- Department of Neurosurgery, Fukui Prefectural Hospital, Fukui, Japan.
DOI:10.25259/SNI_582_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yu Shimizu, Katsuyoshi Miyashita, Nozomu Oikawa, Masaaki Kobayashi, Yasuo Tohma. Ring enhanced aneurysm due to vasa vasorum of aneurysm wall mimicking a metastatic brain tumor. 17-Feb-2021;12:64
How to cite this URL: Yu Shimizu, Katsuyoshi Miyashita, Nozomu Oikawa, Masaaki Kobayashi, Yasuo Tohma. Ring enhanced aneurysm due to vasa vasorum of aneurysm wall mimicking a metastatic brain tumor. 17-Feb-2021;12:64. Available from: https://surgicalneurologyint.com/surgicalint-articles/10589/
Abstract
Background: A spherical intracranial mass can be occasionally misdiagnosed due to the lack of typical radiographic features. Completely thrombosed intracranial aneurysms (CTIA) are uncommon, but a possible differential diagnosis must be considered to guarantee the best surgical approach for these lesions.
Case Description: Here, we report an extremely rare case of a right frontal mass mimicking a brain tumor, in which the surgery unveiled a CTIA of the right middle cerebral artery (MCA). A 56-year-old woman presented with right hemiparesis and mild headache. Magnetic resonance imaging (MRI) revealed a right frontal mass with peripheral edema. The lesion enhanced on initial and follow-up MRI of the brain. Subsequent vascular studies and metastatic workup were negative. A temporal craniotomy with neuronavigation (Brain Lab AG, Germany) was performed and an intraoperative diagnosis of a thrombosed aneurysm along the branch of the MCA was established. The aneurysm was successfully trapped and resected. The patient did not exhibit any postoperative neurological deficits.
