- Department of Spine, Sancheti Institute of Orthopedics and Rehabilitation, Pune, Maharashtra, India.
- Department of Infectious Disease, Sancheti Institute of Orthopedics and Rehabilitation, Pune, Maharashtra, India.
- Department of Research, Sancheti Institute of Orthopedics and Rehabilitation, Pune, Maharashtra, India.
- Medical Director and Chairman, Sancheti Institute of Orthopedics and Rehabilitation, Pune, Maharashtra, India.
Correspondence Address:
Pradhyumn Rathi
Department of Spine, Sancheti Institute of Orthopedics and Rehabilitation, Pune, Maharashtra, India.
DOI:10.25259/SNI_323_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shailesh Hadgaonkar, Pradhyumn Rathi, Bharat Purandare, Ashok Shyam, Parag Sancheti, Arshaj Gaikwad. Salmonella Typhi dorsolumbar spondylodiscitis mimicking tuberculosis – An interesting case report. 11-Jul-2020;11:184
How to cite this URL: Shailesh Hadgaonkar, Pradhyumn Rathi, Bharat Purandare, Ashok Shyam, Parag Sancheti, Arshaj Gaikwad. Salmonella Typhi dorsolumbar spondylodiscitis mimicking tuberculosis – An interesting case report. 11-Jul-2020;11:184. Available from: https://surgicalneurologyint.com/surgicalint-articles/10126/
Abstract
Background: Salmonella rarely causes spinal infections in patients other than those who are immunocompromised or have sickle cell anemia. Further, most cases occurring in healthy individuals have preexisting gastrointestinal infections. Here, we present a case of pyogenic spondylodiscitis attributed to Salmonella Typhi, in an immunologically normal patient without gastrointestinal pathology.
Case Description: A 58-year-old diabetic female complained of lower back pain and malaise. The workup for spinal tuberculosis was negative, but her MRI revealed findings consistent with pyogenic spondylodiscitis (e.g., destruction and instability) for which she required posterior spinal surgery. The organism proved to be S. Typhi; she was treated for 2 months and followed-up for 2 years.
Conclusion: Salmonella spondylodiscitis should be considered among the differential diagnoses for patients with features of infective spondylodiscitis. Culture-specific antibiotics are the cornerstone of treatment, along with appropriate and timely surgery.
Keywords: Diagnosis, Immunocompetent, Salmonella spondylodiscitis, Treatment
INTRODUCTION
Salmonella Typhi causing pyogenic spondylodiscitis was first described by James Paget in 1876.[
Here, we present a 58-year-old immunologically normal female without a significant gastrointestinal history with infective pyogenic spondylodiscitis attributed to S. Typhi, treated with surgical decompression and appropriate antibiotic therapy.
CASE DESCRIPTION
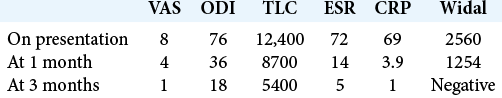
A 58-year-old diabetic female came presented with low back pain of 2 years duration that had exacerbated over the past 4 weeks to the point where she was unable to stand and walk. Her visual analog score was 8 with Oswestry Disability Index of 76. Notably, she had previously empirically received antituberculosis treatment (ATT). On presentation, she was febrile to 100° and had tenderness in the lumbar region with paraspinal spasm. Her neurological examination was intact.
Her total leukocyte count was 12,400/cmm with ESR of 72 mm/h and CRP of 69 mg/L with normal urine report.
