- Department of Neurosurgery, UPMC, Pittsburgh, PA,
- School of Medicine, Drexel University, Philadelphia, PA, United States,
- Department of Biology, John Hopkins University, Gibsonia, PA, United States,
- Department of Medical School, University of Balamand, Al Kurah,
- School of Medicine, American University Beirut, Beirut, Lebanon.
Correspondence Address:
Matt El-Kadi
School of Medicine, American University Beirut, Beirut, Lebanon.
DOI:10.25259/SNI-284-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Matt El-Kadi, Erin Donovan, Laurel Kerr, Coby Cunningham, Victor Osio, Samah Abdallah, Joseph Kazan. Risk factors for postoperative spinal infection: A retrospective analysis of 5065 cases. 25-Jun-2019;10:121
How to cite this URL: Matt El-Kadi, Erin Donovan, Laurel Kerr, Coby Cunningham, Victor Osio, Samah Abdallah, Joseph Kazan. Risk factors for postoperative spinal infection: A retrospective analysis of 5065 cases. 25-Jun-2019;10:121. Available from: http://surgicalneurologyint.com/surgicalint-articles/9410/
Abstract
Background: Multiple factors increase the risk for spinal surgical site infection (SSI): prior SSI, obesity, diabetes mellitus, advanced age, American Society of Anesthesiologists class, alcohol abuse, low prealbumin levels, smoking, history of cancer, chronic steroids, immunosuppressive drugs, rheumatoid arthritis, and hypothyroidism.
Methods: Here, we performed a retrospective medical record review at one facility involving 5065 patients from 2010 to 2015. In 2011, there was an increase in the infection rate (1.07%) which prompted this analysis, resulting in the subsequent introduction of a protocol to reduce the infection risk.