Conclusion: This is the rare report of a ring enhanced completely thrombosed aneurysm due to vasa vasorum which is misdiagnosed as metastatic brain tumor. In case of an intracranial ring enhanced mass with signs of intralesional hemorrhage and peripheral edema, CTIA should be considered as a possible differential diagnosis.
Keywords: Metastatic brain tumor, Ring enhance, Thrombosis, Vasa vasorum
INTRODUCTION
A thrombosed aneurysm is an aneurysm that exhibits an intraluminal thrombus, which is diagnosed based on preoperative imaging and intraoperative findings. Thrombosed aneurysms have been classified into the following six types: concentric, eccentric, lobulated, canalized, coiled, and complete.[
There have been rare case reports of completely thrombosed aneurysms imitating tumor based on the initial presentation and imaging.[
Although up to 40% of cerebral aneurysms involve the middle cerebral artery (MCA), few cases have been reported along the MCA.[
CASE PRESENTATION
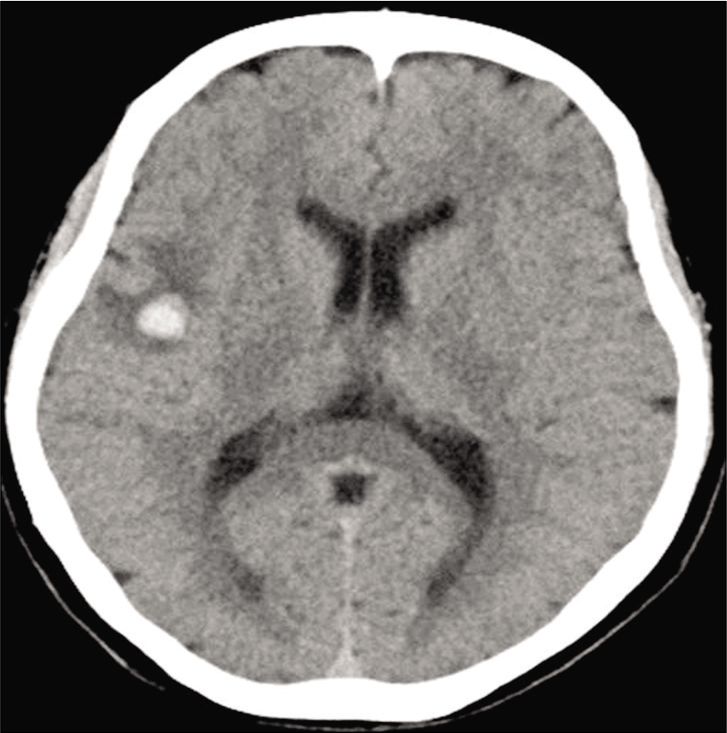
A 56-year-old woman presented to the emergency department with headache and right hemiparesis. Blood screening did not indicate any signs of infection, but she had the history of ovarian tumor resection. A computed tomography (CT) scan revealed a hyperdense mass in the right frontal lobe [
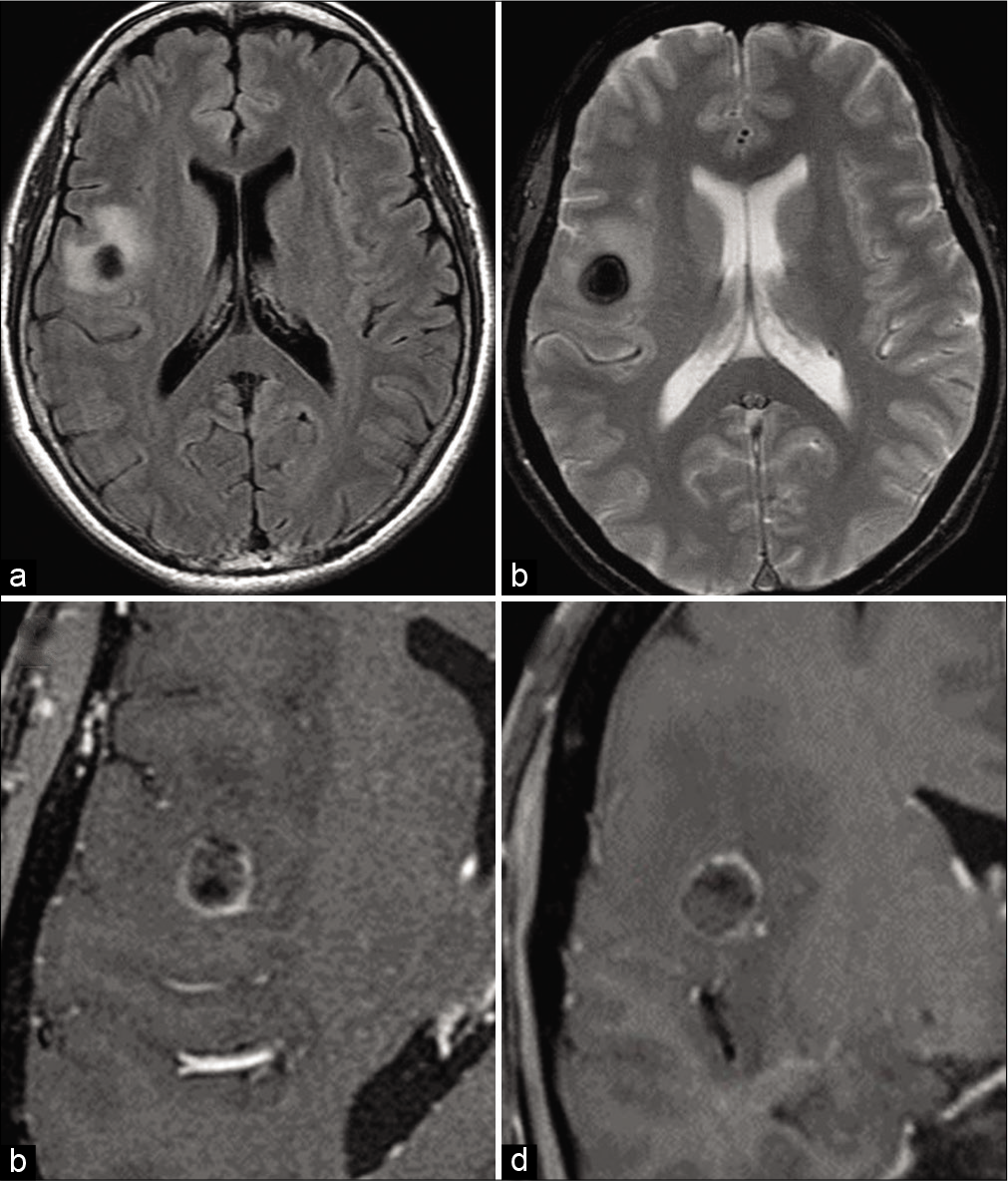
Figure 2:
(a) Fluid-attenuated inversion recovery axial magnetic resonance imaging (MRI). (b) T2-weighted axial MRI. (c) Gadolinium-enhanced T1-weighted axial MRI. (d) Gadolinium-enhanced T1-weighted coronal MRI. A round mass with surrounding edema is noted in the right frontal lobe. T2-weighted image shows dark signal intensity due to hematoma. Gadolinium-enhanced T1-weighted images show ring enhancement, suggesting intra-axial neoplasm as a differential diagnosis.
