- Department of Neurosurgery, Kasr Al Ainy Medical School, Cairo, Egypt.
Correspondence Address:
Ahmed Adel Ezzat, Department of Neurosurgery, Kasr Al Ainy Medical School, Cairo, Egypt.
DOI:10.25259/SNI_866_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahmed Adel Ezzat, Ahmed Mohamed Salah. Rod migration through foramen magnum into posterior fossa after cervical spine lateral mass fixation: A case report and literature review. 04-Nov-2022;13:514
How to cite this URL: Ahmed Adel Ezzat, Ahmed Mohamed Salah. Rod migration through foramen magnum into posterior fossa after cervical spine lateral mass fixation: A case report and literature review. 04-Nov-2022;13:514. Available from: https://surgicalneurologyint.com/surgicalint-articles/11971/
Abstract
Background: Posterior cervical fusion is one of the most common surgical procedures performed for the treatment of many cervical spine pathologies. Hardware failure, due to rod displacement either cranially or caudally, may occur.
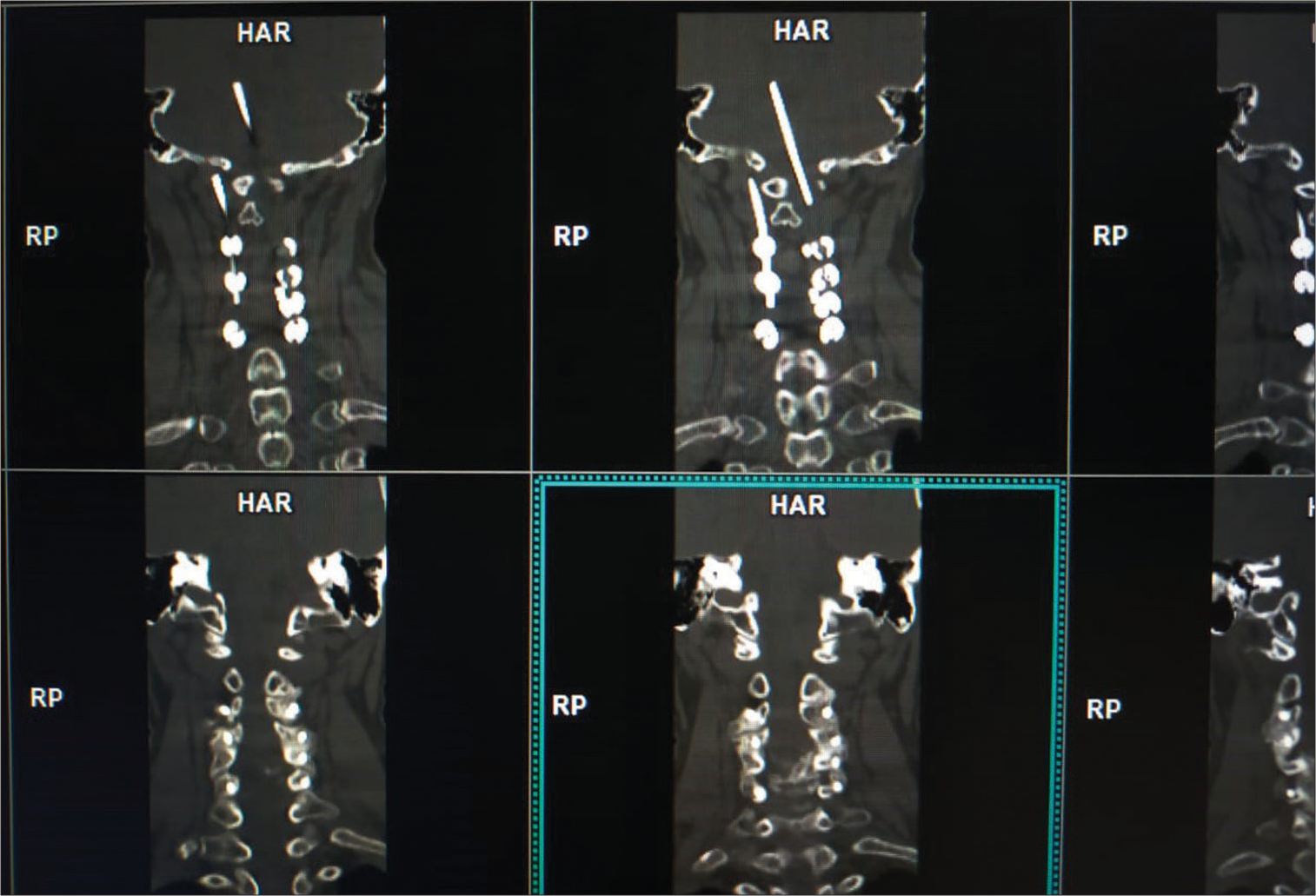
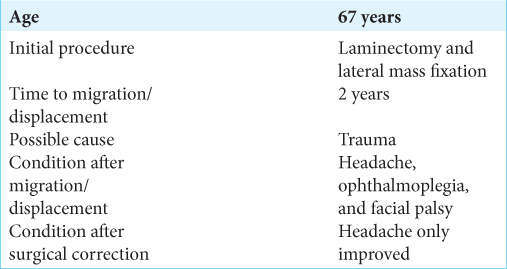
Case Description: Two years following a subaxial laminectomy/lateral mass fusion (from C3 to C6) for stenosis, a 67-year-old female, with a history of trauma 2 months ago, presented with headaches, right-sided facial palsy, and right complete ophthalmoplegia. When the computed tomography scan showed migration of the left-sided rod extending into the posterior fossa through the foramen magnum plus malpositioning of the right rod, she underwent bilateral rod removal resulting in marked headache improvement without improvement of ophthalmoplegia and facial palsy.
