- Department of Neurosurgery and Endovascular Neurosurgery, University of Patras, Patra, Achaia, Greece.
- Department of Neurosurgery, University of Patras, Patra, Achaia, Greece.
- Department of Internal Medicine, Division of Hematology, University of Patras, Patra, Achaia, Greece.
- Department of Otorhinolaryngology, Head and Neck Surgery University of Patras, Patra, Achaia, Greece.
- Department of Radiology and Interventional Neuroradiology, University of Patras, Patra, Achaia, Greece.
Correspondence Address:
Vasileios Panagiotopoulos
Department of Radiology and Interventional Neuroradiology, University of Patras, Patra, Achaia, Greece.
DOI:10.25259/SNI_52_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Vasileios Panagiotopoulos1, Andreas Theofanopoulos2, Alexandra Kourakli3, Anargyros Symeonidis3, Valera Krisela3, Nicholas S. Mastronikolis4, Petros Zampakis5. Ruptured infectious ICA pseudoaneurysm into the sphenoid sinus after maxillofacial infection, successfully treated by selective embolization. 26-Apr-2021;12:191
How to cite this URL: Vasileios Panagiotopoulos1, Andreas Theofanopoulos2, Alexandra Kourakli3, Anargyros Symeonidis3, Valera Krisela3, Nicholas S. Mastronikolis4, Petros Zampakis5. Ruptured infectious ICA pseudoaneurysm into the sphenoid sinus after maxillofacial infection, successfully treated by selective embolization. 26-Apr-2021;12:191. Available from: https://surgicalneurologyint.com/surgicalint-articles/10752/
Abstract
Background: Intracranial infectious aneurysms are cerebral aneurysms caused by pathogen-induced inflammation undermining the arterial wall. We present a rare case of inflammatory pseudoaneurysm of cavernous internal carotid artery (ICA).
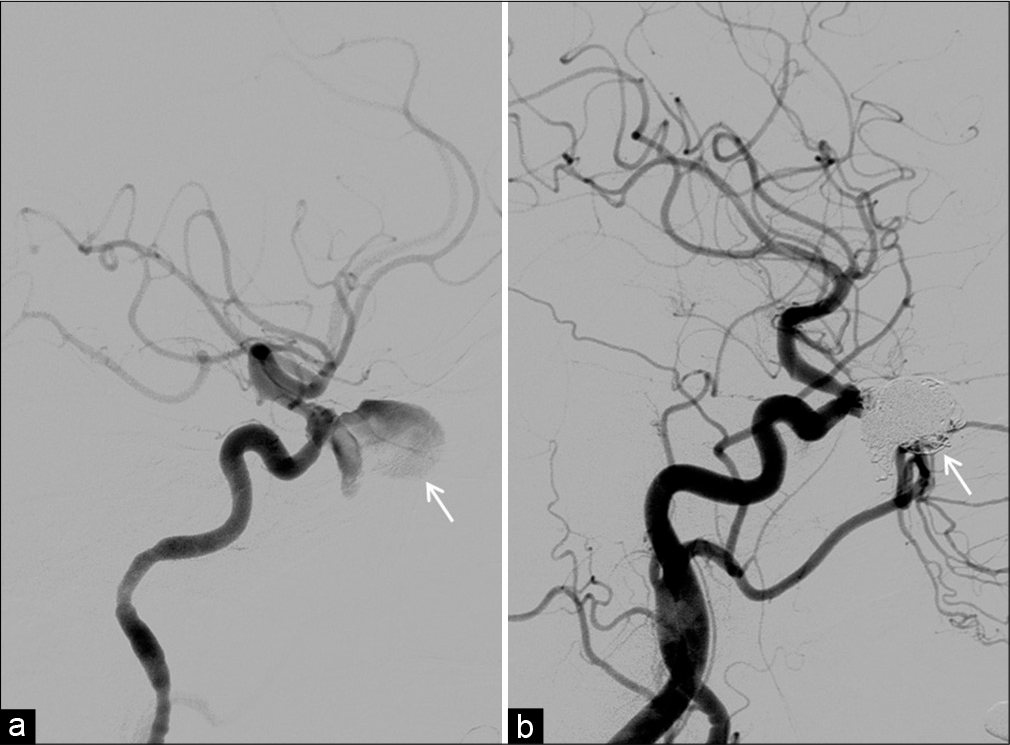
Case Description: A 51-year-old female with a recent diagnosis of acute lymphoblastic leukemia developed maxillofacial infection with Pseudomonas and Acinetobacter after chemotherapy onset. Initial plain computed tomography (CT) revealed bony dehiscence of the left ICA canal, as well as bilateral protrusion of the vessel within the sphenoid sinus. Following infection spread into the left sphenoid sinus, she presented with episodes of intermittent epistaxis, without any profound vascular abnormalities on postcontrast CT. CT angiography that was performed 15 days later, due to refractory epistaxis, illustrated a large narrow necked irregular shape pseudoaneurysm of the left paraophthalmic ICA, extending into the ipsilateral sphenoid sinus. The aneurysm was completely occluded by selective embolization without parent or adjacent vessel sacrifice, documented on both intraoperative and follow-up angiogram, with no recurrence of epistaxis.