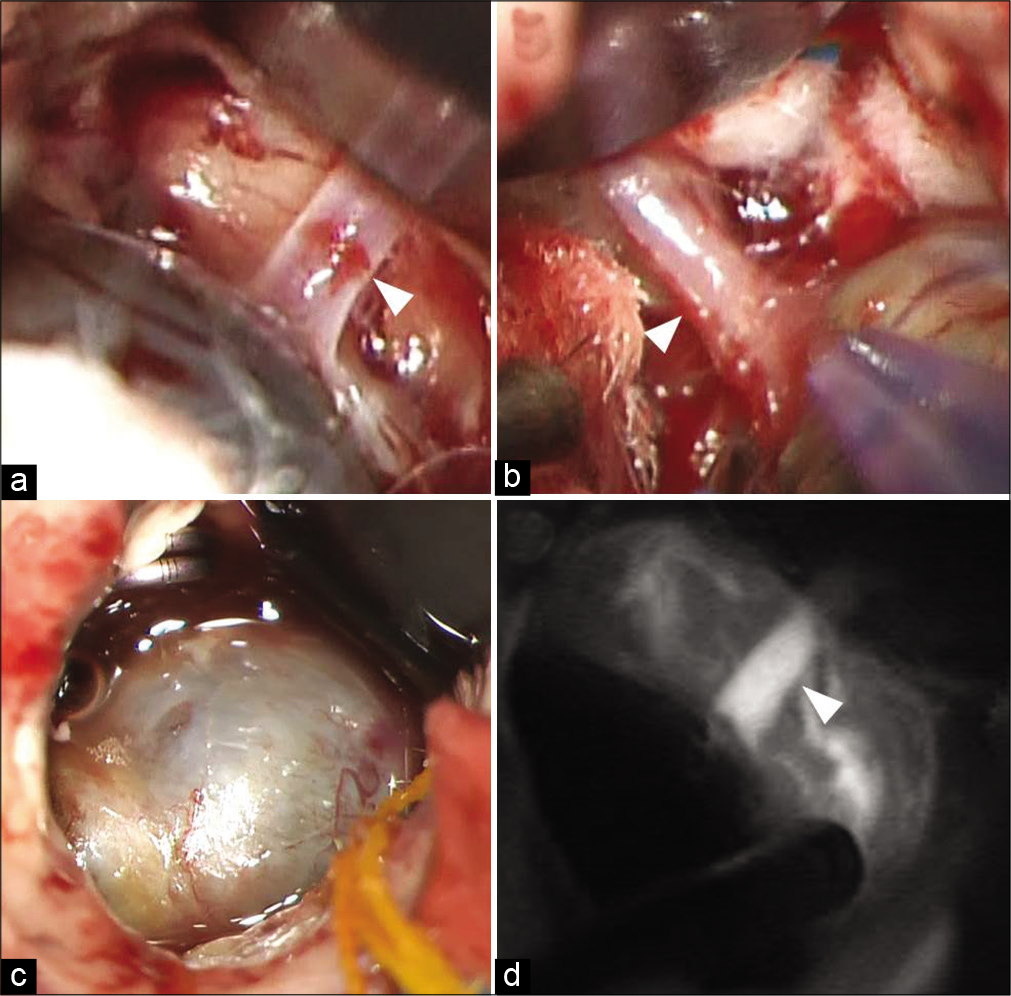
Figure 3:
(a) Small artery (white arrow) connected to the distal end of the mass revealed under the mass. It seems to be a branch of the middle cerebral artery. Vascular clip is applied at the parent artery and the distal end is resected. (b) Small artery (white arrow) connected to the proximal end of the mass. Vascular clip is applied and the artery is resected. (c) The grayish black mass is completely excised and there was no other complication at the surgical site. (d) The intraoperative indocyanine green angiography demonstrated absence of blood flow in the aneurysm.