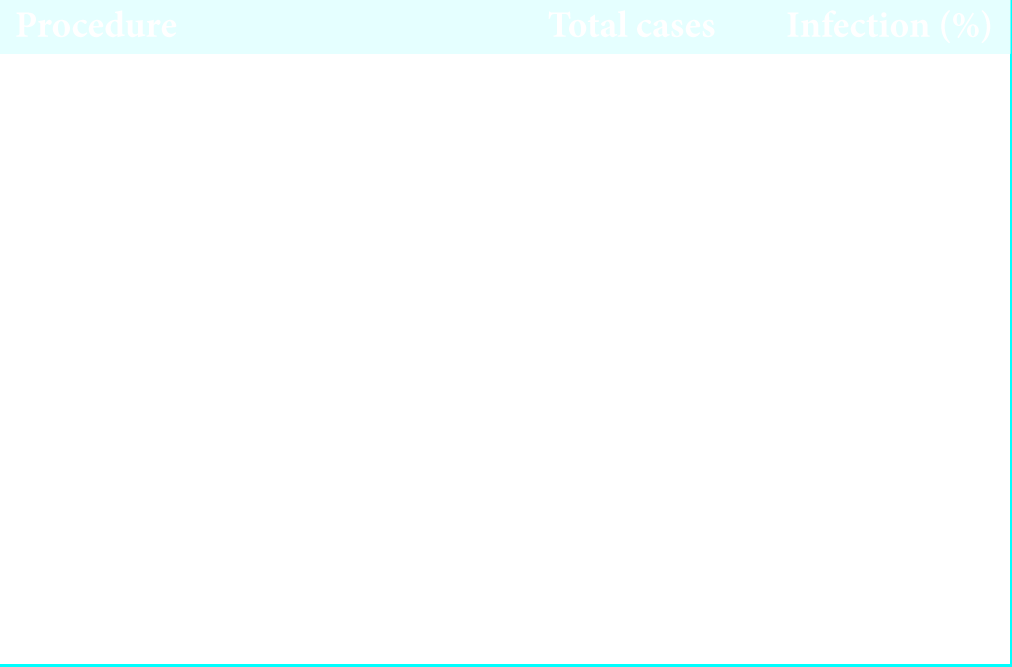
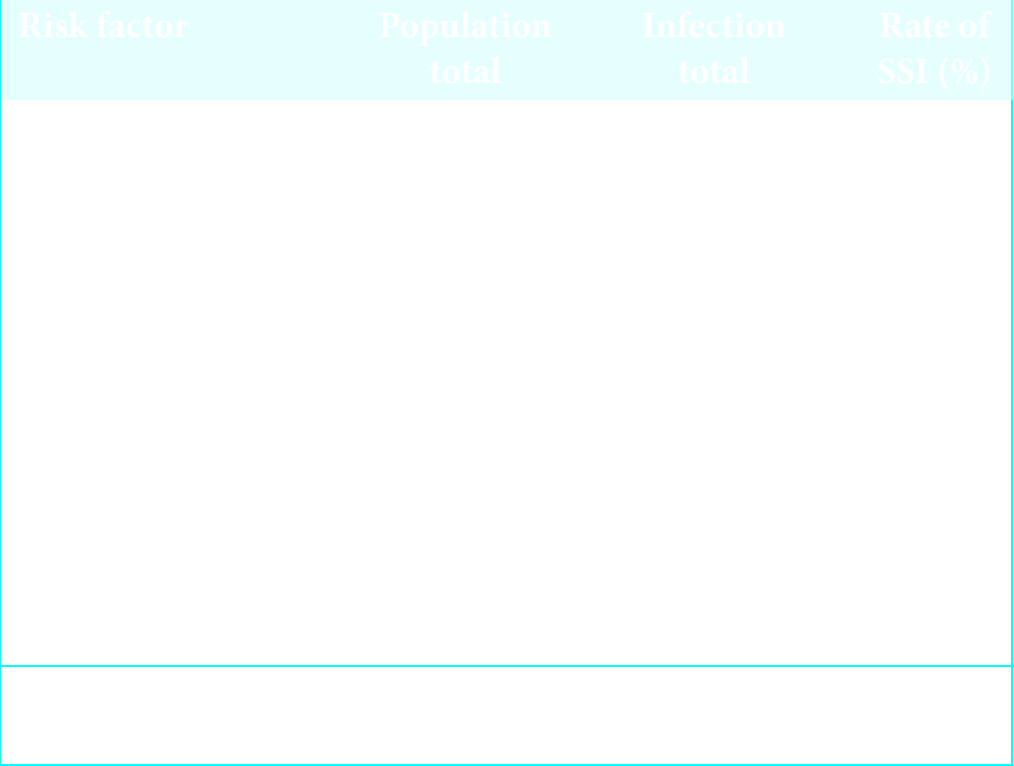
Results: The overall infection rate in this series was 0.59%. The lowest infection rate was 0.00% for anterior cervical discectomy and fusion. The highest rate of infections occurred among patients undergoing posterior cervical fusions, lumbar fusions, and tumor resections. Higher infection rates were also correlated with diabetes mellitus, obesity, and increased surgical time.
Conclusions: Since 2011, we instituted a protocol to limit the risks of spinal SSIs, particularly for patients exhibiting increased medical comorbidities.
Keywords: Infection, Risk factors, Spine surgery, Surgical site infection
INTRODUCTION
Postoperative infection in spine surgery occurs from <1% to as high as 12% of the time.[
In 2011, we noted an increase in SSI at our institution. These SSI correlated with the following predisposing risk factors/comorbidities: obesity, diabetes mellitus, advanced age, higher American Society of Anesthesiologists (ASA) class, alcohol abuse, low prealbumin levels and malnutrition status, smoking, history of cancer, chronic steroid use, rheumatoid arthritis, and hypothyroidism. Here, we reviewed our findings and the protocol we introduced to avoid SSI in 2011 along with a review of literature.
METHODS
We performed a retrospective medical record review of SSI from 2010 to 2015 with the institutional review board approval. The multiple risk factors and comorbidities studied included diabetes, obesity, smoking, age, and ASA. In 2012, we implemented new additional preoperative and perioperative measures to reduce SSI infection risk.
