- Professor of Clinical Neurosurgery, School of Medicine, State University of New York at Stony Brook, New York, and Chief of Neurosurgical Spine and Education, NYU Winthrop Hospital, NYU Winthrop NeuroScience/Neurosurgery, Mineola, New York 11501, United States.
DOI:10.25259/SNI_559_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein. Review of Risks and Complications of Extreme Lateral Interbody Fusion (XLIF). 06-Dec-2019;10:237
How to cite this URL: Nancy E. Epstein. Review of Risks and Complications of Extreme Lateral Interbody Fusion (XLIF). 06-Dec-2019;10:237. Available from: http://surgicalneurologyint.com/surgicalint-articles/9786/
Abstract
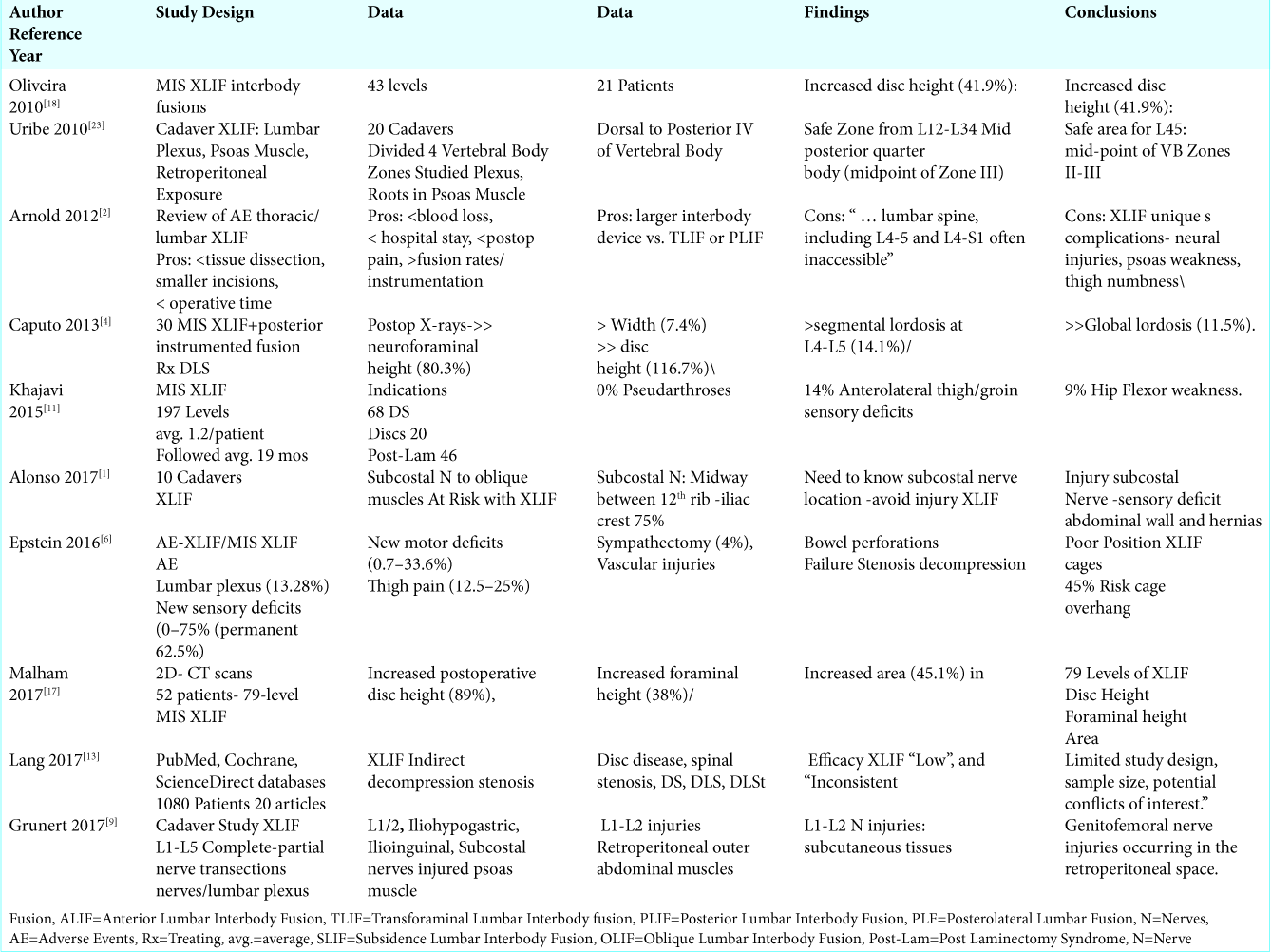
Background: Extreme lateral interbody fusions (XLIF) and Minimally Invasive (MIS) XLIF were developed to limit the vascular injuries associated with anterior lumbar interbody fusion (ALIF), and minimize the muscular/ soft tissue trauma attributed to transforaminal lumbar interbody fusion (TLIF), posterior lumbar interbody fusion (PLIF), and posterolateral lumbar fusion (PLF).
