- Department of Rehabilitation Medicine, Toho University Graduate School of Medicine, Ota-ku, Tokyo, Japan.
- Department of Orthopaedic Surgery, Toho University Graduate School of Medicine, Ota-ku, Tokyo, Japan.
- Department of Oral Surgery, Toho University Omori Medical Center, Ota-ku, Tokyo, Japan.
Correspondence Address:
Midori Miyagi, Department of Rehabilitation Medicine, Toho University Graduate School of Medicine, Ota-ku, Tokyo, Japan.
DOI:10.25259/SNI_547_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Midori Miyagi1, Hiroshi Takahashi2, Hideki Sekiya3, Satoru Ebihara1. Role of preoperative cervical alignment on postoperative dysphagia after occipitocervical fusion. 12-Jul-2021;12:350
How to cite this URL: Midori Miyagi1, Hiroshi Takahashi2, Hideki Sekiya3, Satoru Ebihara1. Role of preoperative cervical alignment on postoperative dysphagia after occipitocervical fusion. 12-Jul-2021;12:350. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10958
Abstract
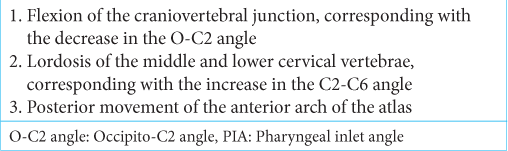
Background: Dysphagia is one of the most serious complications of occipitocervical fusion (OCF). The previous studies have shown that postoperative cervical alignment, documented with occipito (O)-C2 angles, C2-C6 angles, and pharyngeal inlet angles (PIA), impacted the incidence of postoperative dysphagia in patients undergoing OCF. Here, we investigated the relationship of preoperative versus postoperative cervical alignment on the incidence of postoperative dysphagia after OCF.
Methods: We retrospectively reviewed the clinical data/medical charts for 22 patients following OCF (2006– 2019). The O-C2 angles, C2-C6 angles, PIA, and narrowest pharyngeal airway spaces (nPAS) were assessed using plain lateral radiographs of the cervical spine before and after the surgery. The severity of dysphagia was assessed with the functional oral intake scale (FOIS) levels as documented in medical charts; based on this, patients were classified into the nondysphagia (FOIS: 7) versus dysphagia (FOIS: 1–6) groups.
Results: Seven patients (35%) experienced dysphagia after OCF surgery. Preoperative PIA and nPAS were smaller in the dysphagia group. Spearman rank correlation showed a positive correlation between preoperative PIA and FOIS and between preoperative nPAS and FOIS.
Conclusion: This study suggests that preoperative cervical alignment may best predict the incidence of postoperative dysphagia after OCF.
Keywords: Deglutition, Occipitocervical fusion, Preoperative cervical alignment, The functional oral intake scale
INTRODUCTION
Dysphagia is one of the most serious complications of occipitocervical fusion (OCF).[
This study aimed to investigate how differences between preoperative and postoperative cervical alignment contribute to the frequency and severity of postoperative dysphagia following OCF.
