’s level of consciousness continued at a GCS score of 5T (E1VTM4).
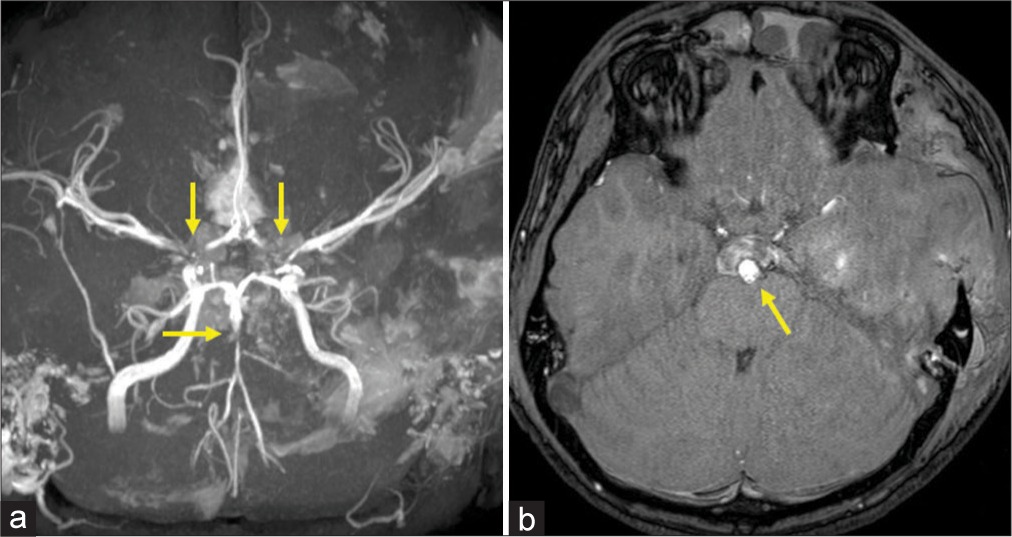
Head magnetic resonance imaging (MRI) was performed 7 days after surgery and revealed bilateral ICA stenosis, BA stenosis, and a pseudoaneurysm at the apical portion of the BA [
Figure 3:
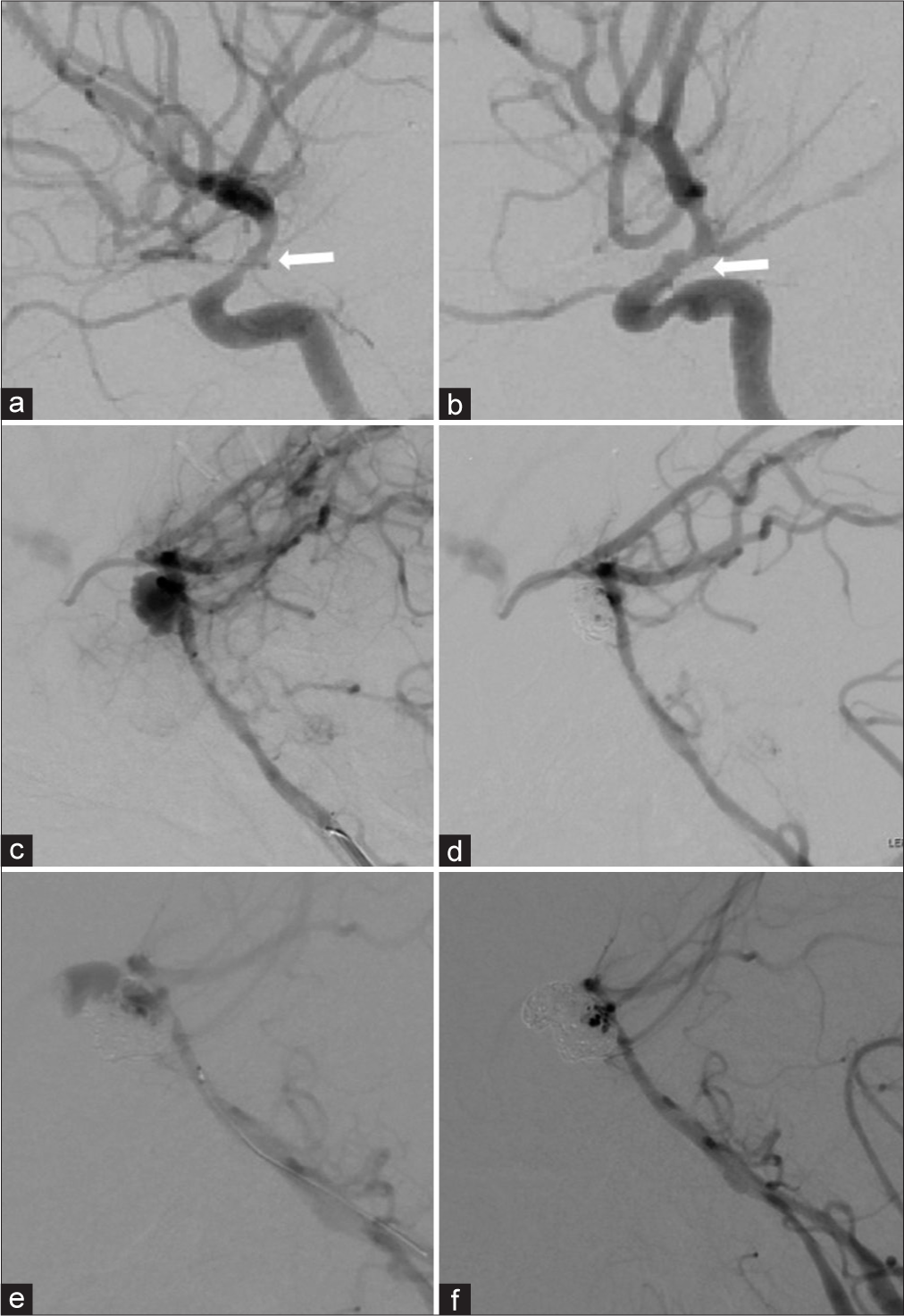
Digital subtraction angiography (DSA) revealed bilateral internal carotid artery stenosis (a and b; white arrow) and the aneurysm protruding irregularly anteriorly from the distal portion of basilar artery (BA) and proximal portion of the BA was dissected (c). The aneurysm gradually thrombosed, resulting in body filling and a volume embolization ratio of 15.7% (d). Second coil embolization was performed following DSA that revealed re-rupture of the aneurysm, resulting in body filling and a volume embolization ratio of 20.9% (e and f).
On day 35, that is, 28 days after coil embolization, head CT was performed for follow-up and revealed enlarged ventricles and intraventricular hemorrhage. A second coil embolization was performed following DSA, which revealed a rupture of the aneurysm, resulting in body filling and a volume embolization ratio of 20.9% [
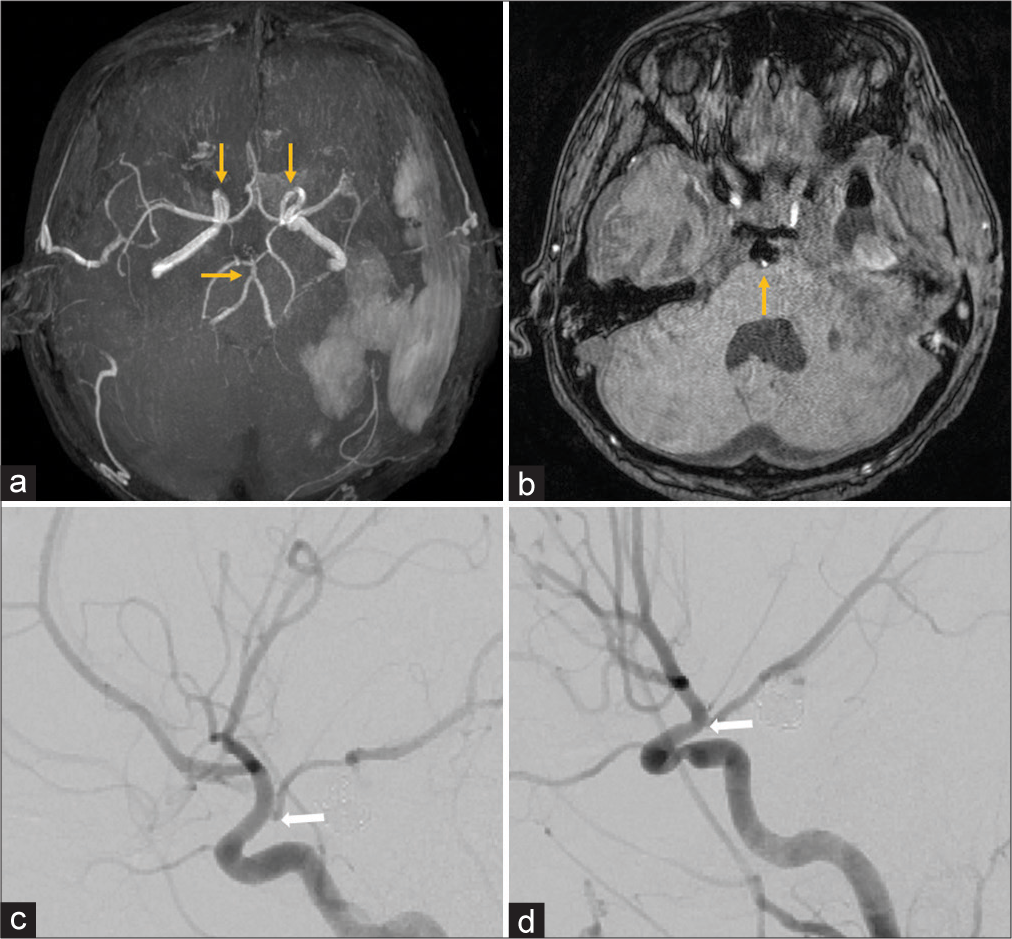
Head MRI on day 42, 1 week after retreatment, showed no obvious blood flow in the aneurysm, and the BA and bilateral ICA stenoses had improved [