Conclusion: Conclusively, ruptured internal carotid infectious aneurysms are rare but potentially fatal causes of epistaxis when extended into the sphenoid sinus. Selective coiling is feasible and can provide definitive treatment of these lesions.
Keywords: Coiling, Epistaxis, Infectious pseudoaneurysm, Maxillofacial infection, Sphenoid sinus
INTRODUCTION
Intracranial infectious aneurysms (traditionally referred to as mycotic aneurysms) are cerebral aneurysms caused by pathogen-induced inflammation undermining the arterial wall. They are relatively rare, accounting for 2.6–6% of all cerebral aneurysms, and are associated with high risk of rupture and mortality.[
We present a rare case of a left paraophthalmic ICA infectious pseudoaneurysm invading the sphenoid sinus which presented with refractory epistaxis, resulting from a multidrug-resistant Pseudomonas and Acinetobacter infection and treated successfully by selective coiling with parent vessel preservation.
CASE REPORT
A 51-year-old female with a recent diagnosis of acute lymphocytic leukemia was admitted to our hospital due to persistent fever and left-sided perioral dysesthesia following initiation of chemotherapy. Clinical examination revealed ulcerous lesions in the patient’s palate. Further laboratory tests were notable for pancytopenia and elevated CRP and ESR. Cultures of tissue samples taken from the oral lesions revealed multidrug-resistant Pseudomonas aeruginosa and Pseudomonas fluorescens and intermediate antibiotic sensitivity Acinetobacter baumannii. Chemotherapy was discontinued and the already instituted empiric antibiotic coverage was adjusted according to antibiograms. Head and facial computed tomography (CT) revealed extensive bone erosion of the maxilla around the dental alveoli without signs of inflammation of the paranasal sinuses. Anatomic variation was the bony dehiscence of the superolateral wall of the left sphenoid sinus [
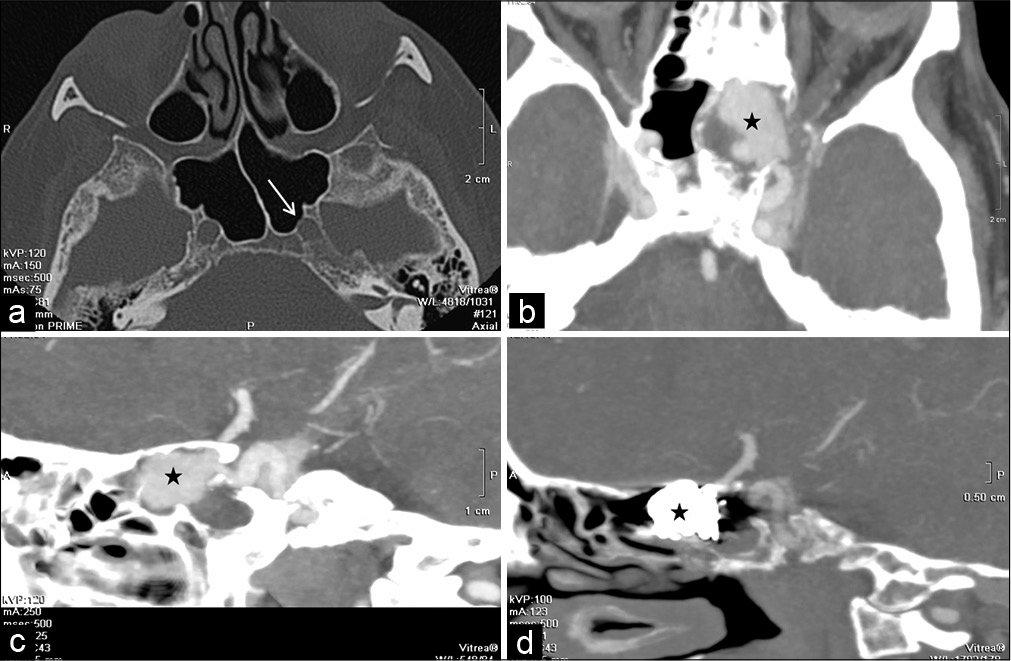
Figure 1:
(a) Bone window computed tomography (CT) demonstrating bony dehiscence of the superolateral wall of the left sphenoid sinus (white arrow). (b and c) Preoperative axial (b) and sagittal reconstruction (c) CT angiography (CTA) showing protrusion of the internal carotid artery (ICA) infectious aneurysm into the left sphenoid sinus (asterisk). (d) Postoperative sagittal CTA demonstrating complete occlusion of the aneurysm (asterisk) and good patency of the supraclinoid ICA.
