- Department of Neurosurgery, University of Louisville, Louisville, Kentucky, United States.
DOI:10.25259/SNI_400_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Zaid Aljuboori, Emily Sieg. Resolution of cauda equina syndrome after surgical extraction of lumbar intrathecal bullet. 25-Jul-2020;11:214
How to cite this URL: Zaid Aljuboori, Emily Sieg. Resolution of cauda equina syndrome after surgical extraction of lumbar intrathecal bullet. 25-Jul-2020;11:214. Available from: https://surgicalneurologyint.com/surgicalint-articles/10150/
Abstract
Background: Gunshot wound (GSW) injuries to the spinal column are correlated with potentially severe neurological damage. Here, we describe a GSW to the thoracolumbar junction (e.g., T12/L1 level) which resulted in a cauda equina syndrome that resolved once the bullet was removed.
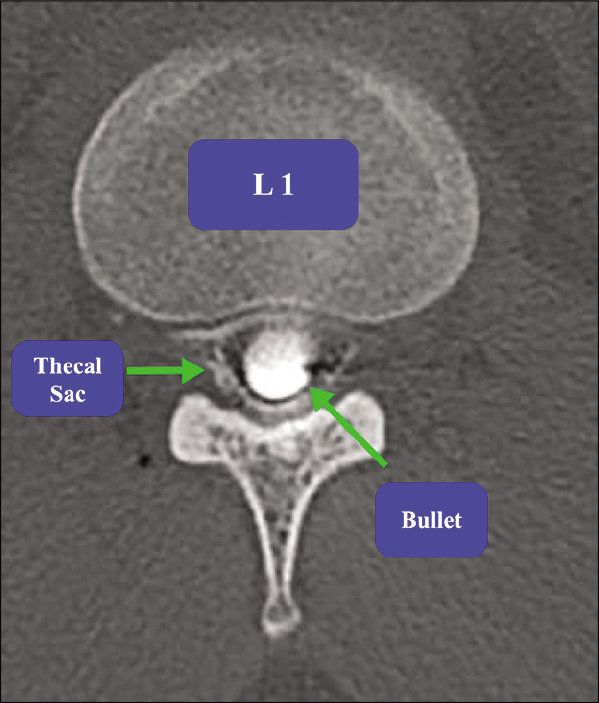
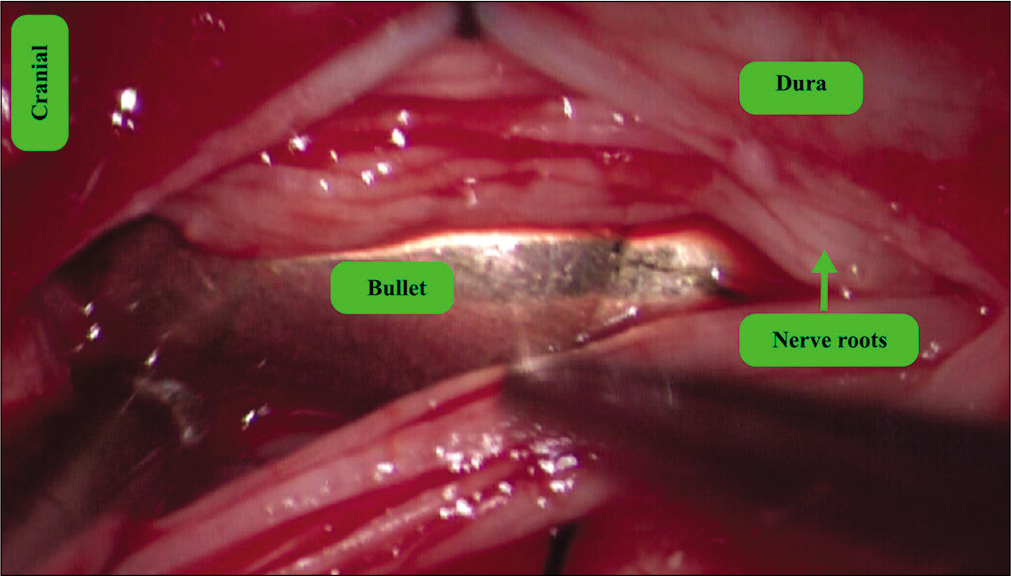
Case Description: A 29-year-old male presented with a T12-L1 GSW; the bullet traversed the right chest and liver, entered the spinal canal at T12, and then settled at L1. He experienced excruciating burning pain in the right lower extremity/perineum and had urinary retention. On neurological examination, he exhibited severe weakness of the right iliopsoas/quadriceps (2/5) and extensor hallucis longus (1/5) which had decreased sensation in the right lower extremity in all dermatomes and urinary retention. The myelogram showed the bullet lodged intrathecally at L1; it compressed the cauda equina. Immediately after, the bullet was extracted and at 8 weeks follow-up, the patient’s right-sided motor function normalized, the sensory findings improved, and the sphincteric dysfunction resolved; the only residual deficit was minimal residual numbness in the L2-L5 distributions.