Figure 4:
Head magnetic resonance imaging on day 42 showed no obvious blood flow in the aneurysm and the basilar artery stenosis and bilateral internal carotid artery stenosis had improved (a and b; orange arrow). Digital subtraction angiography also revealed improved bilateral internal carotid artery stenosis (c and d; white arrow).
DISCUSSION
The incidence of TICAs is lower than that of other aneurysms,[
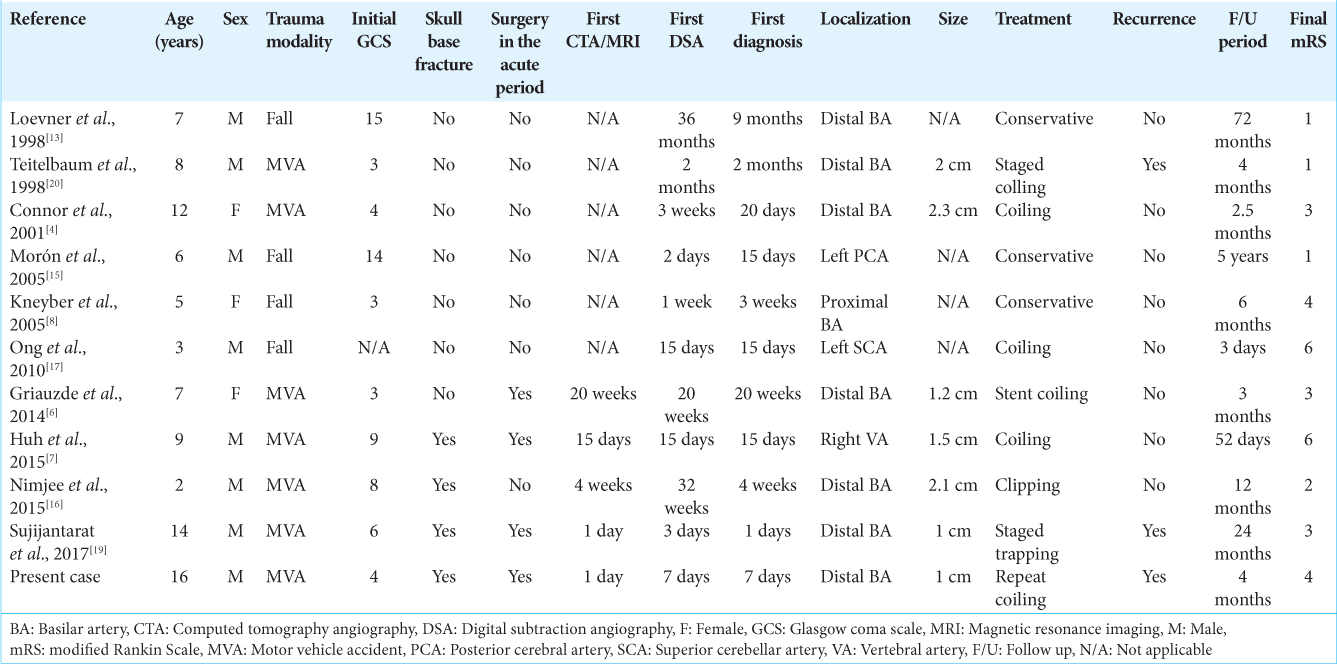
A pTICA in the posterior circulation secondary to blunt trauma is very rare, as the damaging artery is located deep in the brain and is expected to be caused by a large upright external force, with only few cases having been reported. To the best of our knowledge, ten cases of pTICAs in the posterior circulation have been reported after blunt head trauma [
Three recurrences were observed during angiographic follow-up of the eight treated aneurysms, with a recurrence rate of 37.5%. There were one and two recurrences in the microsurgery and endovascular treatment groups, respectively.[
Of all, 7 patients (63.6%) had a poor mRS score (≥3), denoting severe morbidity and mortality.[
CONCLUSION
We reported a pediatric case of traumatic BA pseudoaneurysm accompanied by bilateral traumatic ICA stenosis following severe head injury treated with repeated coil embolization. Past literature has indicated that pTICA has a high recurrence rate and may present severe morbidity and mortality. Early diagnosis, treatment, and detection of recurrence will require close follow-up after treatment and early consideration of DSA.