- Department of Neurosurgery, Shinshu University School of Medicine, Matsumoto 390-8621, Japan
- Department of Neurosurgery, Nnamdi Azikiwe University Teaching Hospital, Nnewi, Anambra State, Nigeria
Correspondence Address:
Kiyoshi Ito
Department of Neurosurgery, Shinshu University School of Medicine, Matsumoto 390-8621, Japan
DOI:10.4103/sni.sni_238_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Sunday Patrick Nkwerem, Kiyoshi Ito, Shunsuke Ichinose, Tetsuyoshi Horiuchi, Kazuhiro Hongo. Resection and imbrication of symptomatic sacral Tarlov cysts: A case report and review of the literature. 04-Sep-2018;9:180
How to cite this URL: Sunday Patrick Nkwerem, Kiyoshi Ito, Shunsuke Ichinose, Tetsuyoshi Horiuchi, Kazuhiro Hongo. Resection and imbrication of symptomatic sacral Tarlov cysts: A case report and review of the literature. 04-Sep-2018;9:180. Available from: http://surgicalneurologyint.com/surgicalint-articles/8991/
Abstract
Background:Symptomatic Tarlov cysts are extremely rare, and there is no consensus regarding their optimal surgical management. Here, we encountered a patient with a symptomatic sacral Tarlov cyst and reviewed the appropriate literature.
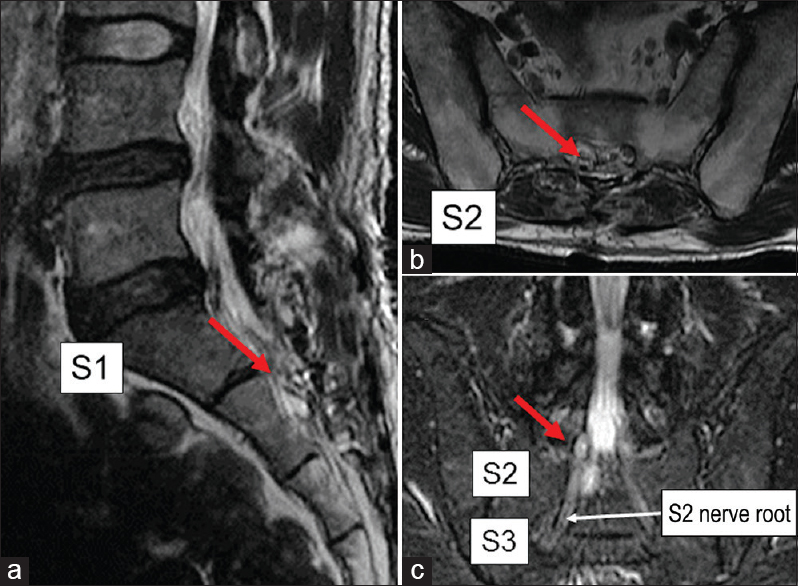
Case Description:A 40-year-old male presented with right lower extremity pain and hypoesthesia in the right S2 dermatome. The lumbosacral MR demonstrated a right S2 Tarlov cyst compressing the S2–S3 perineural sheaths. After the patient underwent microscopic cystectomy with obliteration of the subarachnoid connection to the cyst, the patient's symptoms resolved. Here, we reviewed our operative approach, and others proposed in the literature for the surgical management of these lesions.
Conclusions:Here, we present a 40-year-old male who was symptomatic from a right S2 Tarlov cyst compressing the S2–S3 perineural sheaths and successfully underwent microscopic cystectomy with obliteration of the subarachnoid connection. Additionally, the appropriate Tarlov cyst literature was reviewed.
