- Department of Neurosurgery, Medical College of Wisconsin, Milwaukee, WI, USA
Correspondence Address:
Ha Son Nguyen
Department of Neurosurgery, Medical College of Wisconsin, Milwaukee, WI, USA
DOI:10.4103/2152-7806.173571
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nguyen HS, Oni-Orisan A, Cochran J, Pollock G. Resection of a recurrent cervical internal carotid artery pseudoaneurysm after failed endovascular therapy. Surg Neurol Int 07-Jan-2016;7:
How to cite this URL: Nguyen HS, Oni-Orisan A, Cochran J, Pollock G. Resection of a recurrent cervical internal carotid artery pseudoaneurysm after failed endovascular therapy. Surg Neurol Int 07-Jan-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/resection-of-a-recurrent-cervical-internal-carotid-artery-pseudoaneurysm-after-failed-endovascular-therapy/
Abstract
Background:Recurrence of a cervical internal carotid artery (ICA) pseudoaneurysm initially treated by endovascular means is rare. We report an instance where a patient returned with a recurrent, enlarging cervical ICA pseudoaneursym, 15 years after initial complete, endovascular occlusion of the ICA.
Case Description:Patient is a 64-year-old male with a history of a right cervical ICA pseudoaneurysm diagnosed 15 years ago after a car accident. At the time, he received endovascular occlusion of his right ICA. Recent serial imaging demonstrated progressive enlargement of his pseudoaneurysm, up to 6 cm × 5 cm × 5.5 cm, without evidence of internal flow or extravasation. Due to dysphagia and hoarseness, resection of the pseudoaneurysm was recommended. Dissection occurred down to the lesion, where its borders were skeletonized. Its stump at the proximal ICA was mobilized and clamped; the lesion was incised and the existing thrombus, as well as the coil mass, was removed. The distal ICA appeared completely scarred with no retrograde filling. There were branches from the external carotid artery that appeared to supply the pseudoaneurysm. The scarred remnant of the distal ICA was sutured and the stump at the proximal ICA was ligated. Once hemostasis was obtained, closure occurred via anatomical layers. Postoperatively, the patient woke up well; at discharge, he exhibited no respiratory distress or dysphagia. At 5 months follow-up, a computed tomography angiography of the neck revealed no evidence for a residual pseudoaneurysm. He continues on lifelong aspirin.
Conclusion:Recurrence of a cervical ICA pseudoaneursym is rare. We caution that such a clinical scenario is possible, even 15 years after endovascular occlusion of the ICA. Branches from the external carotid artery may feed the pseudoaneursym and cause recurrence. This mechanism has not been reported. Perhaps longer clinical follow-up is necessary, especially if endovascular therapy is the initial treatment option.