X-rays [
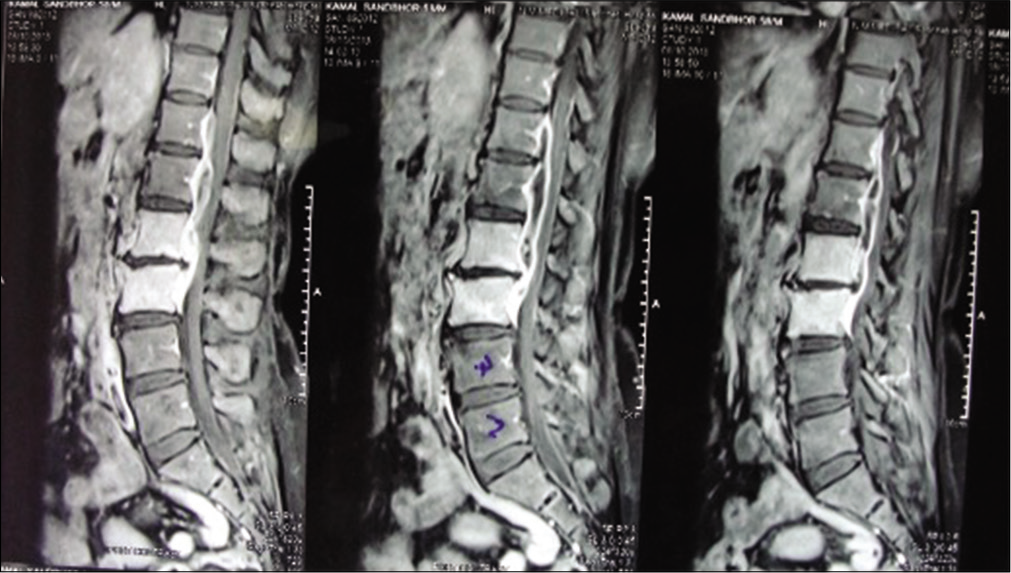
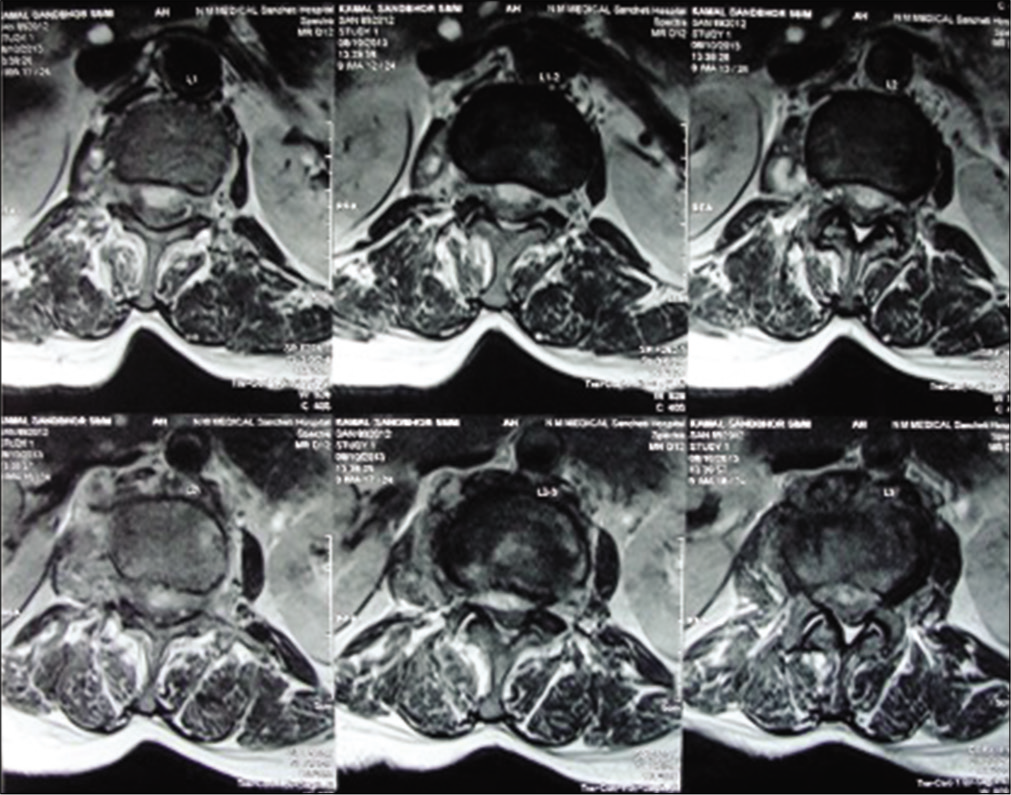
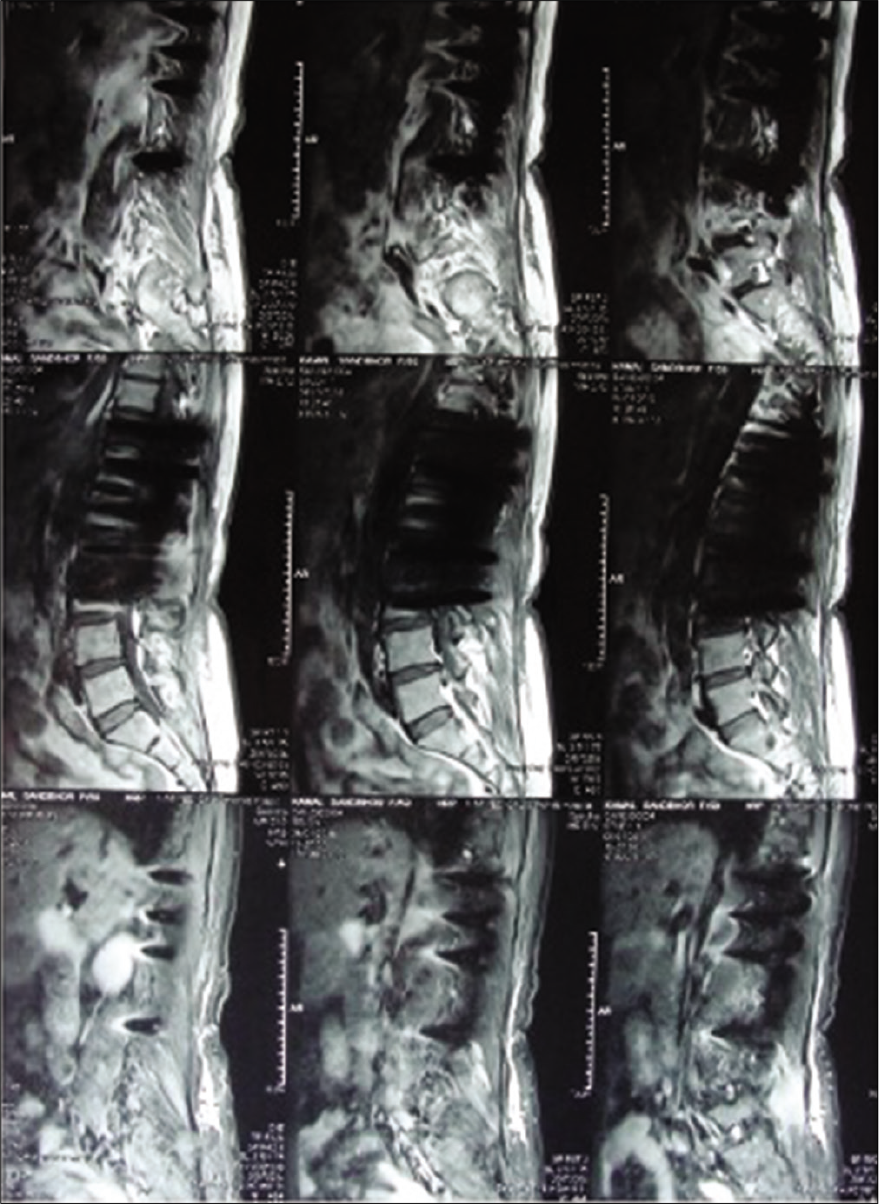
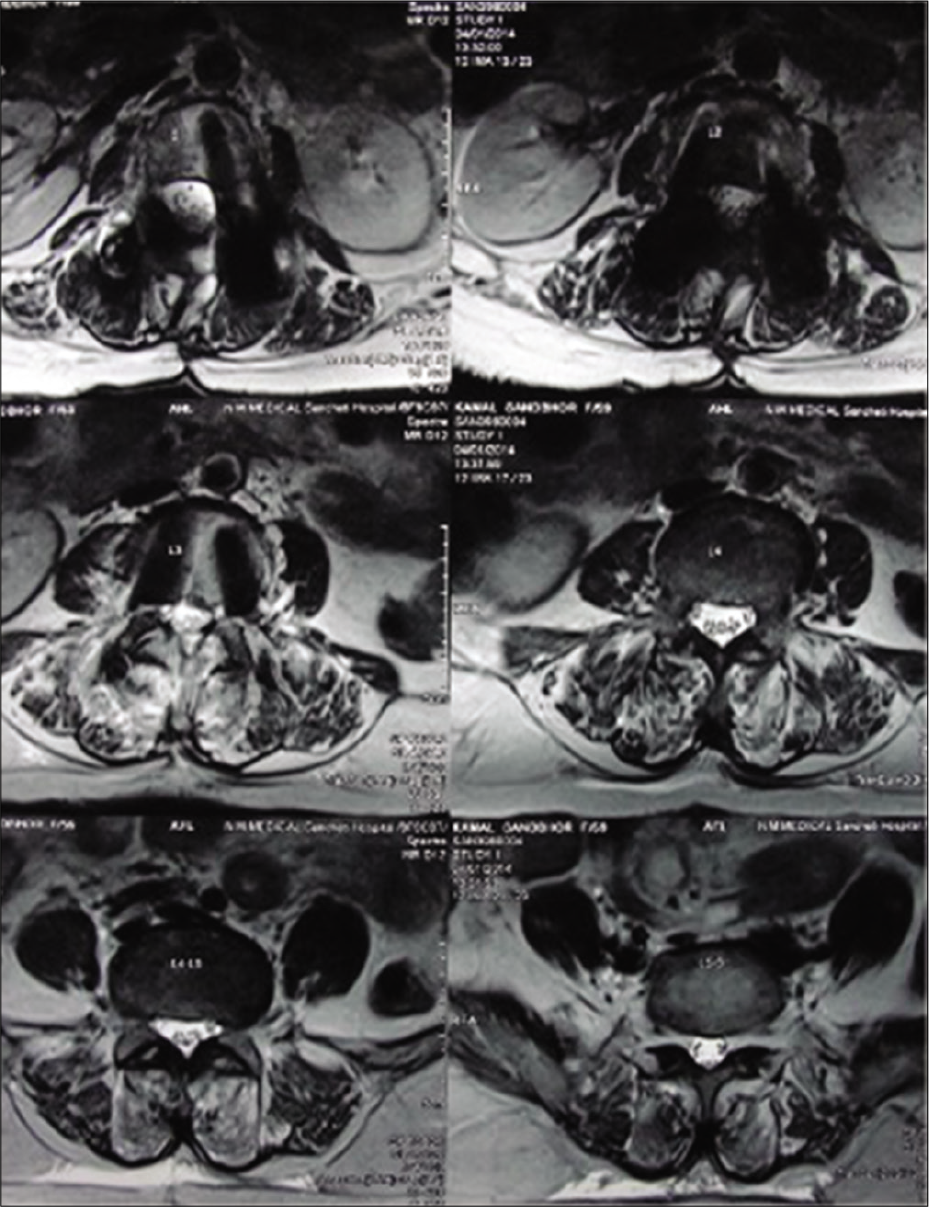
The MR [
Treatment/surgery
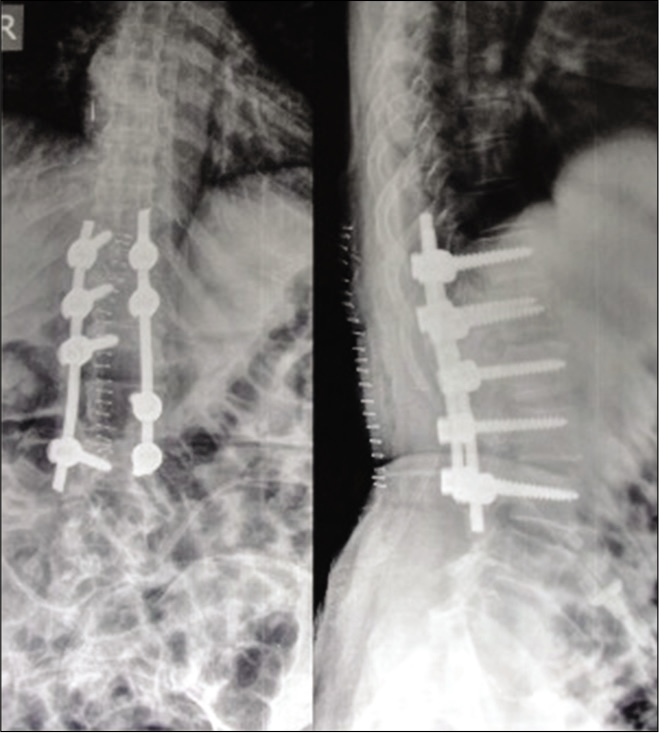
Her anti-tubercular treatment was stopped for a week after which she underwent a D12 to L2 laminectomy, with unilateral D11-D12 facetectomy, debridement/drainage of an anterior epidural abscess with D11-L3 pedicle screw instrumented fusion [
The cultures, after 7 days, were positive for S. Typhi as were the cultures, Widal titer 2560, and drug susceptibility testing suggestive of sensitivity to fluoroquinolone.
She was started intravenous levofloxacin 500 mg single dose daily for 3 weeks. She was discharged after 10 days later on oral levofloxacin 750 mg that was continued till 2 months postoperatively.
