- Clinical Professor of Neurosurgery, School of Medicine, State University of NY at Stony Brook, and Editor-in-Chief Surgical Neurology International NY and ℅ Dr. Marc Agulnick 1122 Frankllin Avenue Suite 106, Garden City, NY 11530, USA,
- Assistant Clinical Professor of Orthopedics, NYU Langone Hospital, Long Island, NY, USA. 1122 Franklin Avenue Suite 106 Garden City, NY 11530, USA
Correspondence Address:
Nancy E. Epstein, M.D., F.A.C.S, Clinical Professor of Neurosurgery, School of Medicine, State University of NY at Stony Brook, and Editor-in-Chief Surgical Neurology International NY and ℅ Dr. Marc Agulnick 1122 Frankllin Avenue Suite 106, Garden City, NY 11530, USA.
DOI:10.25259/SNI_992_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein1, Marc A. Agulnick2. Review of anterior cervical diskectomy/fusion (ACDF) using different polyetheretherketone (PEEK) cages. 25-Nov-2022;13:556
How to cite this URL: Nancy E. Epstein1, Marc A. Agulnick2. Review of anterior cervical diskectomy/fusion (ACDF) using different polyetheretherketone (PEEK) cages. 25-Nov-2022;13:556. Available from: https://surgicalneurologyint.com/surgicalint-articles/12019/
Abstract
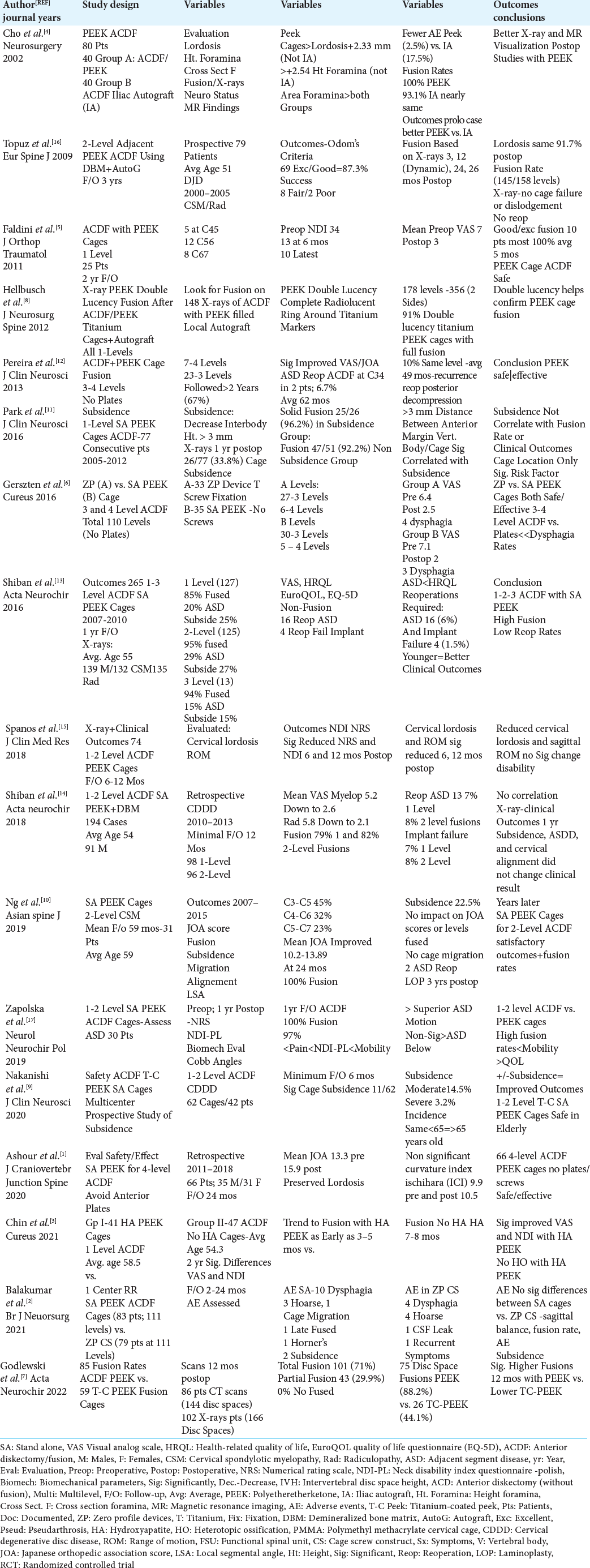
Background: Multiple anterior cervical diskectomy/fusion (ACDF) techniques now use a variety of Polyehteretherketone (PEEK) cages; stand-alone (SA) and zero-profile (ZP) with/without screws, cages filled with demineralized bone matrix/autograft, and cages coated with hydroxyapatite or titanium. We compared the safety/ efficacy between different PEEK ACDF cage constructs in 17 studies, and in some cases, additionally contrasted results with “routine” ACDF (i.e. series/historical data performed with combinations of iliac autograft/allograft and plates).