Keywords: Carotid pseudoaneurysm, endovascular therapy, recurrent pseudoaneurysm
INTRODUCTION
A pseudoaneurysm of the cervical internal carotid artery (ICA) is uncommon. The most frequent etiology is trauma. Other etiologies include upper respiratory tract infections,[
CASE PRESENTATION
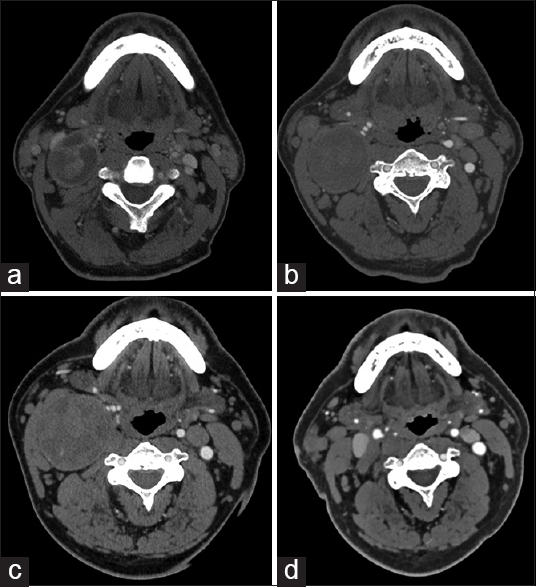
Patient is a 64-year-old male with a history of a right ICA pseudoaneurysm diagnosed 15 years ago after a car accident. At the time, he received endovascular occlusion of his right ICA. Recent serial imaging demonstrated progressive enlargement of his pseudoaneurysm, up to 6 cm × 5 cm × 5.5 cm [Figure
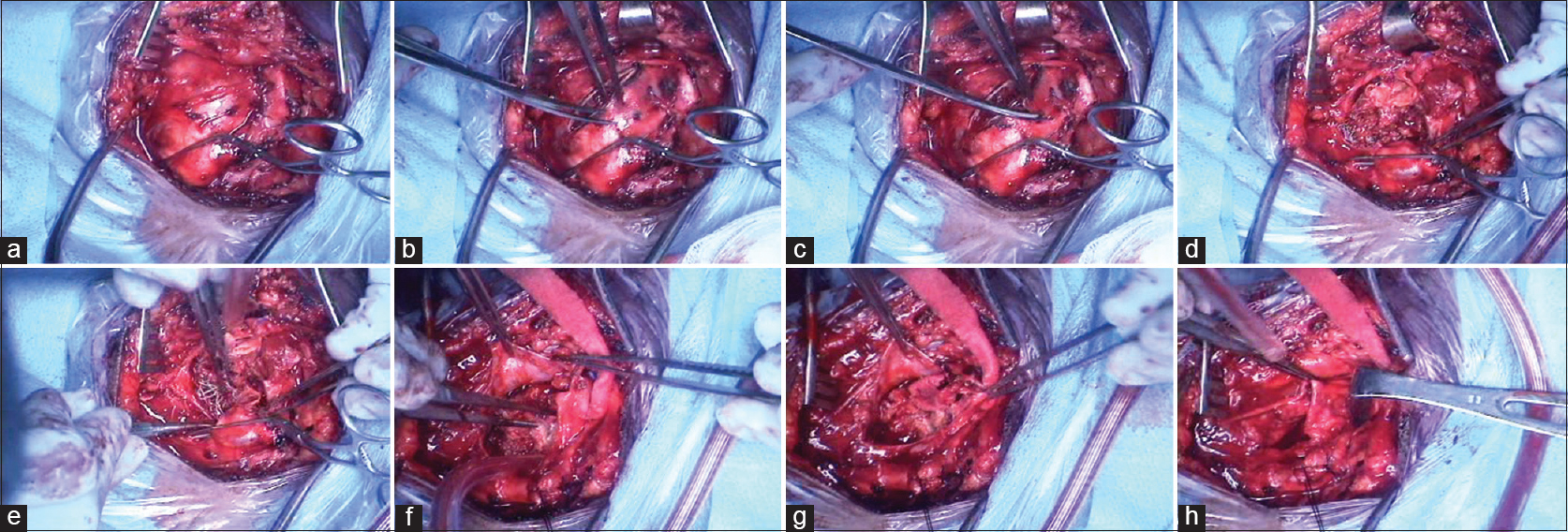
An incision was made over the anterior aspect of the sternocleidomastoid muscle. Dissection occurred in the normal fashion, with exposure of the common facial vein, the jugular vein, and the anterior aspect of the sternocleidomastoid muscle. Deeper dissection revealed the large pseudoaneurysm, as well as the common and external branches of the carotid artery [
Postoperatively, the patient woke up well with a baseline neurological exam; at discharge, he exhibited no respiratory distress or dysphagia. At 5 months follow-up, the patient noted some mild, persistent neck pain, likely from neuropathy due to the surgical dissection. A computed tomography angiography (CTA) of the neck revealed no evidence for a residual pseudoaneurysm [
DISCUSSION
The most common cause of ICA pseudoaneurysm is blunt trauma, where the pathology is under the umbrella term “blunt cerebrovascular injury” (BCVI). The incidence of BCVI ranges between 1.2% and 2.70% of patients with blunt injuries.[
BCVI is classified based on severity.[
Possible endovascular options include balloon embolization, coil embolization, stand-alone-stenting (typically with a covered stent), stent-assisted coiling, and flow diversion. Various studies have short-term follow-up, typically from 6 months to 2 years.[
CONCLUSION
Recurrence of a cervical ICA pseudoaneursym is rare. We caution that such a clinical scenario is possible, even 15 years after endovascular occlusion of the ICA. Branches from the external carotid artery may feed the pseudoaneursym and cause recurrence. Perhaps longer clinical follow-up is necessary, especially if endovascular therapy is the initial treatment option.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Baker A, Rizk H, Carroll W, Lambert P. Cervical internal carotid artery pseudoaneurysm complicating malignant otitis externa:First case report. Laryngoscope. 2015. 125: 733-5
2. Bien AG, Cress MC, Nguyen SB, Westgate SJ, Nanda A. Endovascular treatment of a temporal bone pseudoaneurysm presenting as bloody otorrhea. J Neurol Surg Rep. 2013. 74: 88-91