MATERIALS AND METHODS
Subjects
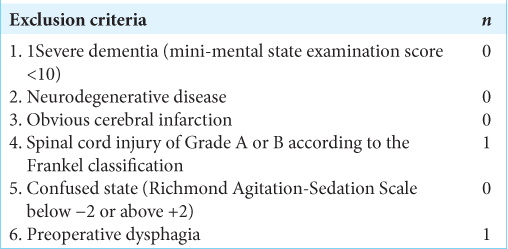
With IRB approval (No. M18017), we retrospectively reviewed the medical charts of patients who underwent OCF at our institute from 2006 to 2019. The major clinical data included; duration of surgery, length of intensive care unit (ICU) stay, duration of ventilator use, and presence or absence of tracheostomy, among others [
Dysphagia evaluation
The severity of dysphagia was assessed using the functional oral intake scale (FOIS) levels determined from the medical chart descriptions of the food intake status of patients.[
According to the FOIS level, patients were classified into nondysphagia (FOIS level: 7) and dysphagia (FOIS level: 1–6) groups. FOIS levels are defined as shown in
Table 3:
The functional oral intake scale.[
Radiographic measurements
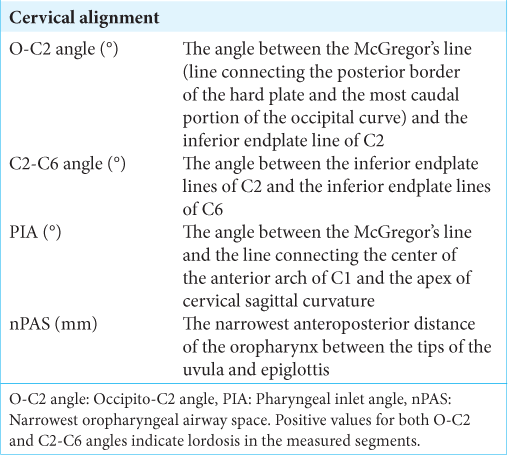
We reviewed plain lateral radiographs of the cervical spine before and after OCF to measure the O-C2 angle, C2-C6 angle, PIA, and nPAS as indicators of the pharyngeal space [
We also estimated the presence of soft-tissue swelling in the prevertebral area on plain lateral radiographs of the cervical spine. Rojas et al. documented the normal range of prevertebral soft-tissue thickness; accordingly, we considered thicknesses >6 mm at C2, 7 mm at C3, or 18 mm at C6 on plain lateral radiographs to represent prevertebral soft-tissue swelling.[
Statistical analysis
The differences in values were compared using the two-tailed t-test, the Mann–Whitney U-test, or χ2 test adequately. Spearman correlation coefficients were used to determine the correlation of the FOIS level with the preoperative cervical alignments. Pearson correlation coefficients were used to evaluate the correlation of continuous variables. Statistical significance was set at P < 0.05. We used SPSS version 17.0 software (SPSS, Chicago, IL, USA) for all analyses.
RESULTS
Based on the FOIS level, the incidence of dysphagia after OCF surgery was 35% [
Radiographic analysis
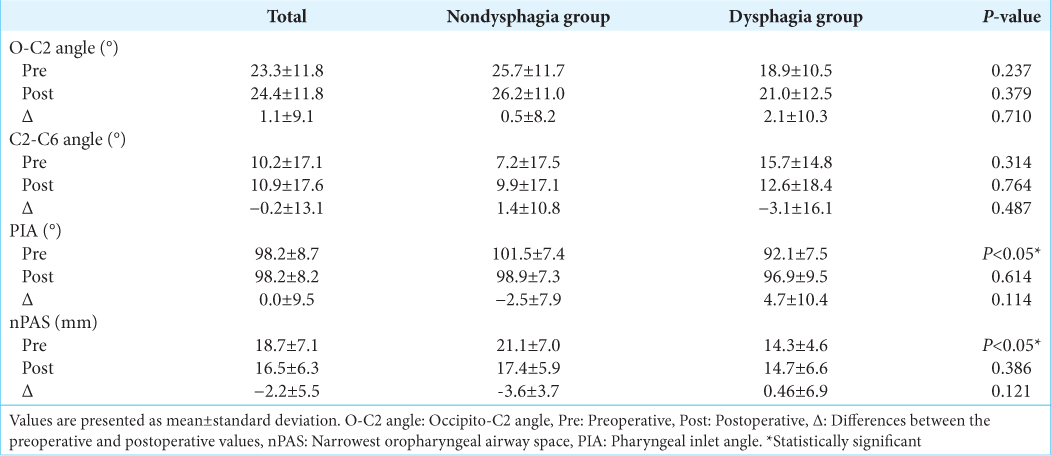
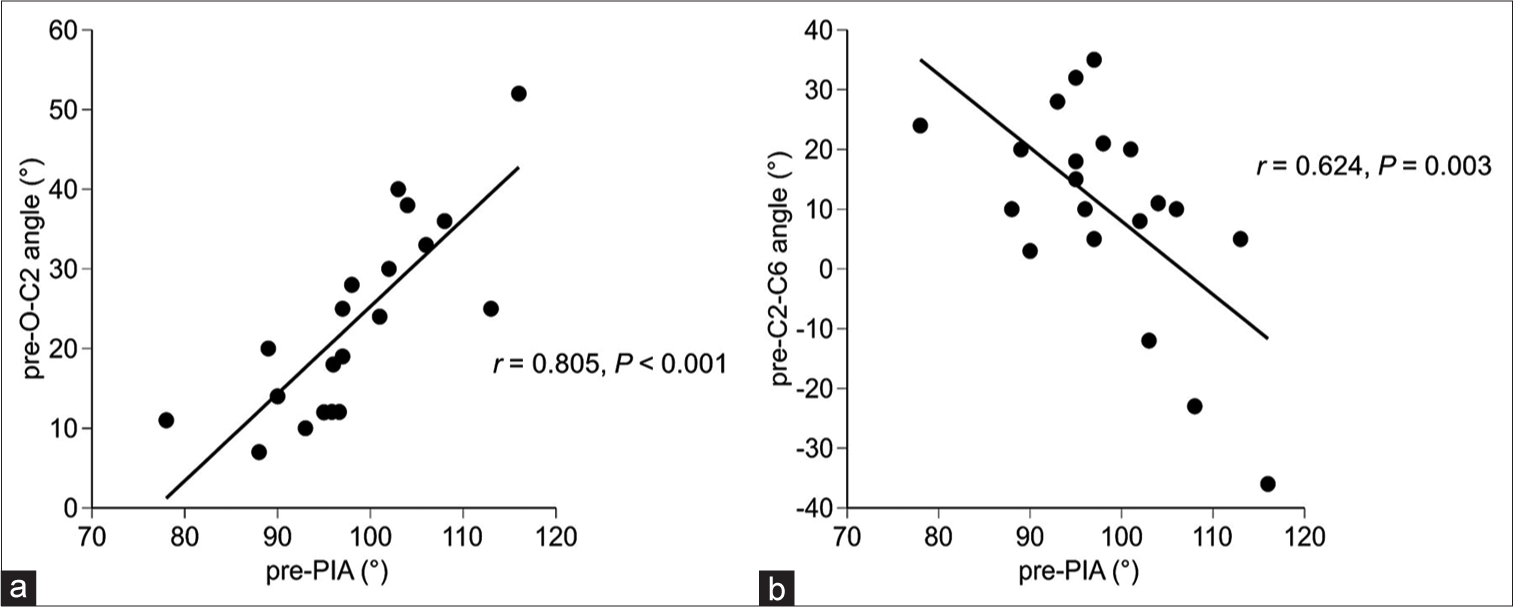
A positive correlation was found between preoperative PIA and FOIS level (r = 0.474, P = 0.035;
DISCUSSION
The results of this study showed that preoperative PIA and nPAS were significantly smaller in the dysphagia group than in the nondysphagia group. Moreover, we found that both preoperative PIA and nPAS were significantly correlated with FOIS level.
The results of this study revealed that a decrease in preoperative PIA could be a predictor of postoperative dysphagia. According to a recent report by Wang et al.,[