Methods: Nevertheless, XLIF/MIS XLIF pose significant additional risks and complications that include; multiple nerve injuries (e.g. lumbar plexus, ilioinguinal, iliohypogastric, genitofemoral, lateral femoral cutaneous, and subcostals (to the anterior abdominal muscles: abdominal oblique), and sympathectomy), major vascular injuries, bowel perforations/postoperative ileus, seromas, pseudarthrosis, subsidence, and reoperations.
Results: The risks of neural injury with XLIF/MIS XLIF (up to 30-40%) are substantially higher than for TLIF, PLIF, PLF, and ALIF. These neural injuries included: lumbar plexus injuries (13.28%); new sensory deficits (0-75% (21.7%-40%); permanent 62.5%); motor deficits (0.7-33.6%-40%); iliopsoas weakness (9%-31%: permanent 5%), anterior thigh/groin pain (12.5-34%), and sympathectomy (4%-12%). Additional non-neurological complications included; subsidence (10.3%-13.8%), major vascular injuries (0.4%), bowel perforations, recurrent seroma, malpositioning of the XLIF cages, a 45% risk of cage-overhang, pseudarthrosis (7.5%), and failure to adequately decompress stenosis. In one study, reviewing 20 publications and involving 1080 XLIF patients, the authors observed “Most (XLIF) studies are limited by study design, sample size, and potential conflicts of interest.”
Conclusion: Many new neurological deficits and other adverse events/complications are attributed to MIS XLIF/ XLIF. Shouldn’t these significant risk factors be carefully taken into consideration before choosing to perform MIS XLIF/XLIF?
Keywords: Extreme lateral interbody fusion (XLIF): Complications, Lumbar plexus injuries, Major injuries, Minor injuries, Nerve root injuries
INTRODUCTION
Extreme lateral interbody fusions (XLIFs) and Minimally Invasive (MIS) XLIF were devised to reduce the vascular injuries seen with anterior lumbar interbody fusions (ALIF), and limit the muscular/soft tissue trauma seen with transforaminal lumbar interbody fusion (TLIF), posterior lumbar interbody fusion (PLIF), and posterolateral lumbar fusion (PLF). Further, XLIF/MIS XLIF uniquely contributed to multiple new major neurological injuries(10%-40%) to the lumbar plexus, ilioinguinal, iliohypogastric, genitofemoral, lateral femoral cutaneous, and subcostal nerves [
Arguments Favoring XLIF/MIS XLIF with/without Supplemental Posterior Instrumentation
XLIF/MIX XLIF With/Without Instrumentation
Minimally Invasive (MIS) Extreme Lateral Interbody Fusion and XLIF (XLIF” NuVasive Inc San Diego CA) were developed to provide interbody fusion, indirect neural decompression, and stabilization. These XLIF/MIS XLIF approaches would theoretically limit the major vascular/visceral injuries seen with ALIF, and avoid the paraspinal/soft tissue trauma observed with TLIF, PLIF, and PLF. Further, potential benefits included; smaller incisions, reduced blood loss, shorter operative time, increased disc space height, reduced infection rates, shorter length of stay (LOS), higher fusion rates, reduced subsidence rates, less postoperative pain, and lower reoperation rates [
Anatomic Studies Showing Nerves at Risk with XLIF