Methods: We focused on the clinical outcomes, fusion rates, postoperative radiographic changes/lordosis/ subsidence, and/or reoperation rates for various PEEK ACDF constructs vs. “routine” ACDF.
Results: One to 3 and 4-level PEEK ACDF cages demonstrated high fusion rates, few cage failures, and low reoperation rates. Subsidence for PEEK ACDF cages did not reduce fusion rates or diminish the quality of postoperative outcomes. Further, titanium-coated (T-C) PEEK cages lowered fusion rates in one study (i.e. 44.1% fusions vs. 88.2% for routine PEEK ACDF) while ACDF PEEK cages coated with hydroxyapatite (HA) showed only a “trend” toward enhanced arthrodesis.
Conclusion: One to 3-4 multilevel ACDF PEEK cage constructs demonstrated comparable safety/efficacy when compared with each other, or in select cases, with “routine” ACDF (i.e. using autograft/allograft and plates).
Keywords: Anterior cervical diskectomy fusion (ACDF), Cages, Complications, Fusion rates, Hydroxyapatite Coated (HA), Outcomes, Polyetheretherketone (PEEK), Screws, Stand-Alone (SA), Subsidence, Titanium-Coated (T-C), Zero Profile (ZP)
INTRODUCTION
Multiple anterior cervical diskectomy/fusion (ACDF) Polyetheretherketone (PEEK) cage constructs/techniques are now available. Their various designs include; Stand Alone (SA) or Zero Profile (ZP) cages with/without screws, cages filled with demineralized bone matrix (DBM) and/or autograft, and PEEK cages coated with hydroxyapatite or titanium [
Methods
Seventeen studies focused on the safety/efficacy between different ACDF PEEK cage constructs with occasional comparisons to “routine” ACDF controls [
Cho et al. Study from 2002 Fusion Rates and Complications for PEEK ACDF vs. Iliac Autograft ACDF
Cho et al. (2002) compared the complications, fusion rates, and outcomes for 40 patients undergoing ACDF with PEEK cages vs. 40 having ACDF utilizing iliac crest autograft (IA) [
Results of 1-Level PEEK ACDF
Several 1-level PEEK ACDF studies showed good/excellent postoperative results with high fusion rates [
Results of 1 to 2-Level PEEK ACDF
Multiple 1 to 2-level PEEK ACDF studies also demonstrated high fusion rates and improved outcomes [
Results of 2-Level PEEK ACDF
Several 2-level PEEK ACDF studies verified high fusion rates and better outcomes with these constructs [
Results of 3-4 Level PEEK ACDF
Several other series additionally documented the safety/ efficacy of 3 and 4-level PEEK ACDF [
Results of Zero Profile PEEK Cages vs. Stand Alone PEEK Cages for 3-4 Level ACDF
Zero Profile (ZP) PEEK ACDF, comprised of a radiolucent polyetheretherketone (PEEK) cage with an anterior titanium 4 hole plate for screw placement, were developed to avoid complications of anterior cervical plates, while maintaining stability (i.e. of interbody cages with plates). Two studies confirmed excellent results with ZP PEEK ACDF devices [
Lower Fusion Rates for Titanium-Coated (T-C) PEEK ACDF vs. PEEK ACDF Alone
In 2022, Godlewski et al. compared fusion rates for 85 PEEK ACDF cages vs. 59 T-C PEEK ACDF cages.[
Subsidence Rates Following Single or Multilevel PEEK ACDF Cage Constructs Varying from Stand-Alone Devices to Titanium-Coated (T-C) PEEK Cages
Several studies documented various postoperative subsidence rates (i.e. defined as a decrease in interbody height of >3 mm on X-rays at 1-year postoperatively) following single to multilevel PEEK ACDF cage procedures [
Double Lucency X-ray Sign of Titanium-Coated PEEK ACDF (Plus Autograft) Fusion
Hellbusch et al.(2012) described the double lucency sign for confirming fusion based on X-rays performed in 148 patients undergoing 1-level Titanium-Coated (T-C) PEEK ACDF cage fusions filled with autograft [
CONCLUSION
