- Department of Neurosurgery, Faculty of Medicine, Kindai University, Osaka, Japan
- Department of Neurosurgery, Kubota Clinic Neurosurgery, Osaka, Japan.
Correspondence Address:
Yasuhiro Sanada, Department of Neurosurgery, Faculty of Medicine, Kindai University, Osaka, Japan.
DOI:10.25259/SNI_577_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yasuhiro Sanada1, Kiyoshi Tsuji1, Yuumi Hamada1, Kazuhiro Fujishima1, Kentaro Furukawa1, Norihito Fukawa1, Hisashi Kubota2, Tetsu Satow1, Jun C. Takahashi1. Rigid but nonmetallic cranioplasty after pterional craniotomy: Technical note. 15-Sep-2023;14:337
How to cite this URL: Yasuhiro Sanada1, Kiyoshi Tsuji1, Yuumi Hamada1, Kazuhiro Fujishima1, Kentaro Furukawa1, Norihito Fukawa1, Hisashi Kubota2, Tetsu Satow1, Jun C. Takahashi1. Rigid but nonmetallic cranioplasty after pterional craniotomy: Technical note. 15-Sep-2023;14:337. Available from: https://surgicalneurologyint.com/surgicalint-articles/12550/
Abstract
Background: Given the popularity of pterional craniotomy, numerous modifications have been made to prevent postoperative deformities. With the advent of titanium plates, fixation has become both simple and excellent. However, titanium plates can cause skin problems, infection, or cause skull growth to fail.
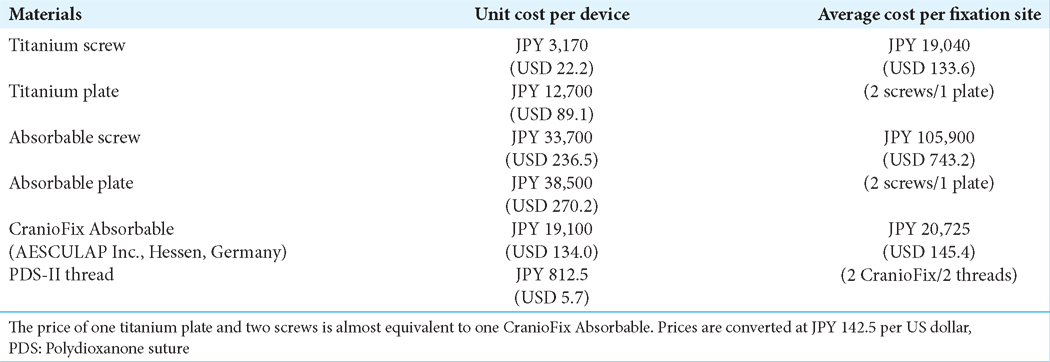
Methods: To develop a simple, cost-effective, and esthetically satisfactory fixation method, without the use of non-metallic materials, six young and older patients underwent pterional craniotomy. CranioFix Absorbable clamps were used to fix the bone flap in the frontal and temporal regions such that the frontal part was in close contact with the skull. After fixation, the bone chips and bone dust were placed in the bone gap and fixed with fibrin glue. We measured the computed tomography values of the reconstructed area and thickness of the temporal profiles postoperatively over time.
Results: Bone fusion was achieved in all patients by 1 year after surgery. Both the thickness of the temporalis muscle and the thickness of the temporal profile had changed within 2 mm as compared with the preoperative state.
Conclusion: Our simple craniotomy technique, gentle tissue handling, and osteoplastic cranioplasty yielded satisfactory esthetic results and rigidness in pterional craniotomy.
Keywords: Absorbable materials, Autologous bone dust, Fibrin glue, Non-metallic cranioplasty, Pterional craniotomy
INTRODUCTION
Pterional craniotomy was widely introduced by Yaşargil et al. in the 1960s.[
To overcome these issues, we developed a simple, cost-effective, and esthetically satisfactory fixation method for use in adult patients, which does not require the use of any non-absorbable materials.
MATERIALS AND METHODS
This study was approved by the Ethics Committee of our institute, and written informed consent was obtained from all the patients included in the study (IRB number is R04-092).