Conclusion: Cephalad rod migration/displacement extending through the foramen magnum into the posterior fossa is a rare complication of cervical laminectomy/rod lateral mass screw instrumented fusion.
Keywords: Cervical, Lateral mass, Migration, Posterior fossa, Rod
INTRODUCTION
The several methods for cervical decompression/fusion include the application of wires, lateral mass screws, pedicle screws, and transarticular screws.[
CASE REPORT
A 67-year-old female originally underwent a cervical laminectomy with lateral mass fixation (from C3 to C6) for cervical canal stenosis [
DISCUSSION
Risks of cephal malpositioning/displacement of posterior cervical rods
Lateral mass screw fixation with rods or plates has become one of the most popular methods for posterior cervical spine fixation.[
Literature on cephalad migration/displacement of lateral mass screw/rods
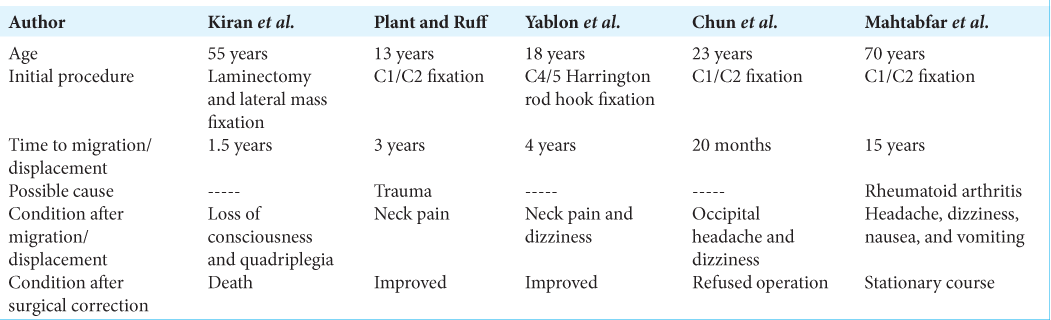
Other studies have similarly reported cephalad displacement of posterior cervical rods to/through the foramen magnum into the posterior fossa resulting in brainstem compression [
CONCLUSION
Rod migration or displacement is a rare complication of cervical lateral mass screw/rod fixation procedures. For patients developing symptoms/signs of brainstem compression, appropriate diagnostic studies (i.e., CT/MR and CTA of the brain/cervical spine) should be performed and lead to prompt surgical remediation (i.e., decompression/ instrumentation removal as needed).
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Chun HJ, Bak KH, Kang TH, Yi HJ. Rod migration into the posterior fossa after harms operation: Case report and review of literatures. J Korean Neurosurg Soc. 2010. 47: 221-3
2. Coe JD, Vaccaro AR, Dailey AT, Skolasky RL, Sasso RC, Ludwig SC. Lateral mass screw fixation in the cervical spine: A systematic literature review. J Bone Joint Surg Am. 2013. 95: 2136-43
3. Dogan S, Gundogdu EB, Taşkapılıoğlu MÖ Karaoglu A. Rod migration to the thoracic subarachnoid space after C1-2 instrumentation: A case report and literature review. Orthop Surg. 2017. 9: 129-32
4. Inoue S, Moriyama T, Tachibana T, Okada F, Maruo K, Horinouchi Y. Cervical lateral mass screw fixation without fluoroscopic control: Analysis of risk factors for complications associated with screw insertion. Arch Orthop Trauma Surg. 2012. 132: 947-53
5. Kiran B, Sharma A, Prashant G, Parekh A. A case report of rod migration into cerebellum through foramen magnum after lateral mass fixation of cervical spine. Acta Neurochir (Wien). 2016. 158: 741-4
6. Mahtabfar A, Mazza J, Franco D, Gonzalez GA, Hines K, Chalouhi N. Cranial settling causing intracranial hemorrhage through violation of the skull base by cervical spine instrumentation. World Neurosurg. 2021. 145: 178-82
7. Plant JG, Ruff SJ. Migration of rod through skull, into brain following C1-C2 instrumental fusion for os odontoideum: A case report. Spine (Phila Pa 1976). 2010. 35: E90-2
8. Roy-Camille R, Gaillant G, Bertreaux D, McKibben B, editors. Early management of spinal injuries. Recent Advances in Orthopedics. Edinburgh: Churchill-Livingstone; 1979. p. 57-87
9. Yablon IG, Cowan S, Mortara R. The migration of a Harrington rod after cervical fusion. Spine (Phila Pa 1976). 1993. 18: 356-8