However, multiple anatomic/cadaveric studies demonstrated how MIS XLIF/XLIF involving dissection through the psoas muscle, placed the lumbar plexus, ilioinguinal, iliohypogastric, genitofemoral, lateral femoral cutaneous, and subcostal nerves at risk.[
Definition of Safe Working Zone for XLIF
In 2010, Uribe et al. attempted to define the “safe working zones” for MIS XLIF in a series of 20 cadavers [
Subcostal Nerve Injury with XLIF
In a cadaveric study, Alonso et al. (2017) observed how the subcostal nerve that typically innervates the anterolateral abdominal muscles (e.g. abdominal oblique muscle), if injured during XLIF, could contribute to abdominal wall hernias [
XLIF Results in Complete or Partial Nerve Transections
In a cadaver study (15 cadavers, 26 sides), Grunert et al. (2017) analyzed complete/partial nerve injuries/transections to the lumbar plexus occurring during L1-L5 XLIF [
Clinical Injuries with XLIF
Multiple neurological and other injuries were clinically observed following XLIF/MIS XLIF.[
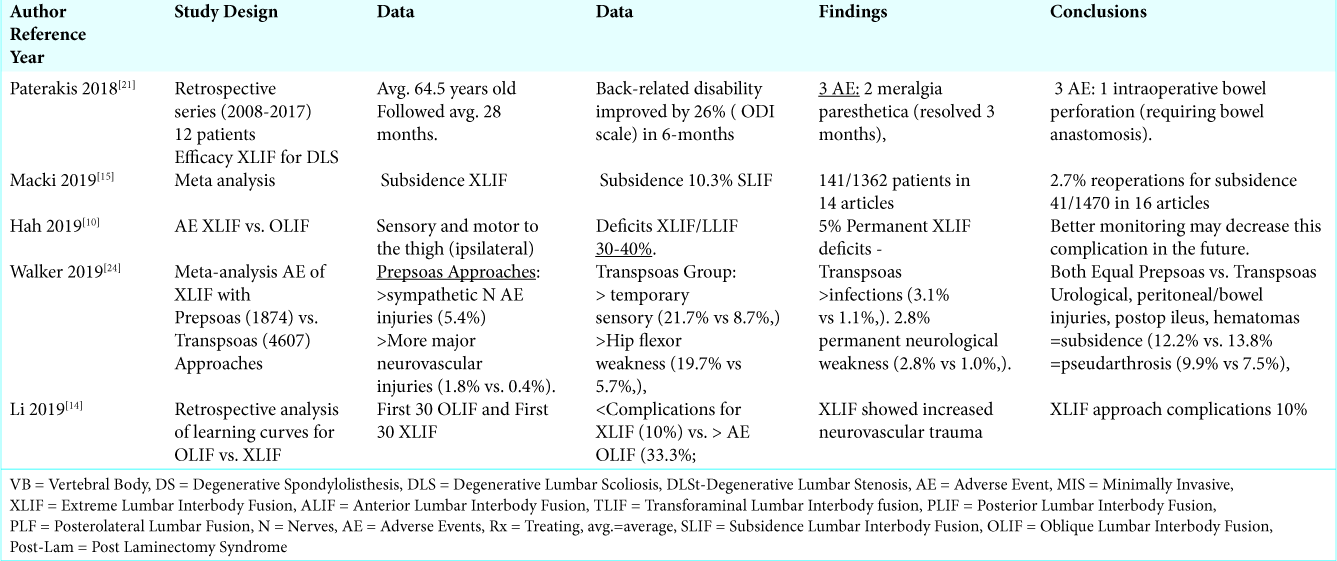
Meta-analysis of Complications of XLIF with Prepsoas vs. Transpsoas Approaches
In 2019, Walker et al. performed a meta-analysis of the complications of XLIF utilizing the prepsoas (1874 patients) vs. transpsoas (4607 patients) approaches.[
XLIF Unreliable Extent of Decompression
Using the PubMed, Cochrane, and ScienceDirect databases, Lang et al. (2017) determined that XLIF failed to provide adequate indirect decompression of central and lateral recess stenosis (e.g. decompression for disc disease, spinal stenosis, spondylolisthesis, and degenerative scoliosis) [
XLIF Resulting in Meralgia Paresthetica and Bowel Perforation
In 2018, Paterakis et al. (study years 2008-2017) retrospectively studied the efficacy of XLIF for treating degenerative scoliosis involving 12 patients averaging 64.5 years of age, and followed for 28 months [
XLIF Subsidence Rate
In a meta-analysis of XLIF, reviewing 14 articles and involving 1362 patients, Macki et al. (2019) found a 10.3% subsidence rate (141/1362 patients) that warranted a 2.7% incidence of reoperations (N = 41/1470 patients in 16 articles) [
Learning Curve for XLIF
In a retrospective analysis of the learning curve (e.g. complications/outcomes) for the first 30 oblique lumbar interbody fusion (OLIF) vs. the first 30 XLIF, Li et al. (2019) found there were fewer complications for XLIF (10%) vs. OLIF (33.3%; increased neurovascular trauma). Nevertheless, XLIF still resulted in a 10% significant complication rate [
Adjacent Segment Disease/Post Laminectomy Syndrome with XLIF
XLIF/MIS XLIF were often utilized to address adjacent segment disease and/or post laminectomy syndromes. When Khajavi et al. (2015) evaluated outcomes of MIS XLIF (197 levels; average 1.2/patient) at 19 postoperative months addressing degenerative spondylolisthesis (n = 68) and disc disease (n = 20), they found 26 new instances of adjacent segment disease, and 46 cases of post- laminectomy syndrome [
3 Cases of L1-L2 Disc Herniations Treated with MIS XLIF Utilizing CT Guidance
Oyelese et al. (2018) evaluated three MIS XLIF performed at the L1-L2 level addressing disc disease and stenosis.[