Craniotomy
The patient was placed in a supine position on the operating table. The head was rotated 30° to the opposite side and secured using a Mayfield skull clamp (Ohwa Tsusho Co., LTD, Tokyo, Japan). A curvilinear skin incision was made in front of the tragus and continued to the midpoint of the hairline to preserve the superficial temporal arteries.
After the skin incision, the scalp was reflected subgaleally and the temporalis fascia, temporalis muscle, and periosteum were incised along the skin incision. They were then gently dissected with irrigation and reflected anteriorly. The temporalis muscle was dissected in a retrograde fashion to prevent muscle atrophy.[
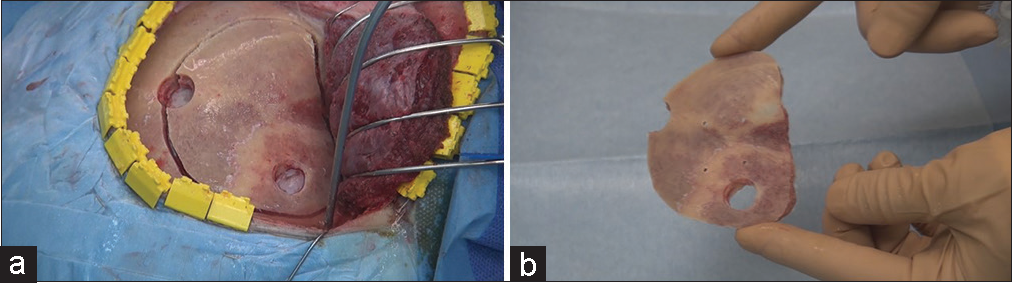
Cranioplasty
After completion of the intradural procedures, the dura was closed in a watertight fashion, using 4–0 polydioxanone suture (PDS, Johnson and Johnson K.K., Tokyo, Japan). In the case of a dural defect, the defect was patched with an autologous periosteal flap or a fascial flap. After dural closure, dural tenting sutures were placed through the tenting holes in the bone flap. A CranioFix Absorbable fixation system (AESCULAP Inc., Hessen, Germany) was employed.[
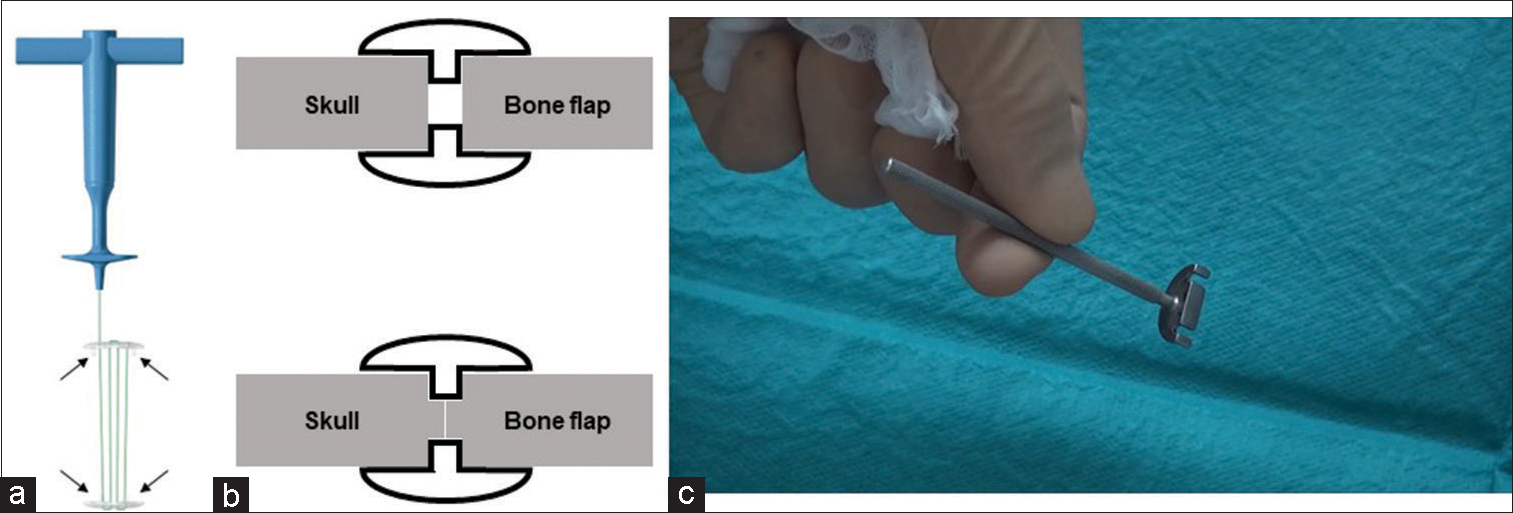
Figure 2:
CranioFix Absorbable and Guide (a) illustration of the CranioFix Absorbable system. Arrows indicate the gap pins. (b) Schematic drawing of the gap pins. The upper scheme indicates the creation of a gap between the skull and the bone flap using the usual method. The lower scheme indicates firm contact between the skull and bone flap achieved by making pivot holes to allow the gap pins to escape. (c) Photograph of the guide to mark the position for gap pins.
