- Department of Neurosurgery, Nagoya University School of Medicine, Nagoya, Aichi, Japan.
Correspondence Address:
Yusuke Nishimura, Department of Neurosurgery, Nagoya University School of Medicine, Nagoya, Aichi, Japan.
DOI:10.25259/SNI_606_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Motonori Ishii, Yusuke Nishimura, Yoshitaka Nagashima, Takafumi Tanei, Masahiro Nishihori, Takashi Izumi, Ryuta Saito. Sacral arteriovenous fistula with lower thoracic cord edema without perimedullary vein enlargement. 18-Aug-2023;14:295
How to cite this URL: Motonori Ishii, Yusuke Nishimura, Yoshitaka Nagashima, Takafumi Tanei, Masahiro Nishihori, Takashi Izumi, Ryuta Saito. Sacral arteriovenous fistula with lower thoracic cord edema without perimedullary vein enlargement. 18-Aug-2023;14:295. Available from: https://surgicalneurologyint.com/surgicalint-articles/12502/
Abstract
Background: Sacral dural arteriovenous fistulas (AVFs) are often undiagnosed at the initial presentation due to their rarity.
Case Description: For 1 year, a 71-year-old man developed progressive motor and sensory disturbances in both legs. Magnetic resonance imaging showed spinal cord edema with mild contrast enhancement at the T9–10 and T12 levels. Although mild venous dilatation was observed only at the cauda equina level, it was not initially recognized as abnormal. Blood and cerebrospinal fluid tests and spinal angiography of the lower thoracic to upper lumbar levels were nonspecific. The patient was unsuccessfully treated with three courses of high-dose intravenous methylprednisolone. Ultimately, following repeat spinal angiography (i.e., including the bilateral internal iliac arteries) that revealed a low-flow sacral dural AVF supplied by the right lateral sacral artery, the patient underwent successful surgical venous AVF occlusion/transection.
Conclusion: In cases of spinal cord edema without perimedullary abnormal flow voids, careful spinal angiography including the sacral spine is necessary even if only minimal venous dilation is initially observed at the cauda equina level.
Keywords: Magnetic resonance imaging, Sacral dural arteriovenous fistula, Spinal dural arteriovenous fistula
INTRODUCTION
Sacral dural arteriovenous fistulas (AVFs) comprise only 4–9% of all spinal AVFs.[
CASE REPORT
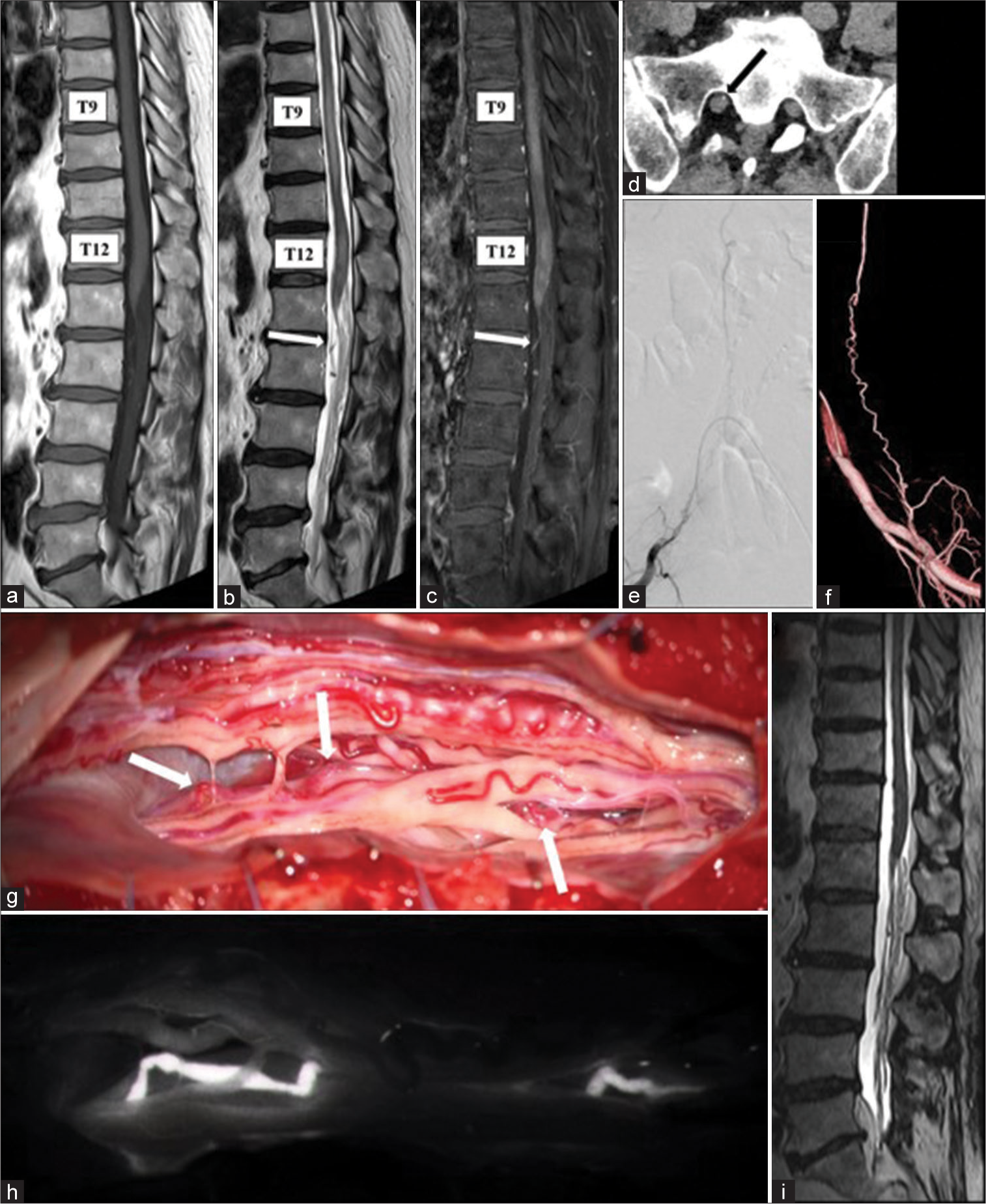
A 71-year-old male presented with 3 months of progressive bilateral lower extremity motor weakness and dysesthesia. The spinal MRI showed two separate levels of spinal cord edema at the T9–10 and T12 levels that were slightly enhanced with contrast-enhanced [