Conclusion: Twenty percent of penetrating spinal column injuries are attributed to GSW s. The location of these injuries best determines the neurological damage and degree of recovery. Since patients with incomplete cauda equina syndromes have favorable prognoses, removal of bullets involving the T12-S1 levels may prove beneficial.
Keywords: Bullet, Cauda equine, Gunshot, Intrathecal
INTRODUCTION
There are no clear guidelines regarding the surgical management of penetrating injuries of the spinal column (PISC) attributed to ballistic or stab injuries.[
CASE DESCRIPTION
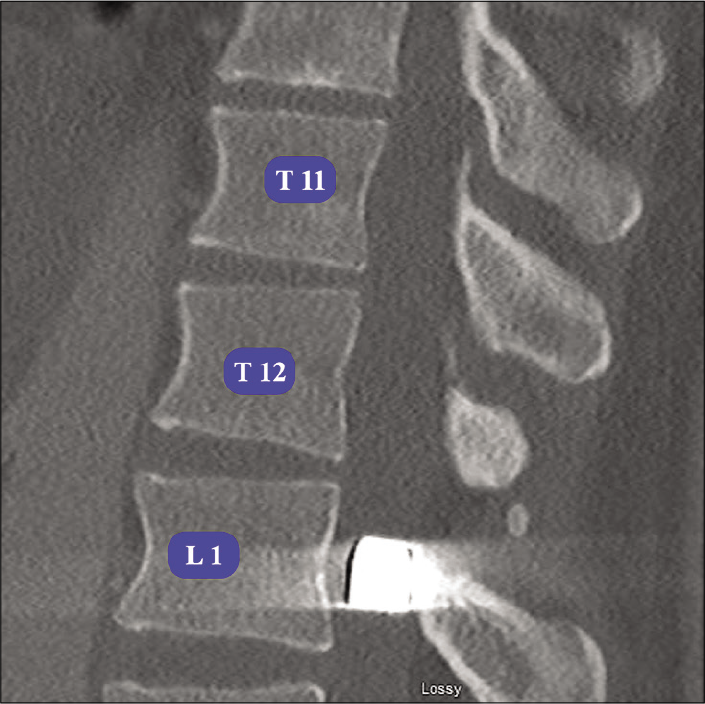
A 29-year-old male sustained a GSW to the chest. The CT scan documented the bullet traversed the lung and liver, entered the spinal canal at T12 anterior to the psoas muscle (e.g., resulting in a nondisplaced fracture of the right facet joint), and settled intrathecally at L1 [
DISCUSSION
Despite their frequency, the management of PISC remains controversial.[
Indications for surgery with incomplete CES
Incomplete CES has a favorable prognosis with early surgery/ decompression, while complete injuries carry a poorer prognosis with or without surgery.[
CONCLUSION
With GSW/PISC to the thoracolumbar junction, patients presenting with incomplete CES and radiographic documentation of bullet fragments lodged within the spinal canal should be considered for early surgical decompression and bullet removal.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Crutcher CL, Wilson JM, DiGiorgio AM, Fannin ES, Shields JA, Morrow KD. Minimally invasive management of civilian gunshot wounds to the lumbar spine: A case series and technical report. Oper Neurosurg (Hagerstown). 2020. p. opaa030-
2. Gutierrez A, Su YS, Vaughan KA, Miranda S, Chen HI, Petrov D. Penetrating spinal column injuries (pSI): An institutional experience with 100 consecutive cases in an urban trauma center. World Neurosurg. 2020. 138: e551-6
3. Hoeritzauer I, Wood M, Copley PC, Demetriades AK, Woodfield J. What is the incidence of cauda equina syndrome? A systematic review. J Neurosurg Spine. 2020. 32: 1-10
4. Morrow KD, Podet AG, Spinelli CP, Lasseigne LM, Crutcher CL, Wilson JD. A case series of penetrating spinal trauma: Comparisons to blunt trauma, surgical indications, and outcomes. Neurosurg Focus. 2019. 46: E4-
5. Patil R, Jaiswal G, Gupta TK. Gunshot wound causing complete spinal cord injury without mechanical violation of spinal axis: Case report with review of literature. J Craniovertebr Junction Spine. 2015. 6: 149-57
6. Penn-Barwell JG, Brown KV, Fries CA. High velocity gunshot injuries to the extremities: Management on and off the battlefield. Curr Rev Musculoskelet Med. 2015. 8: 312-7
7. Rider IS, Marra EM.editors. Cauda Equina and Conus Medullaris Syndromes. Treasure Island, FL: StatPearls; 2020. p.