Keywords: Cyst resection, perineural cyst, recurrence, surgical treatment, Tarlov cyst
INTRODUCTION
Tarlov cysts, first described by Tarlov in 1938, are perineural cysts often seen in the extradural segment involving the posterior sacral nerve roots.[
CASE REPORT
History
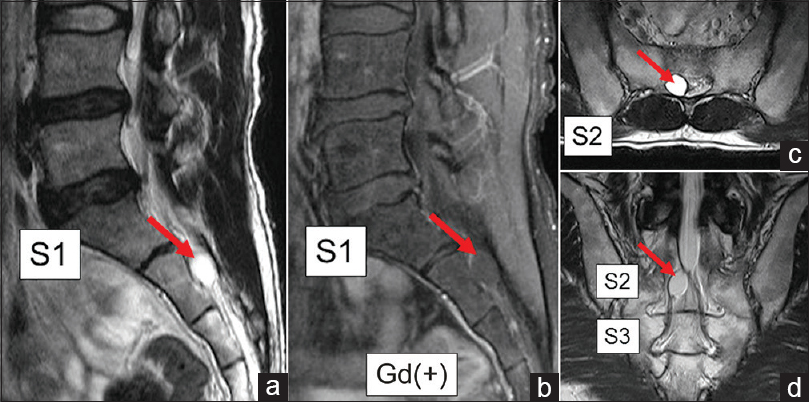
A 40-year-old male presented with a 3-year history of sensory changes involving the S2–S3 distribution in the right leg (e.g., hypoesthesia without motor weakness or dysuria). The lumbosacral MRI showed a noncontrast enhancing right-sided cystic mass at the S2–S3 level; it had the same intensity as CSF on both the T1- and T2-weighted images [
Figure 1
Lumbosacral magnetic resonance images. Sagittal (a and b), axial (c), and coronal (d) view of lumbosacral magnetic resonance imaging showing the cyst (red arrow) at the S2 vertebra. Preoperative magnetic resonance images showing a less-enhanced tumor (b). The contents of the cyst have the same intensity as the cerebrospinal fluid on both T2-weighted images
Operation
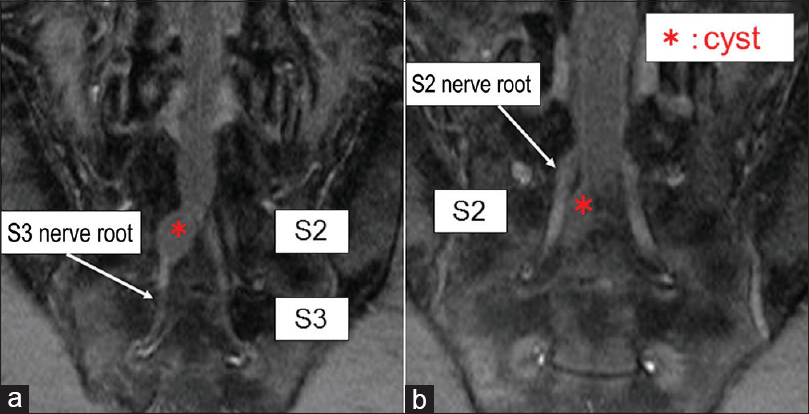
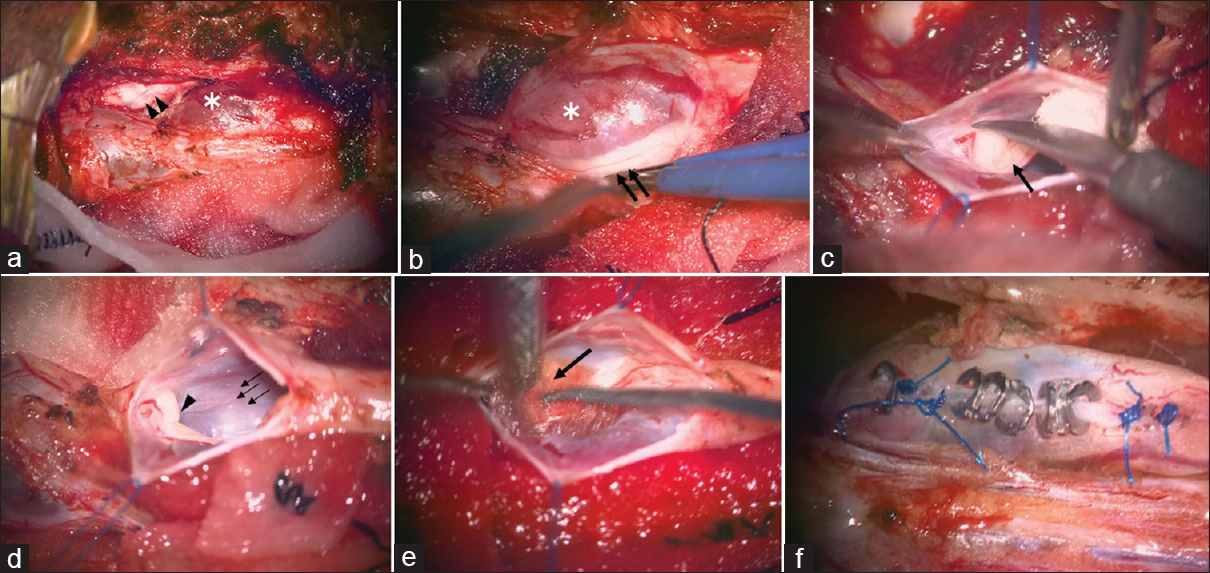
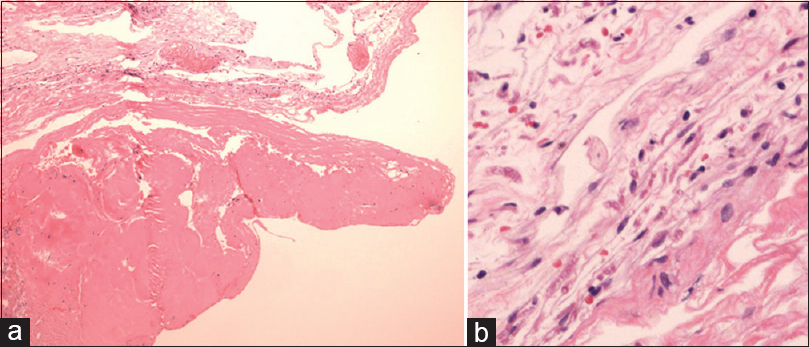
A laminoplastic laminotomy was performed at three levels using an ultrasonic bone curette. At surgery, the S3 nerve root was enveloped within cyst wall and the S2 nerve root was clearly compressed [Figure
Figure 3
Operative procedure and intraoperative findings. (a) Intraoperative photograph showing that the S2 nerve root (double arrowheads) was compressed by the cyst component (white asterisk). (b) Closer observation revealed that the cyst wall (white asterisk) contains the S3 nerve root (double arrows). (c and d) After excision of the cyst wall, the inlet of the cerebrospinal