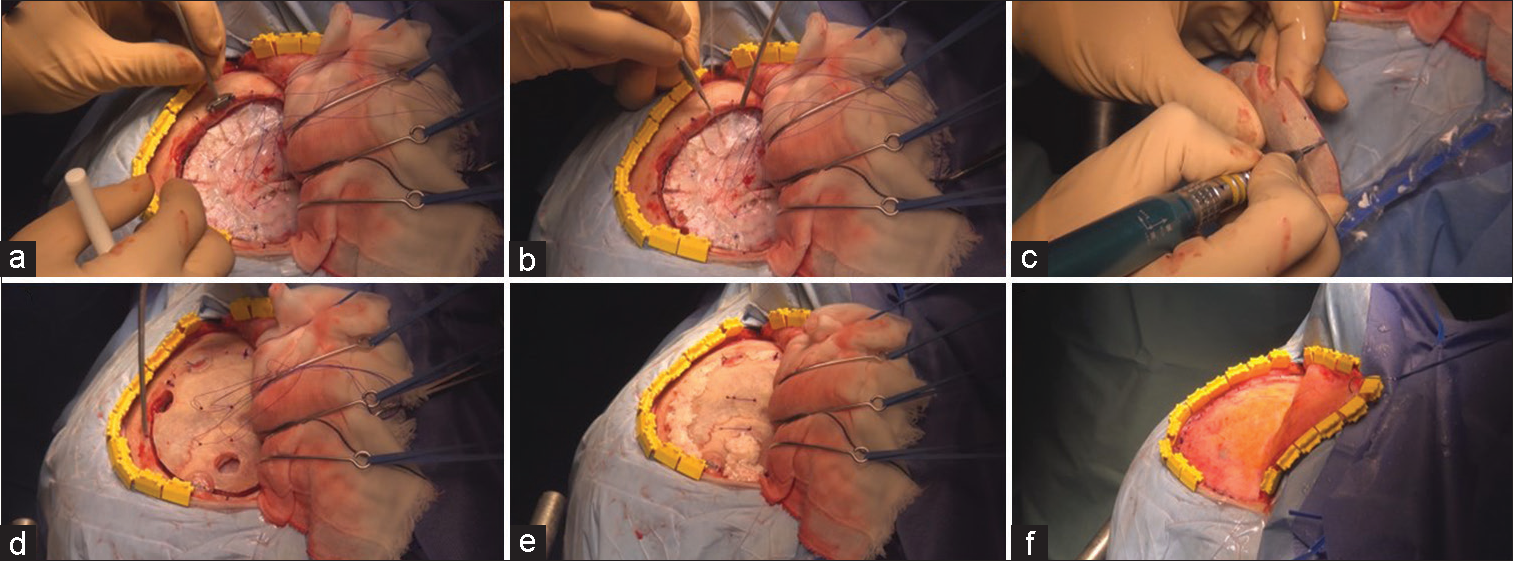
Figure 3:
Procedures of cranioplasty (a) Guide to marking the position for gap pins. (b) Pivot hole drilling according to the markings. (c) Pivot hole drilling on the bone flap to match skull markings. (d) Fixation with two CranioFix Absorbable clamps. (e) Pegging gaps with bone chips, and filling the gap and burr holes with bone dust and fibrin glue. (f) Closure of the temporalis fascia and periosteum.