Modifications and Surgical Alternatives to XLIF
Endoscopic XLIF
Schonauer et al. (2017) noted the following risks for the classical XLIF: (the XLIF) “deep and tight surgical corridor makes visual identification of important landmark structures, as well as sufficient endplate and contralateral preparation, challenging” [
XLIF: Open vs. Percutaneous Screw Fusion in Adult Degenerative Scoliosis
Attenello et al. (2018) retrospectively evaluated 22 XLIF performed with open vs. percutaneous screws fixation for the management of adult degenerative scoliosis (ADScoli) over an average of 22 postoperative months [
Comparing Mini Open TLIF vs. XLIF for Degenerative Lumbar Spondylolisthesis
Kono et al. (2018) demonstrated the comparable safety/efficacy of XLIF (XLIF: 20 patients) vs. mini-open transforaminal lumbar interbody fusion (TLIF: 20 patients) for treating lumbar degenerative spondylolisthesis [
CONCLUSION
There are multiple neurological and other surgical risks associated with MIS XLIF/XLIF. The resultant nerve injuries included; the lumbar plexus, iliohypogastric, ilioinguinal, genitofemoral, subcostal, lateral femoral cutaneous nerves, meralgia paresthetica and sympathectomy [
References
1. Alonso F, Graham R, Rustagi T, Drazin D, Loukas M, Oskouian RJ. The Subcostal Nerve During Lateral Approaches to the Lumbar Spine: An Anatomical Study with Relevance for Injury Avoidance and Postoperative Complications Such as Abdominal Wall Hernia. World Neurosurg. 2017. 104: 669-673
2. Arnold PM, Anderson KK, McGuire RA. The lateral transpsoas approach to the lumbar and thoracic spine: A review. Surg Neurol Int. 2012. 3: S198-215
3. Attenello J, Chang C, Lee YP, Zlomislic V, Garfin SR, Allen RT. Comparison of lateral lumbar interbody fusion (LLIF) with open versus percutaneous screw fixation for adult degenerative scoliosis. J Orthop. 2018. 15: 486-489
4. Caputo AM, Michael KW, Chapman TM, Jennings JM, Hubbard EW, Isaacs RE. Extreme lateral interbody fusion for the treatment of adult degenerative scoliosis. J Clin Neurosci. 2013. 20: 1558-63
5. Epstein NE. Extreme lateral lumbar interbody fusion: Do the cons outweigh the pros?. Surg Neurol Int. 2016. 7: S692-S700
6. Epstein NE. Non-neurological major complications of extreme lateral and related lumbar interbody fusion techniques. Surg Neurol Int. 2016. 7: S656-S659
7. Epstein NE. High neurological complication rates for extreme lateral lumbar interbody fusion and related techniques: A review of safety concerns. Surg Neurol Int. 2016. 7: S652-S655
8. Goodnough LH, Koltsov J, Wang T, Xiong G, Nathan K, Cheng I. Decreased estimated blood loss in lateral trans-psoas versus anterior approach to lumbar interbody fusion for degenerative spondylolisthesis. J Spine Surg. 2019. 5: 185-193
9. Grunert P, Drazin D, Iwanaga J, Schmidt C, Alonso F, Moisi M. Injury to the Lumbar Plexus and its Branches After Lateral Fusion Procedures: A Cadaver Study. World Neurosurg. 2017. 105: 519-525
10. Hah R, Kang HP. Lateral and Oblique Lumbar Interbody Fusion-Current Concepts and a Review of Recent Literature. Curr Rev Musculoskelet Med. 2019. 22: 305-310