Postoperatively, the patient was stable and had no neurological deficits. A collateral circulation from the MCA and posterior circulation was detected. After 1-month of follow-up, the patient recovered from the surgery and could walk without assistance.
DISCUSSION
Spontaneous thrombosis of MCA aneurysm is known to occur in approximately 16% of giant aneurysms and only 2–3% are completely thrombosed aneurysms.[
The mechanism of the spontaneous thrombosis of an aneurysm and its parent artery is unknown. Theories of local stretching, compression, and distortion could explain the occurrence of this complication in intracranial aneurysms, due to the presence of dural folds and bony structures at this location.[
The CT and MRI findings in thrombotic aneurysm include peripheral ring enhancement, curvilinear mural calcification, mixed high-density attenuation in the aneurysmal lumen, the presence of “target sign,” and perianeurysmal edema on the FLAIR images.[
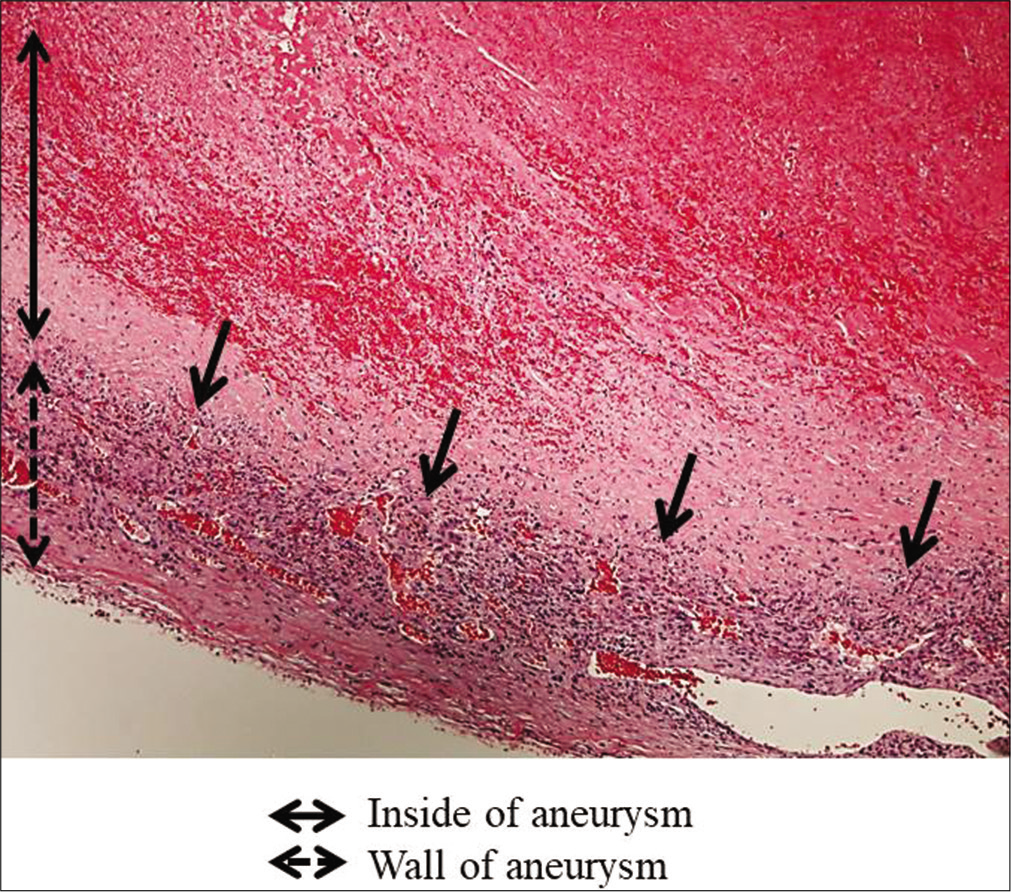
Recently, the pathogenesis of thrombosed aneurysm was proposed to originate in structural vessel wall disease. The vessel wall was injured by hypercholesterolemia, atherosclerosis, and chronic inflammation.[
The endothelial cell junctions are responsible for maintaining vessel wall integrity and preventing the leakage of intravascular components to the extravascular space. As angiogenic processes are initiated vessel permeability increases, enabling the deposition of serum proteins, triggering inflammatory cell adhesion of neutrophils, and lymphocytes. Both local and systemic inflammation results in increased permeability of the endothelial cell junctions.[
Our patient showed ring enhancement and perianeurysmal edema on MRI; hence, she was misdiagnosed with neoplasm. The histopathological findings revealed the vasa vasorum on the aneurysm wall and many lymphocytes and neutrophils infiltrated in the vessel wall. The vasa vasorum could be involved in ring enhancement.