Comparison between multiple types of ACDF PEEK cage constructs and select instances of “routine” ACDF largely demonstrated comparable safety/efficacy for these procedures.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ashour AM, Abdelmohsen I, Sawy ME, Toubar AF. Stand-alone polyetheretherketone cages for anterior cervical discectomy and fusion for successive four-level degenerative disc disease without plate fixation. J Craniovertebr Junction Spine. 2020. 11: 118-23
2. Balakumar B, Raju S, Maraconi SD, Hassan MF. A pragmatic single centre retrospective comparative review of complication profile between PEEK cages and zero-P cage screw constructs. Br J Neurosurg. 2021. p. 1-7
3. Chin KR, Gohel NN, Aloise DM, Seale JA, Pandey DK, Pencle FJ. Effectiveness of a fully impregnated hydroxyapatite polyetheretherketone cage on fusion in anterior cervical spine surgery. Cureus. 2021. 13: e17457
4. Cho DY, Liau WR, Lee WY, Liu JT, Chiu CL, Sheu PC. Preliminary experience using a polyetheretherketone (PEEK) cage in the treatment of cervical disc disease. Neurosurgery. 2002. 51: 1343-9
5. Faldini C, Chehrassan M, Miscione MT, Acri F, d’Amato M, Pungetti C. Single-level anterior cervical discectomy and interbody fusion using PEEK anatomical cervical cage and allograft bone. J Orthop Traumatol. 2011. 12: 201-5
6. Gerszten PC, Paschel E, Marhalay H, Sabry H, Jalalod”din H, Saoud K. Outcomes evaluation of zero-profile devices compared to stand-alone PEEK cages for the treatment of three-and four-level cervical disc disease. Cureus. 2016. 8: e775
7. Godlewski B, Bebenek A, Dominiak M, Karpinski G, Cieslik P, Pawelczyk . PEEK versus titanium-coated PEEK cervical cages: Fusion rate. Acta Neurochir (Wien). 2022. 164: 1501-7
8. Hellbusch LC, Spangler WJ, Bowder A. Radiographic PEEK double-lucency finding after anterior cervical discectomy and fusion with local autograft and PEEK spacer: A preliminary study. J Neurosurg Spine. 2012. 16: 248-50
9. Nakanishi Y, Naito K, Yamagata T, Yoshimura M, Shimokawa N, Nishikawa M. Safety of anterior cervical discectomy and fusion using titanium-coated polyetheretherketone stand-alone cages: Multicenter prospective study of incidence of cage subsidence. J Clin Neurosci. 2020. 74: 47-54
10. Ng EP, Yip AS, Wan KH, Tse MS, Wong KK, Kwok TK. Stand-alone cervical cages in 2-level anterior interbody fusion in cervical spondylotic myelopathy: Results from a minimum 2-year follow-up. Asian Spine J. 2019. 13: 225-32
11. Park JY, Choi KY, Moon BJ, Hur H, Jang JW, Lee JK. Subsidence after single-level anterior cervical fusion with a stand-alone cage. J Clin Neurosci. 2016. 33: 83-8
12. Pereira EA, Chari A, Hempenstall J, Leach JC, Chandran H, Cadoux-Hudson TA. Anterior cervical discectomy plus intervertebral polyetheretherketone cage fusion over three and four levels without plating is safe and effective long-term. J Clin Neurosci. 2013. 20: 1250-5
13. Shiban E, Gapon K, Wostrack M, Meyer B, Lehmberg . Clinical and radiological outcome after anterior cervical discectomy and fusion with stand-alone empty polyetheretherketone (PEEK) cages. Acta Neurochir (Wien). 2016. 158: 349-55
14. Shiban E, Nies M, Kogler J, Kogler L, da Cunha PR, Meyer B. No correlation between radiological and clinical outcome 1 year following cervical arthrodesis. Acta Neurochir (Wien). 2018. 160: 845-53
15. Spanos SL, Siasios I, Dimopoulos VG, Paterakis KN, Mastrogiannis DS, Giannis TP. Correlation of clinical and radiological outcome after anterior cervical discectomy and fusion with a polyetheretherketone cage. J Clin Med Res. 2018. 10: 268-27
16. Topuz K, Colak A, Kaya S, Simsek H, Kutlay M, Nusret M. Two-level contiguous cervical disc disease treated with peek cages packed with demineralized bone matrix: Results of 3-year follow-up. Eur Spine J. 2009. 18: 238-43
17. Zapolska G, Kwaitkowski M, Turek G, Mariak Z, Hermanowicz A. Biomechanical evaluation of single-and multi-level anterior cervical discectomy and fusion with polyetheretherketone cages: Radiological and clinical outcomes. Neurol Neurochir Pol. 2019. 53: 358-62