3. Choudhri O, Heit J, Do HM. Endovascular reconstruction of enlarging traumatic internal carotid artery pseudoaneurysm. Neurosurg Focus. 2014. 37: 1-
4. da Silva PS, Waisberg DR. Internal carotid artery pseudoaneurysm with life-threatening epistaxis as a complication of deep neck space infection. Pediatr Emerg Care. 2011. 27: 422-4
5. Dang NV, Hai NT, Cuong TC. Recurrent carotico-cavernous fistula after internal carotid artery ligation: A case with embolization of the fistula via contralateral internal carotid artery approach. Interv Neuroradiol. 2014. 20: 482-6
6. Defillo A, Zelensky A, Pulivarthi S, Lowary JL, Nussbaum ES, Lassig JP. Non-infected carotid artery pseudoaneurysm 29 years after endarterectomy, endovascular management with covered stent. J Neurosurg Sci. 2012. 56: 145-9
7. Ellens DJ, Hurley MC, Surdel D, Shaibani A, Pelzer H, Bendok BR. Radiotherapy-induced common carotid pseudoaneurysm presenting with initially occult upper airway hemorrhage and successfully treated by endovascular stent graft. Am J Otolaryngol. 2010. 31: 195-8
8. Gupta V, Niranjan K, Rawat L, Gupta AK. Stent-graft repair of a large cervical internal carotid artery pseudoaneurysm causing dysphagia. Cardiovasc Intervent Radiol. 2009. 32: 558-62
9. Hacein-Bey L, Blazun JM, Jackson RF. Carotid artery pseudoaneurysm after orthognathic surgery causing lower cranial nerve palsies: Endovascular repair. J Oral Maxillofac Surg. 2013. 71: 1948-55
10. Hamasaki O, Ikawa F, Hidaka T, Kurokawa Y, Yonezawa U. Extracranial internal carotid artery pseudoaneurysm associated with neurofibromatosis type 1 treated with endovascular stenting and coil embolization. Vasc Endovascular Surg. 2014. 48: 176-9
11. Jagetia A, Sharma D, Singh D, Sinha S, Ganjoo P, Narang P. Endovascular occlusion of cervical internal carotid artery pseudoaneurysm in a child treated by N-butyl cyanoacrylate: A rare case report. Pediatr Neurosurg. 2015. 50: 168-72
12. Jao SY, Weng HH, Wong HF, Wang WH, Tsai YH. Successful endovascular treatment of intractable epistaxis due to ruptured internal carotid artery pseudoaneurysm secondary to invasive fungal sinusitis. Head Neck. 2011. 33: 437-40
13. Koyanagi M, Nishi S, Hattori I, Horikawa F, Iwasaki K. Stent-supported coil embolization for carotid artery pseudoaneurysm as a complication of endovascular surgery – case report. Neurol Med Chir (Tokyo). 2004. 44: 544-7
14. Makeieff M, Pelliccia P, Mondain M, Machi P. Pseudoaneurysm of the internal carotid artery complicating deep neck space infection. J Pediatr. 2010. 157: 510-
15. Mascitelli JR, De Leacy RA, Oermann EK, Skovrlj B, Smouha EE, Ellozy SH. Cervical-petrous internal carotid artery pseudoaneurysm presenting with otorrhagia treated with endovascular techniques. J Neurointerv Surg. 2015. 7: e25-
16. Meher R, Garg A, Malhotra V, Singh I. Pseudoaneurysm of the internal carotid artery in an infant aged 8 months. N Z Med J. 2006. 119: U1815-