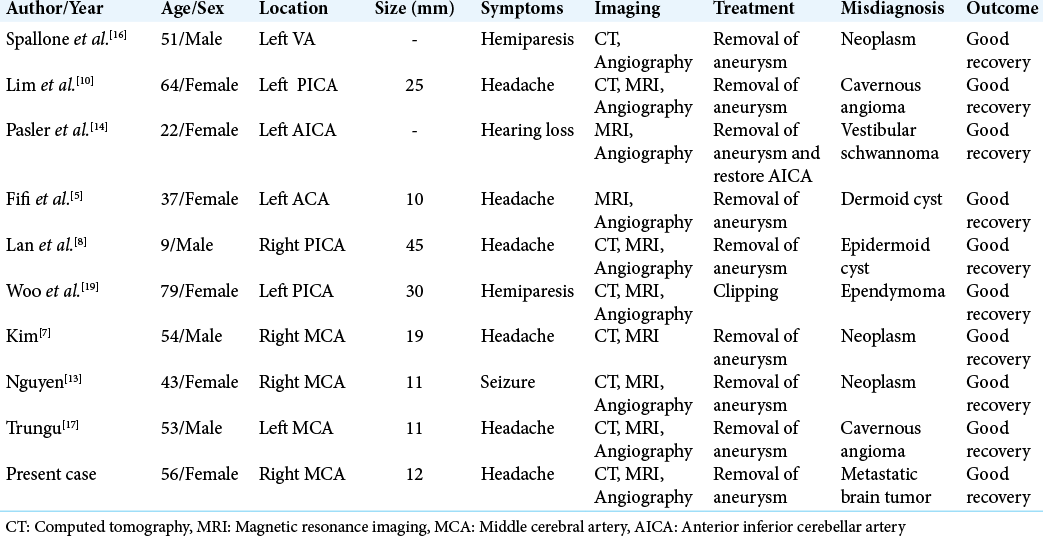
Misdiagnosis of a thrombosed aneurysm as a brain tumor is not rare in clinical field; however, completely thrombosed aneurysms mimicking intracranial neoplasms have been reported only in nine cases previously [
When a patient presents with an intracranial lesion lying on the course of major cerebral arteries or even on the course of distal cerebral arteries, it is important to consider thrombosed aneurysm as one of the differential diagnosis.