Evaluation of computed tomography (CT) scan-based ossification
The extent of ossification of the bone gap was assessed using CT at 3, 6, and 12 months after surgery. CT scans of 0.5-mm slices were performed using a multirow high-resolution CT scan system (Toshiba Aquilion Prime, Tochigi, Japan; GE Discovery 750HD, Boston, MA, USA). Bone density CT scans were performed at a window level of 500 and a window width of 2000. CT values of bone gap ossification in Hounsfield Unit (HU) were calculated using the SYNAPSE Enterprise-PACS (Fujifilm Medical Corporation, Tokyo, Japan). The extent of ossification was determined by comparing the HU in the bone gap with that in the intact region.
Evaluation of CT scan-based temporal profile
The thickness of the temporalis muscle and overlying soft tissue was measured in the frontozygomatic fossa at the level of the orbital roof using a CT scan and was compared before and 1 year after surgery. The sum of the thickness of the temporalis muscle and overlying soft tissue was taken as the thickness of the temporal profile.
Statistical analysis
All statistical analyses were performed using Easy R (EZR)[
RESULTS
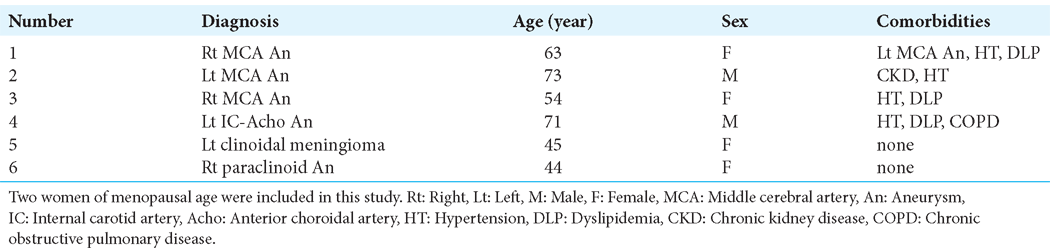
Six patients, ranging in age from 44 to 73 years, underwent head closure using the method described in this study. The male-to-female ratio was 2:4 [
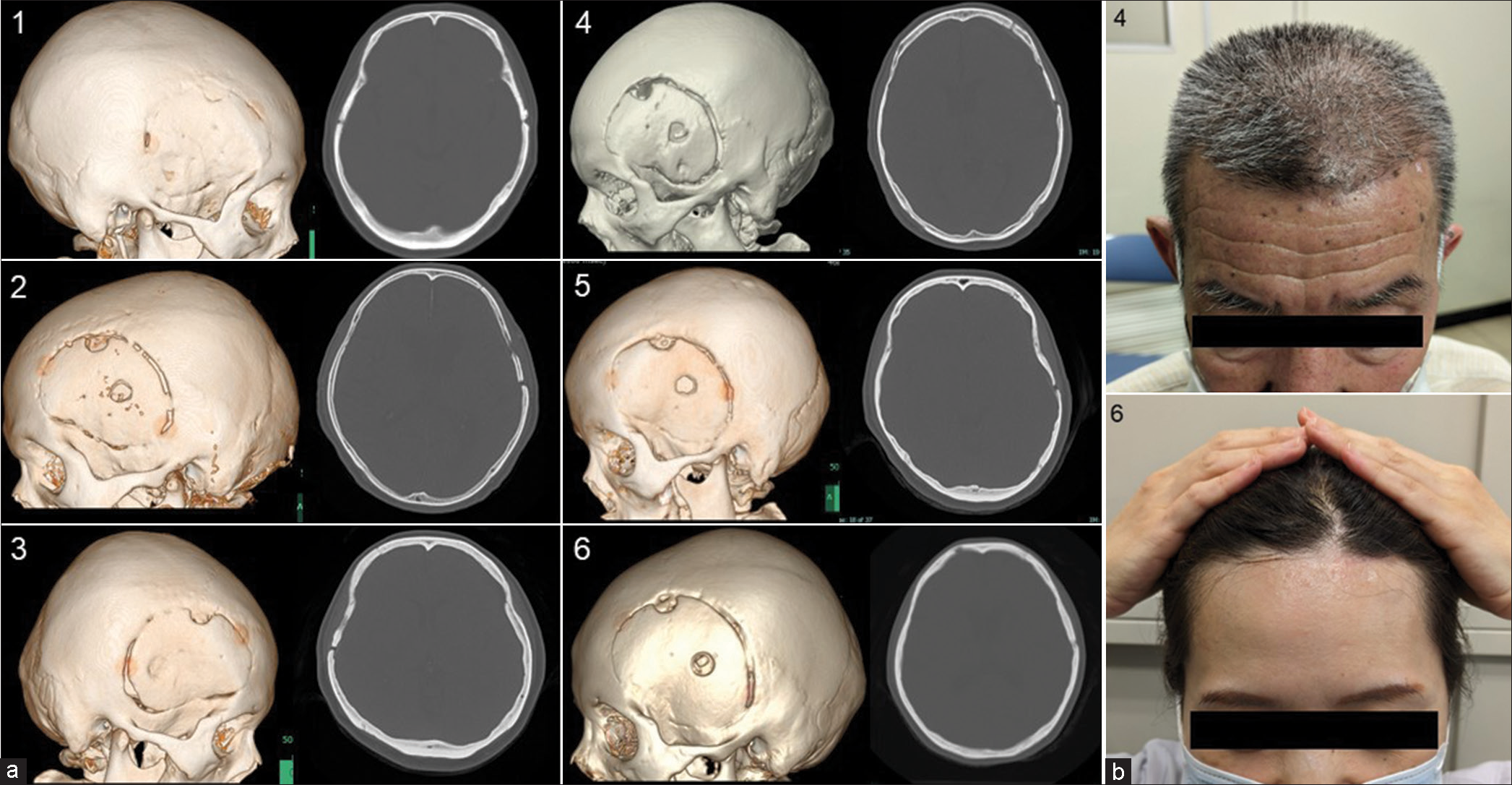
In all cases, satisfactory bone fixation was achieved with the CranioFix Absorbable system. None of the patients required reoperation due to postoperative infection or poor fixation. Moreover, bone fusion was detected in the frontal region where the skull was in