Preoperative counseling and measures
Preoperatively, as appropriate, patients were advised regarding; weight loss, smoking cessation, and discontinuation of immunosuppressant medications. Those with inadequate prealbumin levels received high protein supplements.[
Skin prep protocol
Three days before surgery, patients were advised to perform local washing of the operative site with Hibiclens. For high- risk patients, a three-step regimen was initiated that included; first isopropyl alcohol, next Betadine, and finally Hibiclens. In the preoperative holding area, the patients’ surgical site was wiped with chlorhexidine gluconate.
Preoperative antibiotic protocol
Cefazolin was used as a first-line antibiotic; we utilized a standard dose of 2 g. However, patients over 80 kg received 3 g. The second-line antibiotic was vancomycin dosed at 1 g; patients over 90 kg received 1.5 g. The antibiotic chosen was redosed when the length of the operative procedure exceeded 4 h. Intravenous antibiotics were continued for 24–48 h postoperatively, dependent on the drain status. In high-risk patients, 5 days of additional oral antibiotics were given at discharge.
Intraoperative irrigation
In high-risk patients, the surgical wound was irrigated with 3 l of saline with antibiotics before skin closure. In addition, in 2014, vancomycin powder was introduced and placed topically in the operative bed.
Silver dressing
In high-risk patients, silver nitrate impregnated dressings were utilized over wounds with staples or sutures. The operative dressing was maintained for 3 days in most cases, followed by daily dry dressing changes and a Betadine cleanse of staples when present. The wound was kept dry and covered for 1 week.
Foley catheter
The Foley catheter was discontinued on postoperative day 1, unless longer placement was indicated.
Glucose monitoring
In diabetic patients, glucose levels were monitored closely intraoperatively, and postoperatively; they were treated appropriately.
Immunosuppressant medications
These medications were routinely discontinued 2 weeks before surgery and resumed at the first 2 weeks postoperative visit.
RESULTS AND DISCUSSION
The population comprised a total of 5065 spine cases performed by one service in the same facility. A total of 30 (0.59%) infections were documented utilizing positive wound cultures taken during operative wound revisions. The peak rate was seen in 2011, with 11 (1.07%) SSIs out 1031 cases performed that year.
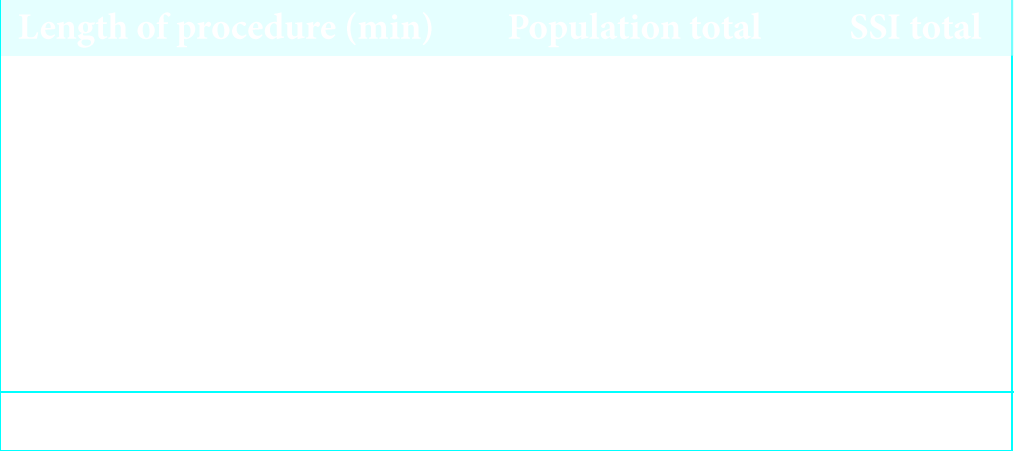
In general, longer procedures were associated with an increased risk of SSI.[
The 5065 cases were divided into eight categories [
We were not able to identify a correlation between the risk of infection and the ASA classification score.