11. Khajavi K, Shen A, Lagina M, Hutchison A. Comparison of clinical outcomes following minimally invasive lateral interbody fusion stratified by preoperative diagnosis. Eur Spine J. 2015. 24: 322-30
12. Kono Y, Gen H, Sakuma Y, Koshika Y. Comparison of Clinical and Radiologic Results of Mini-Open Transforaminal Lumbar Interbody Fusion and Extreme Lateral Interbody Fusion Indirect Decompression for Degenerative Lumbar Spondylolisthesis. Asian Spine J. 2018. 12: 356-364
13. Lang G, Perrech M, Navarro-Ramirez R, Hussain I, Pennicooke B, Maryam F. Potential and Limitations of Neural Decompression in Extreme Lateral Interbody Fusion-A Systematic Review. World Neurosurg. 2017. 101: 99-113
14. Li J, Wang X, Sun Y, Zhang F, Gao Y, Li Z. Safety Analysis of Two Anterior Lateral Lumbar Interbody Fusions at the Initial Stage of Learning Curve. World Neurosurg. 2019. 127: e901-e909
15. Macki M, Anand SK, Surapaneni A, Park P, Chang V. Subsidence Rates After Lateral Lumbar Interbody Fusion: A Systematic Review. World Neurosurg. 2019. 122: 599-606
16. Malham GM, Parker RM, Goss B, Blecher CM, BaX . Indirect foraminal decompression is independent of metabolically active facet arthropathy in extreme lateral interbody fusion. Spine. 2014. 39: E1303-10
17. Malham GM, Ellis NJ, Parker RM, Blecher CM, White R, Goss B, Seex KA. Maintenance of Segmental Lordosis and Disk Height in Stand-alone and Instrumented Extreme Lateral Interbody Fusion (XLIF). Clin Spine Surg. 2017. 30: E90-E98
18. Oliveira L, Marchi L, Coutinho E, Pimenta L. A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine. 2010. 35: S331-7
19. Ono K, Ohmori K, Hori T.editors. Clinical and Radiological Outcomes of Corrective Surgery on Adult Spinal Deformity Patients: Comparison of Short and Long Fusion. Adv Orthop. 2019. 2019: 9492486-
20. Oyelese AA, Fridley J, Choi DB, Telfeian A, Gokaslan ZL. Minimally invasive direct lateral, retroperitoneal transforaminal approach for large L1-2 disc herniations with intraoperative CT navigational assistance: technical note and report of 3 cases. J Neurosurg Spine. 2018. 29: 46-53
21. Paterakis KN, Brotis AG, Paschalis A, Tzannis A, Fountas KN. Extreme lateral lumbar interbody fusion (XLIF) in the management of degenerative scoliosis: a retrospective case series. J Spine Surg. 2018. 4: 610-615
22. Schonauer C, Stienen MN, Gautschi OP, Schaller K, Tessitore E. Endoscope-Assisted Extreme-Lateral Interbody Fusion: Preliminary Experience and Technical Note. World Neurosurg. 2017. 103: 869-875.e3
23. Uribe JS, Arredondo N, Dakwar E, Vale FL. Defining the safe working zones using the minimally invasive lateralretroperitoneal transpsoas approach: an anatomical study. J Neurosurg Spine. 2010. 13: 260-6
24. Walker CT, Farber SH, Cole TS, Xu DS, Godzik J, Whiting AC. Complications for minimally invasive lateral interbody arthrodesis: a systematic review and meta-analysis comparing prepsoas and transpsoas approaches. J Neurosurg Spine. 2019. 25: 1-15






Toni Ketterman
Posted June 15, 2023, 7:35 am
I would be interested in updated information regarding the XLIFT procedure