contact with the bone flap. In the temporal region, where a bony gap occurs, bone fusion occurs over time, although only partially. Bone fusion was achieved in all cases 1 year after surgery, resulting in overall fusion and fixation of the bone flap and skull [
Figure 4:
Postoperative images. (a) Postoperative computed tomography images were obtained 1 year after the operation. The numbers correspond to those in Table 1. Bone fusion was detected in the frontal region, where the skull was in contact with the bone flap in every case. No marked flap depressions were observed. (b) Postoperative photographs of representative cases. The numbers correspond to those in Table 1. Case 4 photograph was taken 4 years after the operation, and Case 6 photograph was taken 3 years after the operation. No deformity was observed in appearance over several years, and symmetry was maintained on both sides.
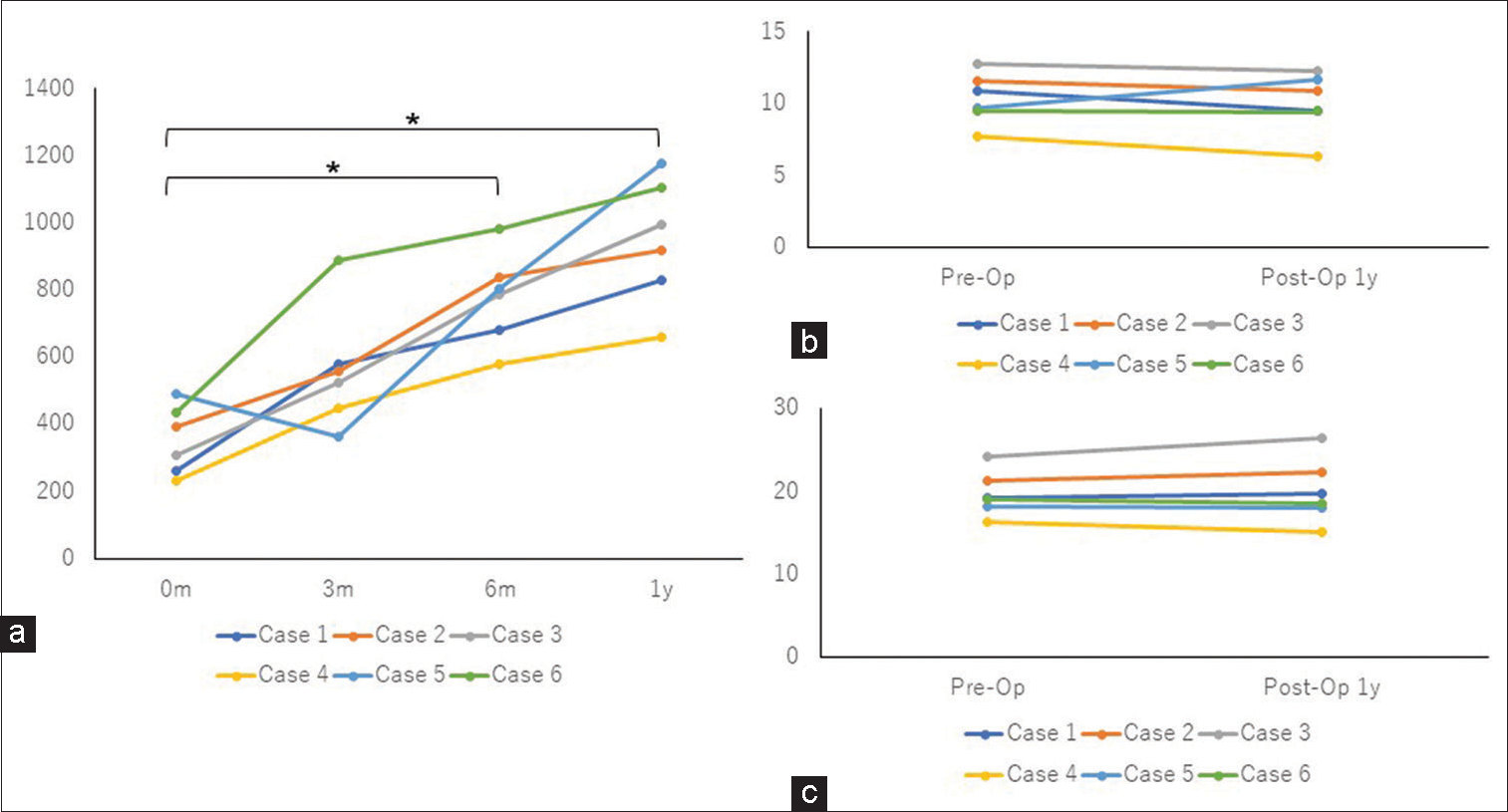
Figure 5:
Change of the computed tomography (CT) values of the bone gap and comparison of the thickness of the temporal profiles. (a) CT values of the bone gap were assessed by CT scan at 3, 6, and 12 months after the operation. The CT values of the bone gap gradually increased over time. (b) Comparison of the thickness of the temporalis muscle at the level of the orbital roof preoperatively and 1 year postoperatively. The difference was <2 mm in all cases. (c) Comparison of the thickness of the temporal profile at the level of the orbital roof preoperatively and 1 year postoperatively. There was little difference between the pre-and post-operative values in any of the cases. 0 months: Immediately after the operation; 3 m: 3 months after the operation; 6 m: 6 months after the operation; 1 y: 1 year after the operation. *P < 0.05; Pre-Op: Preoperatively; Post-Op 1 y: 1 year postoperatively.
DISCUSSION
A frontotemporal craniotomy is one of the most basic and important techniques used in neurosurgery and is used for treating various lesions, such as anterior circulation aneurysms and parasellar tumors. In the era when the Gigli saw was commonly used, a so-called keyhole, or key burr hole, was required.[
With the advent of titanium plates, postoperative cranioplasty became easier and bone defects could more easily be covered. However, titanium plates can sometimes cause postoperative skin problems, and because they are foreign bodies, they can also cause infection.[
Absorbable bone fixation devices are generally used in younger patients because they do not interfere with bone growth.[
The postoperative deformity is not only caused by the sinking of the bone but also by atrophy of soft tissues, such as the temporalis muscle. In our method, the postoperative temporal profile was not markedly atrophic but was maintained at the preoperative level [
Limitations
Our current study includes several limitations. First, the number of cases was small. Second, the long-term outcome of this procedure was unclear. Finally, histological confirmation of bone fusion was not proven. However, the CT values of the bone gap that appeared to be regenerated on CT were equivalent to bone, and continuity with the skull was observed. Therefore, we believe that the bone was regenerated and firmly fixed and that the long-term esthetic outcome will be satisfactory.