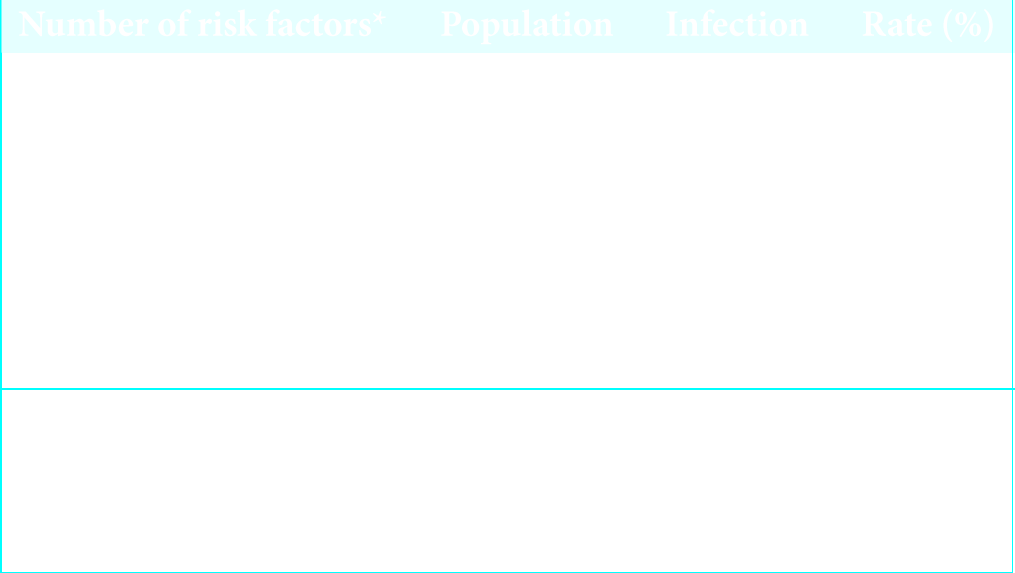
With the initiation of the current protocol, since 2011, over the next 6 years, despite a gradual increase in the medical complexity/comorbidities of the patient population, there were no further increases in the SSI rates [
Organisms involved in infection
In literature, Staphylococcus aureus is the principal agent cited in SSI following spine surgery.[
CONCLUSIONS
SSIs increase the costs of spinal surgery, resulting in readmissions and/or increased length of hospital stay. Obesity and diabetes independently contributed to higher SSI rates. Our data showed that multiple risk factors may quadruple the expected SSI rate. However, the introduction of a new infection prevention protocol in 2011 kept the infection rate as low as 0.59%, regardless of the case complexity, attendant comorbidities, and increased case mix index over the ensuing 6 years.
References
1. Beiner JM, Grauer J, Kwon B, Vaccaro AR. Postoperative wound infections of the spine. Neurosurg Focus. 2003. 15: 1-5
2. Blumberg T, Woelber E, Bellabarba C, Bransford R, Spina N. Predictors of increased cost and length of stay in the treatment of postoperative spine surgical site infection. Spine J. 2017. 18: 300-6
3. Chahoud J, Kanafani Z, Kanj SS. Surgical site infections following spine surgery: Elmininating the controversies in the diagnosis. Front Med. 2014. 1: 1-10
4. Epstein NE. Predominantly negative impact of diabetes on spinal surgery: A review and recommendation for better preoperative screening. Surg Neurol Int. 2017. 8: 107-
5. Guan J, Holland CM, Schmidt MH, Dailey AT, Mahan MA, Bisson EF. Association of low perioperative prealbumin level and surgical complications in long-segment spinal fusion patients: A retrospective cohort study. Int J Surg. 2017. 39: 135-40
6. Veeravagu A, Patil CG, Lad SP, Boakye M. Risk factors for postoperative spinal wound infections after spinal decompression and fusion surgeries. Spine. 2009. 34: 1869-72