fluid (CSF) was confirmed around the nerve root (single arrow). The inlet from the subarachnoid space was found (single arrowhead) and the CSF was spontaneously flowing out from it (small triple arrows). A Valsalva maneuver clearly showed the CSF flow from the subarachnoid space to the perineural cyst. (e) After confirmation of the subarachnoid connection, it was sealed with adipose tissue (large arrow) and fibrin glue. (f) Finally, imbrication of the cyst wall was performed with nonpenetrating titanium clips. A repeated Valsalva maneuver showed no CSF leakage
DISCUSSION
Tarlov cysts are meningeal dilatations commonly found between the endoneurium and perineurium in the spinal nerve root sheaths at the S2 and S3 levels. They commonly communicate with the subarachnoid space. Some authors believe that these are a congenital lesions, whereas others consider them to be acquired.[
Symptomatic Tarlov cysts
Although they are typically asymptomatic, 1% may demonstrate growth and contribute to nerve root compression (e.g., sacral/perineal pain, sphincter dysfunction, radiculopathy, and rarely, infertility).[
Surgical options for symptomatic Tarlov cysts
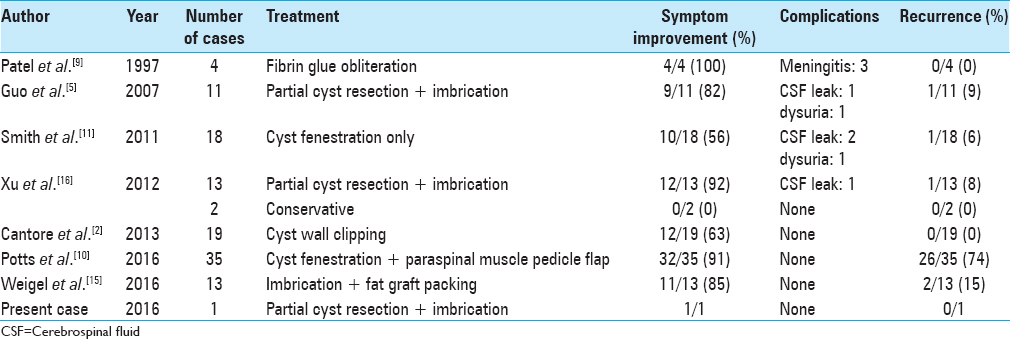
Different surgical treatment options are available for symptomatic Tarlov Cysts [
Studies demonstrating surgical outcomes of Tarlov cysts
Seven studies (all case series) evaluated the surgical treatment outcomes for Tarlov Cysts.[
CONCLUSION
There are several surgical treatment options for treating symptomatic (e.g., 1%) Tarlov cysts. An optimal strategy appears to include direct cyst resection, imbrication, and fat graft packing of the communication between the dural sac to the cyst (e.g., occlude the ball-valve mechanism of refilling).