17. Mordekar SR, Bradley PJ, Whitehouse WP, Goddard AJ. Occult carotid pseudoaneurysm following streptococcal throat infection. J Paediatr Child Health. 2005. 41: 682-4
18. Petar P, Slobodan T, Srdjan B, Dragoslav N, Djordje R. Extracranial internal carotid artery pseudoaneurysms after kinking reconstruction. Vascular. 2010. 18: 356-62
19. Rahal JP, Gao B, Safain MG, Malek AM. Stent recanalization of carotid tonsillar loop dissection using the enterprise vascular reconstruction device. J Clin Neurosci. 2014. 21: 1141-7
20. Ramesh A, Muthukumarassamy R, Karthikeyan VS, Rajaraman G, Mishra S. Pseudoaneurysm of internal carotid artery after carotid body tumor excision. Indian J Radiol Imaging. 2013. 23: 208-11
21. Requejo F, Sierre S, Lipsich J, Zuccaro G. Endovascular treatment of post-pharyngitis internal carotid artery pseudoaneurysm with a covered stent in a child: A case report. Childs Nerv Syst. 2013. 29: 1369-73
22. Sankararaman S, Velayuthan S, Gonzalez-Toledo E. Internal carotid artery stenosis as the sequela of a pseudoaneurysm after methicillin-resistant Staphylococcus aureus infection. Pediatr Neurol. 2012. 47: 312-4
23. Seth R, Obuchowski AM, Zoarski GH. Endovascular repair of traumatic cervical internal carotid artery injuries: A safe and effective treatment option. AJNR Am J Neuroradiol. 2013. 34: 1219-26
24. Sibtain N, Shah J, Johnson D, Clifton A. Treatment of a recurrent internal carotid artery pseudoaneurysm with the wallgraft endoprosthesis. Interv Neuroradiol. 2006. 12: 165-70
25. Singhal M, Gupta V, Singh P, Lal A, Behra A, Khandelwal N. Iatrogenic life-threatening pseudoaneurysms of extracranial internal carotid artery after fine-needle aspiration of cervical lymph nodes: Report of two cases in children. Cardiovasc Intervent Radiol. 2009. 32: 1260-3
26. Vávrová M, Slezácek I, Vávra P, Karlová P, Procházka V. Pseudoaneurysm of the left internal carotid artery following tonsillectomy. Vasa. 2011. 40: 491-4
27. Wang W, Li MH, Li YD, Gu BX, Wang J, Zhang PL. Treatment of traumatic internal carotid artery pseudoaneurysms with the Willis covered stent: A prospective study. J Trauma. 2011. 70: 816-22
28. Yeh CH, Lin MS, Chiu MC, Chen CH, Pai YL. Endovascular treatment of a huge cervical carotid artery pseudoaneurysm with wallgraft prosthesis. Ann Vasc Surg. 2011. 25: 265.e1-3
29. Zaghlool D, Franz R. Treatment of a high large extracranial carotid artery pseudoaneurysm from trauma using a viabahn graft. Ann Vasc Surg. 2015. 29: 837.e1-7
30. Zelenák K, Zelenáková J, DeRiggo J, Kurca E, Kantorová E, Polácek H. Treatment of cervical internal carotid artery spontaneous dissection with pseudoaneurysm and unilateral lower cranial nerves palsy by two silk flow diverters. Cardiovasc Intervent Radiol. 2013. 36: 1147-50