A study analyzing the swallowing pressure in healthy participants using high-resolution manometry showed that the duration of lowered swallowing pressure at the upper esophageal sphincter is lesser during the flexion of the craniovertebral junction, which is the first factor leading to a decrease in PIA. Presumably, the bolus passage is inhibited by a decrease in tongue movement and pharyngeal contraction from the flexion of the craniovertebral junction.[
The mean age of the patients in the dysphagia group was 73.0 years. A previous study with independently living older individuals showed that 27% had signs of dysphagia in the oropharyngeal phase, and 23% had dysphagia.[
The previous studies on dysphagia associated with intubation have revealed that even a short intubation duration could be a risk factor for postextubation dysphagia, and hence, endotracheal intubation could be considered a trigger for the incidence of dysphagia. In addition, a previous study reported that postoperative paralysis of the hypoglossal nerve, which is the motor nerve of the tongue, and the vagus nerve, which innervates the pharyngeal contractile muscles, could occur after cervical spinal fusion.[
The following preoperative factors for predicting the postoperative outcomes have been identified: (1) morbidity and severity, (2) cervical alignment, and (3) imaging findings.
In terms of morbidity and severity, the length and severity of the morbid neuropathy during the surgery are the factors contributing to the poor improvement rate.[
All three preoperative factors elucidated in the previous studies are indicators of irreversible functional impairment of the spinal cord. In our study, preoperative factors, rather than postoperative, were associated with postoperative dysphagia, suggesting that preoperative conditions may affect postoperative outcomes.
Since we identified the preoperative radiological measurements related to the incidence of postoperative dysphagia, the measurements might predict dysphagia after OCF surgery. They can be easily measured using the plain lateral radiographs of the cervical spine. If this is possible, performing these measurements in selected patients may help prevent dysphagia and aspiration pneumonia. Further prospective studies are required to evaluate these points.
This study had several limitations, which include its retrospective design and the relatively small sample size. In addition, fiber-optic endoscopic and/or video fluoroscopic analyses of swallowing were not performed for each patient. Another limitation is the lack of analysis using computed tomography and magnetic resonance imaging.
CONCLUSION
In this study, preoperative PIA and nPAS were significantly smaller in patients who developed dysphagia after OCF. These results suggest that preoperative cervical alignment may predict the incidence of dysphagia after OCF.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
JSPS KAKENHI (No. 20K19321, 19H03984, 19K22821).