DISCUSSION
Whereas usually benign, sphenoid sinus infection has the potential to cause life-threatening complications in the form of ruptured infectious intracranial aneurysms of the ICA, especially in immunocompromised individuals.[
Prompt securing of the aneurysm should be prioritized; we suggest that endovascular occlusion by coiling is a safe and efficient minimally invasive technique of preventing rebleeding, without always necessitating either parent vessel sacrifice or stenting. Stenting may be pursued at a later stage, when hemorrhagic complications are deemed acceptably reduced, if aneurysm recurrence is documented at follow-up. Furthermore, a high index of clinical suspicion is paramount to early recognition. Clinicians should have a low threshold for performing a CTA in patients with persistent epistaxis, as it is rapid and sensitive enough for timely detection of ruptured infectious pseudoaneurysms.
CONCLUSION
Ruptured infectious intracranial ICA aneurysm as a result of infection spread from a paranasal sinus infection is a rare but potentially fatal cause of epistaxis, especially when accompanied by an uncommon anatomic variation in the form of bony dehiscence of the superolateral wall of the sphenoid sinus. Embolization is a minimally invasive technique which can provide efficient treatment in ruptured infectious aneurysms protruding inside the sphenoid sinus and – barring particularities in the morphology and location of the lesion – should be offered as a first-line lifesaving procedure.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Azar MM, Assi R, Patel N, Malinis MF. Fungal mycotic aneurysm of the internal carotid artery associated with sphenoid sinusitis in an immunocompromised patient: A case report and review of the literature. Mycopathologia. 2016. 181: 425-33
2. Clare CE, Barrow DL. Infectious intracranial aneurysms. Neurosurg Clin N Am. 1992. 3: 551-66
3. Ducruet AF, Hickman ZL, Zacharia BE, Narula R, Grobelny BT, Gorski J. Intracranial infectious aneurysms: a comprehensive review. Neurosurg Rev. 2010. 33: 37-46
4. Gibelli D, Cellina M, Gibelli S, Cappella A, Oliva AG, Termine G. Relationship between sphenoid sinus volume and protrusion of internal carotid artery and optic nerve: a 3D segmentation study on maxillofacial CT-scans. Surg Radiol Anat. 2019. 41: 507-12
5. Zheng Y, Lu Z, Shen J, Xu F. Intracranial Pseudoaneurysms: Evaluation and Management. Front Neurol. 2020. 11: 582