In the literature, nine of ten cases underwent aneurysm trapping and removal of the aneurysm.[
CONCLUSION
CTIA is a rare lesion that could be misdiagnosed as metastatic brain tumor. Thus, in case of an intracranial ring enhanced mass with intralesional hemorrhage, presence of a CTIA should be considered as a possible differential diagnosis. This is the rare report of a ring enhanced completely thrombosed aneurysm due to vasa vasorum of wall which is misdiagnosed as metastatic brain tumor.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Black SP, German WJ. Observations on the relationship between the volume and the size of the orifice of experimental aneurysms. J Neurosurg. 1960. 17: 984-90
2. Das KK, Singh G, Pandey S, Bhaisora KS, Jaiswal A, Behari S. Completely thrombosed giant intracranial aneurysm with spontaneous thrombosis of the parent artery: Is it nature’s divine intervention and a self-cure?. World Neurosurg. 2018. 118: 132-8
3. Dashti R, Rinne J, Hernesniemi J, Niemelä M, Kivipelto L, Lehecka M. Microneurosurgical management of proximal middle cerebral artery aneurysms. Surg Neurol. 2007. 67: 6-14
4. dos Santos ML, Spotti AR, dos Santos RM, Borges MA, Ferrari AF, Colli BO. Giant intracranial aneurysms: Morphology and clinical presentation. Neurosurg Rev. 2013. 36: 117-22
5. Fifi JT, Komotar R, Meyers P, Khandji A, Tanji K, Connolly ES. Restricted diffusion in a thrombosed anterior cerebral artery aneurysm mimicking a dermoid cyst. J Neuroimaging. 2012. 22: 85-8
6. Hashimoto T, Meng H, Young WL. Intracranial aneurysms: Links among inflammation, hemodynamics and vascular remodeling. Neurol Res. 2006. 28: 372-80
7. Kim YJ, Jeun SS, Park JH. Thrombosed large middle cerebral artery aneurysm mimicking an intra-axial brain tumor: Case report and review of literature. Brain Tumor Res Treat. 2015. 3: 39-43
8. Lan ZG, Ma L, Duan J, You C. A fully thrombosed giant posterior inferior cerebellar aneurysm mimicking an intracranial tumour in a child. Br J Neurosurg. 2012. 26: 888-90
9. Lawton MT, Quiñones-Hinojosa A, Chang EF, Yu T. Thrombotic intracranial aneurysms: Classification scheme and management strategies in 68 patients. Neurosurgery. 2005. 56: 441-54
10. Lim DH, Jung S, Jung TY, Kim TS. An unusual case of a thrombosed giant distal PICA aneurysm simulating a large cavernous angioma. J Korean Neurosurg Soc. 2008. 43: 155-8
11. Martin AJ, Hetts SW, Dillon WP, Higashida RT, Halbach V, Dowd CF. MR imaging of partially thrombosed cerebral aneurysms: Characteristics and evolution. AJNR Am J Neuroradiol. 2011. 32: 346-51
12. Nakatomi H, Segawa H, Kurata A, Shiokawa Y, Nagata K, Kamiyama H. Clinicopathological study of intracranial fusiform and dolichoectatic aneurysms: Insight on the mechanism of growth. Stroke. 2000. 31: 896-900
13. Nguyen HS, Doan N, Eckardt G, Gelsomino M, Shabani S, Brown WD. A completely thrombosed, nongiant middle cerebral artery aneurysm mimicking an intra-axial neoplasm. Surg Neurol Int. 2015. 6: 146
14. Pasler D, Baldauf J, Runge U, Schroeder HW. Intrameatal thrombosed anterior inferior cerebellar artery aneurysm mimicking a vestibular schwannoma. J Neurosurg. 2011. 114: 1057-60
15. Perrini P, Bortolotti C, Wang H, Fraser K, Lanzino G. Thrombosed giant intracavernous aneurysm with subsequent spontaneous ipsilateral carotid artery occlusion. Acta Neurochir (Wien). 2005. 147: 215-7
16. Spallone A. Giant, completely thrombosed intracranial aneurysm simulating tumor of the foramen magnum. Surg Neurol. 1982. 18: 372-6
17. Trungu S, Bruzzaniti P, Forcato S, Cimatti M, Raco A. Completely thrombosed distal middle cerebral artery aneurysm mimicking a cavernous angioma: Case report and review of the literature. World Neurosurg. 2017. 103: 955.e1-4
18. Whittle IR, Williams DB, Halmagyi GM, Besser M. Spontaneous thrombosis of a giant intracranial aneurysm and ipsilateral internal carotid artery. Case report. J Neurosurg. 1982. 56: 287-9
19. Woo PY, Ko NM, Chan KY. Thrombosed large distal posterior inferior cerebellar artery aneurysm mimicking an infratentorial ependymoma. Case Rep Neurol Med. 2014. 2014: 435953