Conflicts of interest
There are no conflicts of interest.
References
1. Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005. 86: 1516-20
2. Ebata S, Hatsushika K, Ohba T, Nitta K, Akaike H, Masuyama K. Swallowing function after occipitocervical arthrodesis for cervical deformity in patients with rheumatoid arthritis. Neurorehabilitation. 2015. 37: 299-304
3. Hong JT, Lee SW, Son BC, Sung JH, Kim IS, Park CK. Hypoglossal nerve palsy after posterior screw placement on the C-1 lateral mass. Case report. J Neurosurg Spine. 2006. 5: 83-5
4. Ito T, Oyanagi K, Takahashi H, Takahashi HE, Ikuta F. Cervical spondylotic myelopathy, Clinicopathologic study on the progression pattern and thin myelinated fibers of the lesions of seven patients examined during complete autopsy. Spine (Phila Pa 1976). 1996. 21: 827-33
5. Izeki M, Neo M, Takemoto M, Fujibayashi S, Ito H, Nagai K. The O-C2 angle established at occipito-cervical fusion dictates the patient’s destiny in terms of postoperative dyspnea and/or dysphagia. Eur Spine J. 2014. 23: 328-36
6. Kaneyama S, Sumi M, Takabatake M, Kasahara K, Kanemura A, Hirata H. The prediction and prevention of dysphagia after occipitospinal fusion by use of the S-line (swallowing line). Spine (Phila Pa 1976). 2017. 42: 718-25
7. Koyanagi T, Hirabayashi K, Satomi K, Toyama Y, Fujimura Y. Predictability of operative results of cervical compression myelopathy based on preoperative computed tomographic myelography. Spine (Phila Pa 1976). 1993. 18: 1958-63
8. Matsubara K, Kumai Y, Kamenosono Y, Samejima Y, Yumoto E. Effect of three different chin-down maneuvers on swallowing pressure in healthy young adults. Laryngoscope. 2016. 126: 437-41
9. Miyagi M, Takahashi H, Tsuchiya K, Sekiya H, Ebihara S. Role of O-C2 angle in the development of dysphagia in patients with halo-vest fixation. BMC Musculoskelet Disord. 2020. 21: 131
10. Rojas CA, Vermess D, Bertozzi JC, Whitlow J, Guidi C, Martinez CR. Normal thickness and appearance of the prevertebral soft tissues on multidetector CT. AJNR Am J Neuroradiol. 2009. 30: 136-41
11. Serra-Prat M, Hinojosa G, López D, Juan M, Fabré E, Voss DS. Prevalence of oropharyngeal dysphagia and impaired safety and efficacy of swallow in independently living older persons. J Am Geriatr Soc. 2011. 59: 186-7
12. Shamji MF, Cook C, Pietrobon R, Tackett S, Brown C, Isaacs RE. Impact of surgical approach on complications and resource utilization of cervical spine fusion: A nationwide perspective to the surgical treatment of diffuse cervical spondylosis. Spine J. 2009. 9: 31-8
13. Shamji MF, Mohanty C, Massicotte EM, Fehlings MG. The association of cervical spine alignment with neurologic recovery in a prospective cohort of patients with surgical myelopathy: Analysis of a series of 124 cases. World Neurosurg. 2016. 86: 112-9
14. Tetreault LA, Karpova A, Fehlings MG. Predictors of outcome in patients with degenerative cervical spondylotic myelopathy undergoing surgical treatment: Results of a systematic review. Eur Spine J. 2015. 24: 236-51
15. Tian W, Yu J. The role of C2-C7 angle in the development of dysphagia after anterior and posterior cervical spine surgery. Clin Spine Surg. 2017. 30: E1306-14
16. Wang LN, Hu BW, Song YM, Liu LM, Zhou CG, Wang L. Predictive ability of pharyngeal inlet angle for the occurrence of postoperative dysphagia after occipitocervical fusion. BMC Musculoskelet Disord. 2021. 22: 54
17. Wang X, Chou D, Jian F. Influence of postoperative O-C2 angle on the development of dysphagia after occipitocervical fusion surgery: Results from a retrospective analysis and prospective validation. World Neurosurg. 2018. 116: e595-601
18. Yoshida M, Neo M, Fujibayashi S, Nakamura T. Upper-airway obstruction after short posterior occipitocervical fusion in a flexed position. Spine (Phila Pa 1976). 2007. 32: E267-70