Financial support and sponsorship
Japan Society for the Promotion of Science (JSPS) provided financial support in the form of Grants-in Aid for Scientific Research: KAKENHI. This work was supported by JSPS KAKENHI grant no. JP15 K10356.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors express their gratitude to our colleagues in the Department of Neurosurgery, Shinshu University School of Medicine, for their daily contributions to helping patients with Tarlov cysts.
References
1. Acosta FL, Quinones-Hinojosa A, Schmidt MH, Weinstein PR. Diagnosis and management of sacral tarlov cysts. Case report and review of the literature. Neurosurg Focus. 2003. 15: E15-
2. Cantore G, Bistazzoni S, Esposito V, Tola S, Lenzi J, Passacantilli E. Sacral tarlov cyst: Surgical treatment by clipping. World Neurosurg. 2013. 79: 381-9
3. Caspar W, Papavero L, Nabhan A, Loew C, Ahlhelm F. Microsurgical excision of symptomatic sacral perineurial cysts: A study of 15 cases. Surg Neurol. 2003. 59: 101-5
4. Chaiyabud P, Suwanpratheep K. Symptomatic tarlov cyst: Report and review. J Med Assoc Thai. 2006. 89: 1047-50
5. Guo D, Shu K, Chen R, Ke C, Zhu Y, Lei T. Microsurgical treatment of symptomatic sacral perineurial cysts. Neurosurgery. 2007. 60: 1059-65
6. Langdown AJ, Grundy JR, Birch NC. The clinical relevance of tarlov cysts. J Spinal Disord Tech. 2005. 18: 29-33
7. Lucantoni C, Than KD, Wang AC, Valdivia-Valdivia JM, Maher CO, La Marca F. Tarlov cysts: A controversial lesion of the sacral spine. Neurosurg Focus. 2011. 31: E14-
8. Park HJ, Kim IS, Lee SW, Son BC. Two cases of symptomatic perineural cysts (tarlov cysts) in one family: A case report. J Korean Neurosurg Soc. 2008. 44: 174-7
9. Patel MR, Louie W, Rachlin J. Percutaneous fibrin glue therapy of meningeal cysts of the sacral spine. AJR Am J Roentgenol. 1997. 168: 367-70
10. Potts MB, McGrath MH, Chin CT, Garcia RM, Weinstein PR. Microsurgical fenestration and paraspinal muscle pedicle flaps for the treatment of symptomatic sacral tarlov cysts. World Neurosurg. 2016. 86: 233-42
11. Smith ZA, Li Z, Raphael D, Khoo LT. Sacral laminoplasty and cystic fenestration in the treatment of symptomatic sacral perineural (Tarlov) cysts: Technical case report. Surg Neurol Int. 2011. 2: 129-
12. Tani S, Hata Y, Tochigi S, Ohashi H, Isoshima A, Nagashima H. Prevalence of spinal meningeal cyst in the sacrum. Neurol Med Chir (Tokyo). 2013. 53: 91-4
13. Tarlov IM. Perineural cysts of the spinal roots. Arch Neurol Psychiatry. 1938. 40: 1067-74
14. Voyadzis JM, Bhargava P, Henderson FC. Tarlov cysts: A study of 10 cases with review of the literature. J Neurosurg. 2001. 95: 25-32
15. Weigel R, Polemikos M, Uksul N, Krauss JK. Tarlov cysts: Long-term follow-up after microsurgical inverted plication and sacroplasty. Eur Spine J. 2016. 25: 3403-10
16. Xu J, Sun Y, Huang X, Luan W. Management of symptomatic sacral perineural cysts. PLoS One. 2012. 7: e39958-






Cory B.
Posted February 13, 2020, 9:16 pm
I recently was diagnosed with Tarlov Cyst disorder and have done extensive reviews of treatment options after only being referred to physical therapy. In my reviews I found your page and given your findings, and my symptoms (13 years now), I present as the 1% you are referring to; indicated on my recent MRI.
The cyst sits at the S3, I also show indications of a possible Neurofibroma at the S2(I was diagnosed at age 5 with Neurofibromatosis Type 1 after my right fibia failed to grow 1in in length leaving a gap; this was repaired by Dr. Spear at UMC Medical Center when he,” Rolled it like a cigarret and molded it in,” after removing part of my pelvic bone for the repair; his words not mine).
If possible could I send a copy of my images to be reviewed and given a 2nd opinion on the correct treatment after showing obvious symptoms for over 10+ years? Thank you for your time and dedication to solving these life altering ailments.