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Aeron G, Abruzzo TA, Jones BV. Clinical and imaging features of intracranial arterial aneurysms in the pediatric population. Radiographics. 2012. 32: 667-81
2. Benoit BG, Wortzman G. Traumatic cerebral aneurysms. Clinical features and natural history. J Neurol Neurosurg Psychiatry. 1973. 36: 127-38
3. Buckingham MJ, Crone KR, Ball WS, Tomsick TA, Berger TS, Tew JM. Traumatic intracranial aneurysms in childhood: Two cases and a review of the literature. Neurosurgery. 1988. 22: 398-408
4. Connor SE, Martin AJ, Deasy NP, Jeffree MA, Strong AJ. Traumatic basilar pseudoaneurysm with a basilar-cavernous arteriovenous fistula. Neuroradiology. 2001. 43: 249-53
5. Dubey A, Sung WS, Chen YY, Amato D, Mujic A, Waites P. Traumatic intracranial aneurysm: A brief review. J Clin Neurosci. 2008. 15: 609-12
6. Griauzde J, Gemmete JJ, Chaudhary N, Pandey AS, Garton HJ. Basilar artery pseudoaneurysm presenting at 5-month follow-up after traumatic atlanto-occipital dislocation in a 7-year-old girl treated with intracranial stent placement and coiling. J Neurointerv Surg. 2014. 6: e8