Figure 1:
(a) T1-weighted sequence, (b) T2-weighted sequence, and (c) post-gadolinium T1-weighted sequence – initial magnetic resonance imaging at a local hospital, showing intramedullary edema at T9–10 and T12 levels and a mildly dilated vessel at the cauda equina level (white arrow) without perimedullary vein enlargement. (d) Contrast-enhanced computed tomography image at our hospital, demonstrating a dilated vessel in the right first sacral foramen (black arrow). (e and f) Right internal iliac artery angiograms, showing sacral arteriovenous fistula supplied by the right lateral sacral artery. (g and h) Intraoperative photos showing an arterialized vein (white arrows) along the S1 nerve root visualized early by the indocyanine green without other shunt vessels. (i) Magnetic resonance imaging 5 months after surgery, showing extinguished intramedullary edema.
Surgery
Following an L4–S1 laminectomy, intraoperative indocyanine green angiography revealed an arterialized “red vein” along the right S1 nerve root; no other shunting vessels were detected intradurally [
DISCUSSION
Even in the absence of obvious dilation of the perimedullary veins, sacral dural AVFs should be suspected in cases in which only mildly dilated veins of the cauda equina coexist with edema of the lower thoracic spine. MR findings associated with spinal dural AVFs include spinal cord edema, intramedullary contrast-enhancement, and perimedullary flow voids (i.e., highly suggestive of spinal dural AVFs/present in 85–88% of sacral dural AVFs).[
CONCLUSION
A sacral dural AVF went undiagnosed for over a year in a 71-year-old male. Ultimately, a laminectomy from L4 to S1 allowed for the occlusion/resection of the arterialized AVF vein along the right S1 nerve root.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Brinjikji W, Hilditch CA, Morris JM, Dmytriw AA, Cloft H, Pereira MV. Dilated vein of the filum terminale on MRI: A marker for deep lumbar and sacral dural and epidural arteriovenous fistulas. AJNR Am J Neuroradiol. 2018. 39: 1953-6
2. Domingo RA, De Biase G, Navarro R, Jaime L, Santos JL, Rivas GA. Clinical and radiographic characteristics of sacral arteriovenous fistulas: A multicenter experience. J Neurosurg Spine. 2021. 8: 487-97
3. Jablawi F, Nikoubashman O, Schubert GA, Dafotakis M, Hans FJ, Mull M. Clinical and radiologic characteristics of deep lumbosacral dural arteriovenous fistulas. AJNR Am J Neuroradiol. 2018. 39: 392-8
4. Krings T, Geibprasert S. Spinal dural arteriovenous fistulas. AJNR Am J Neuroradiol. 2009. 30: 639-48