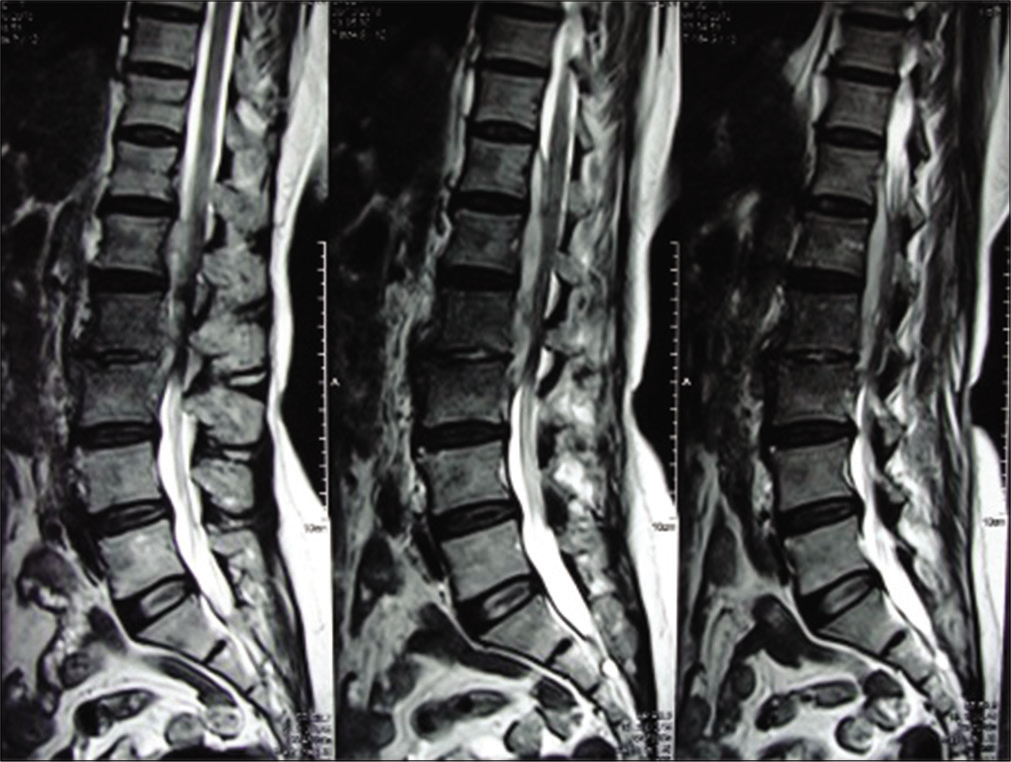
At 3-month follow-up, her MRI [
At 2 years, she was asymptomatic. Moreover, plain X-rays confirmed adequate stabilization [
DISCUSSION
Salmonella osteomyelitis is rare,[
The MRI of our patient suggested pyogenic spondylitis. Furthermore, MRI allows the diagnosis of a tuberculous lesion, with a sensitivity of 100% and specificity of 88%, and tuberculosis being essentially a medical disease, empirical ATT can be considered in India where it is endemic.[
Histopathology may not be completely reliable as there have been reports of Salmonella osteomyelitis presenting as a granulomatous condition with a similar histopathological picture as in tuberculosis, brucellosis, or fungal osteomyelitis.[
Once Salmonella infection is identified, it usually responds to treatment with antibiotics such as chloramphenicol, ciprofloxacin, levofloxacin, ceftriaxone, or ampicillin.[
Indications of surgical interventions include osseous instability, neurologic deficit, or to establish the diagnosis in doubtful case.[
CONCLUSION
Salmonella spondylodiscitis should be considered among the differential diagnoses for patients with features of infective spondylodiscitis. Culture-specific antibiotics are the cornerstone of treatment, along with appropriate and timely surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Banerjee B, Madiyal M, Madhava PK, Agarwal M, Mukhopadhyay C. Typhoid spondylodiscitis mimicking tuberculosis in a teenage girl. J Infect Public Health. 2018. 11: 136-7
2. Carvell JE, Maclarnon JC. Chronic osteomyelitis of the thoracic spine due to salmonella typhi: A case report. Spine (Phila Pa 1976). 1981. 6: 527-30
3. Chang IC. Salmonella spondylodiscitis in patients without sickle cell disease. Clin Orthop Relat Res. 2005. 430: 243-7
4. Chattaway MA, Aboderin AO, Fashae K, Okoro CK, Opintan JA, Okeke IN. Fluoroquinolone-resistant enteric bacteria in Sub-Saharan Africa: Clones, implications and research needs. Front Microbiol. 2016. 7: 558-
5. Jain AK. Tuberculosis of the spine: A fresh look at an old disease. J Bone Joint Surg Br. 2010. 92: 905-13
6. Laloum E, Zeller V, Graff W, Aerts J, Chazerain P, Mamoudy P. Salmonella typhi osteitis can mimic tuberculosis. A report of three cases. Joint Bone Spine. 2005. 72: 171-4
7. Rajesh PK, Mythili S, Subramaniam L. Typhoid spine-a case report. Indian J Med Microbiol. 2004. 22: 128-9
8. Tassinari D, Forti S, Torella M, Tani G. A special case of lower back pain in a 3-year-old girl. BMJ Case Rep. 2013. 2013: bcr0920114796-