7. Huh CW, Nam KH, Choi CH, Lee JI. Post traumatic pseudoaneurysm arising from V4 segment of vertebral artery: A case report. Korean J Neurotrauma. 2015. 11: 154-7
8. Kneyber MC, Rinkel GJ, Ramos LM, Tulleken CA, Braun KP. Early posttraumatic subarachnoid hemorrhage due to dissecting aneurysms in three children. Neurology. 2005. 65: 1663-5
9. Krings T, Geibprasert S, TerBrugge KG. Pathomechanisms and treatment of pediatric aneurysms. Childs Nerv Syst. 2010. 26: 1309-18
10. Kumar M, Kitchen ND. Infective and traumatic aneurysms. Neurosurg Clin N Am. 1998. 9: 577-86
11. Lasjaunias P, Wuppalapati S, Alvarez H, Rodesch G, Ozanne A. Intracranial aneurysms in children aged under 15 years: Review of 59 consecutive children with 75 aneurysms. Childs Nerv Syst. 2005. 21: 437-50
12. Li T, Zhang Y, Gu Z, Ma X, Yang X. Traumatic pseudoaneurysm of the basilar artery presenting with fatal epistaxis: A rare case report. Brain Inj. 2013. 27: 1316-9
13. Loevner LA, Ting TY, Hurst RW, Goldberg HI, Schut L. Spontaneous thrombosis of a basilar artery traumatic aneurysm in a child. AJNR Am J Neuroradiol. 1998. 19: 386-8
14. Lu J, Li M, Zhao Y, Zhao Y, Chen X, Zhao J. Paediatric intracranial aneurysms: Long-term angiographic and clinical outcomes in a contemporary series. Front Neurol. 2022. 13: 684093
15. Morón F, Benndorf G, Akpek S, Dempsy R, Strother CM. Spontaneous thrombosis of a traumatic posterior cerebral artery aneurysm in a child. AJNR Am J Neuroradiol. 2005. 26: 58-60