CONCLUSION
Our simple craniotomy, gentle tissue handling, and osteoplastic cranioplasty yielded satisfactory esthetic results. This method allows cost-effective cranioplasty and provides esthetically satisfactory fixation without the requirement of nonabsorbable materials, even in older patients.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Altay T, Couldwell WT. The frontotemporal (pterional) approach: An historical perspective. Neurosurgery. 2012. 71: 481-91 discussion 491-2
2. Asencio-Cortés C, Salgado-López L, Muñoz-Hernandez F, de Quintana-Schmidt C, Rodríguez-Rodríguez R, Álvarez-Holzapfel MJ. Long-term safety and performance of a polymeric clamplike cranial fixation system. World Neurosurg. 2019. 126: e758-64
3. Balasubramanian C, Chakravarthy H, John R. Keyhole and key-bur-hole. Neurosurgery. 2011. 68: E594
4. Böstman OM. Absorbable implants for the fixation of fractures. J Bone Joint Surg Am. 1991. 73: 148-53
5. Campbell CA, Lin KY. Complications of rigid internal fixation. Craniomaxillofac Trauma Reconstr. 2009. 2: 41-7
6. Hernesniemi J, Ishii K, Niemelä M, Smrcka M, Kivipelto L, Fujiki M. Lateral supraorbital approach as an alternative to the classical pterional approach. Acta Neurochir Suppl. 2005. 94: 17-21
7. Horimoto C, Toba T, Yamaga S, Tsujimura M. Subfascial temporalis dissection preserving the facial nerve in pterional craniotomy--technical note. Neurol Med Chir (Tokyo). 1992. 32: 36-7
8. Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013. 48: 452-8
9. Kang SD. Pterional craniotomy without keyhole to supratentorial cerebral aneurysms: Technical note. Surg Neurol. 2003. 60: 457-61 discussion 461-2
10. Krayenbühl HA, Yaşargil MG, Flamm ES, Tew JM. Microsurgical treatment of intracranial saccular aneurysms. J Neurosurg. 1972. 37: 678-86
11. Lemcke J, Meier U, Al-Zain F. The clinical application of a new absorbable fixation clamp in craniotomy closure. A technical note after first experiences with 29 patients. Acta Neurochir (Wien). 2009. 151: 1231-4
12. Lopez J, Siegel N, Reategui A, Faateh M, Manson PN, Redett RJ. Absorbable fixation devices for pediatric craniomaxillofacial trauma: A systematic review of the literature. Plast Reconstr Surg. 2019. 144: 685-92
13. Matsumoto K, Akagi K, Abekura M, Ohkawa M, Tasaki O, Tomishima T. Cosmetic and functional reconstruction achieved using a split myofascial bone flap for pterional craniotomy. Technical note. J Neurosurg. 2001. 94: 667-70
14. Moscovici S, Mizrahi CJ, Margolin E, Spektor S. Modified pterional craniotomy without “MacCarty keyhole”. J Clin Neurosci. 2016. 24: 135-7
15. Oikawa S, Mizuno M, Muraoka S, Kobayashi S. Retrograde dissection of the temporalis muscle preventing muscle atrophy for pterional craniotomy. Technical note. J Neurosurg. 1996. 84: 297-9
16. Resnick JI, Kinney BM, Kawamoto HK. The effect of rigid internal fixation on cranial growth. Ann Plast Surg. 1990. 25: 372-4
17. Rychen J, Croci D, Roethlisberger M, Nossek E, Potts M, Radovanovic I. Minimally invasive alternative approaches to pterional craniotomy: A systematic review of the literature. World Neurosurg. 2018. 113: 163-79
18. Sadatomo T, Yuki K, Migita K, Taniguchi E, Kodama Y, Kurisu K. Reconstruction of pterional key hole using three-dimensional titanium plate: Technical note. Hiroshima J Med Sci. 2005. 54: 53-6
19. Sakata Y, Hadeishi H, Moroi J. Cosmetic frontotemporal craniotomy using an osteotome: Technical note. Neurol Med Chir (Tokyo). 2013. 53: 635-7
20. Yaşargil MG, Fox JL. The microsurgical approach to intracranial aneurysms. Surg Neurol. 1975. 3: 7-14
21. Yaşargil MG, Reichman MV, Kubik S. Preservation of the frontotemporal branch of the facial nerve using the interfascial temporalis flap for pterional craniotomy. Technical article. J Neurosurg. 1987. 67: 463-6