16. Nimjee SM, Smith TP, Kanter RJ, Ames W, Machovec KA, Grant GA. Rapid ventricular pacing for a basilar artery pseudoaneurysm in a pediatric patient: Case report. J Neurosurg Pediatr. 2015. 15: 625-9
17. Ong CK, Ong MT, Lam DV, Wenderoth JD. Catastrophic delayed rupture of a traumatic aneurysm of the distal superior cerebellar artery in a child. J Clin Neurosci. 2010. 17: 515-7
18. Quintana F, Diez C, Gutierrez A, Diez ML, Austin O, Vazquez A. Traumatic aneurysm of the basilar artery. AJNR Am J Neuroradiol. 1996. 17: 283-5
19. Sujijantarat N, Pierson MJ, Kemp J, Coppens JR. Staged trapping of traumatic basilar trunk pseudoaneurysm: Case report and review of literature. World Neurosurg. 2017. 108: 991.e7-12
20. Teitelbaum GP, Bernstein K, Choi S, Giannotta SL. Endovascular coil occlusion of a traumatic basilar-cavernous fistula: Technical report. Neurosurgery. 1998. 42: 1394-7
21. Uzan M, Cantasdemir M, Seckin MS, Hanci M, Kocer N, Sarioglu AC. Traumatic intracranial carotid tree aneurysms. Neurosurgery. 1998. 43: 1314-20 discussion 1320-22
22. Ventureyra EC, Higgins MJ. Traumatic intracranial aneurysms in childhood and adolescence. Case reports and review of the literature. Childs Nerv Syst. 1994. 10: 361-79
23. Yazbak PA, McComb JG, Raffel C. Pediatric traumatic intracranial aneurysms. Pediatr Neurosurg. 1995. 22: 15-9