- Stroke Center, Sagamihara Kyodo Hospital, Sagamiharashi, Japan
Correspondence Address:
Tatsuki Kimura, Stroke Center, Sagamihara Kyodo Hospital, Sagamiharashi, Japan.
DOI:10.25259/SNI_792_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tatsuki Kimura, Taro Yanagawa, Kazuki Fukumoto, Masaya Sato, Shunsuke Ikeda, Shinichiro Yoshikawa, Tsuyoshi Uesugi, Toshiki Ikeda. Short-term recurrence of stroke following misdiagnosis of carotid web masked by thrombus. 29-Nov-2024;15:441
How to cite this URL: Tatsuki Kimura, Taro Yanagawa, Kazuki Fukumoto, Masaya Sato, Shunsuke Ikeda, Shinichiro Yoshikawa, Tsuyoshi Uesugi, Toshiki Ikeda. Short-term recurrence of stroke following misdiagnosis of carotid web masked by thrombus. 29-Nov-2024;15:441. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13257
Abstract
Background: Carotid webs are a potential cause of occult cerebral infarction. Although they occur frequently, proper diagnosis and treatment are crucial; surgery has been shown to provide a good outcome. Although thrombus on the carotid web have been reported, digital subtraction angiography (DSA)-confirmed cases of pre-dispersed thrombus are rare. In this study, we report a case in which a thrombus on the carotid web concealed a shelf-like defect, complicating its diagnosis.
Case Description: A 47-year-old woman without stroke risk factors presented to our hospital with aphasia and right hemiplegia. On arrival, the symptoms had improved. Magnetic resonance (MR) imaging showed left middle cerebral artery stenosis; however, there was no cerebral infarction. DSA was performed post-admission to examine middle cerebral artery stenosis, which showed no middle cerebral artery stenosis but left internal carotid artery (ICA) origin stenosis and contrast pooling. We diagnosed a transient ischemic attack due to artery-to-artery embolism caused by left ICA stenosis and accompanied by a contralateral carotid web. The same symptoms appeared 6 days later. MR imaging showed a new cerebral infarction and the left middle cerebral artery occlusion. A mechanical thrombectomy procedure revealed a change in ICA origin shape compared to the 1st time, with a shelf-like defect within the carotid web. She subsequently underwent carotid artery stenting and was discharged with mild dysesthesia in her right fingers (modified Rankin Scale of 1).
Conclusion: Thrombus on the carotid web conceals characteristic shelf-like defects and may cause misdiagnosis. However, contrast pooling and contralateral carotid web are important findings for early treatment.
Keywords: Carotid web, Misdiagnosis, Recurrence, Stroke, Thrombus
INTRODUCTION
The carotid web is a shelf-like defect in the posterior wall of the internal carotid artery (ICA) bulb.[
CASE DESCRIPTION
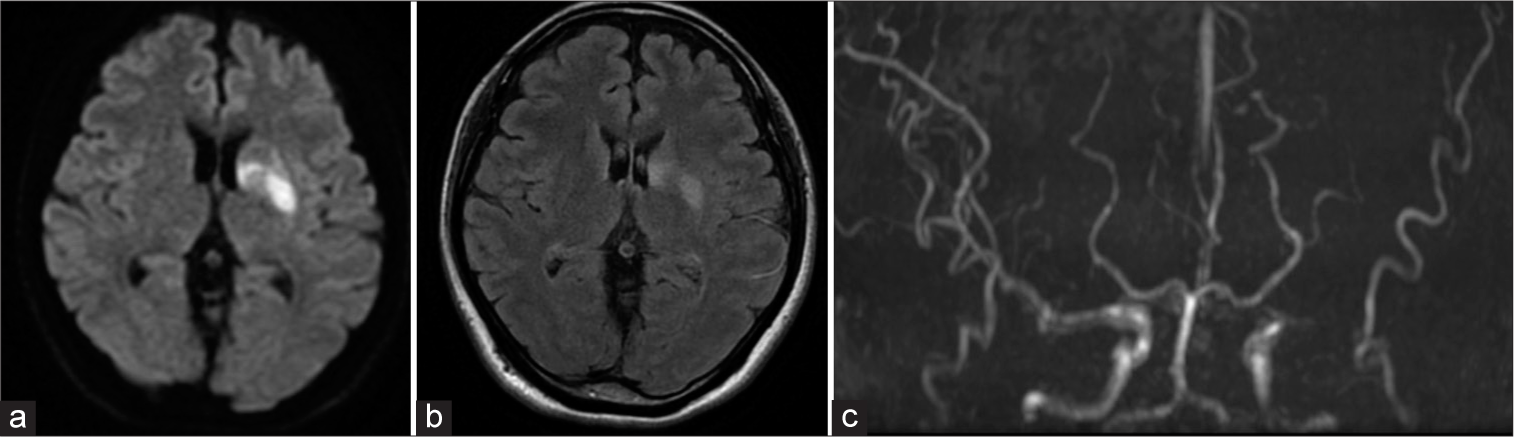
A 47-year-old woman without medical history presented to our hospital with acute onset aphasia and right hemiplegia. The symptoms had improved by the time of the visit. Magnetic resonance (MR) imaging of the head showed left middle cerebral artery stenosis without infarction [
Figure 2:
Digital subtraction angiography performed to examine middle cerebral artery stenosis. (a and b) The angiography of the common carotid artery revealed no stenosis in the middle cerebral artery, previously seen on magnetic resonance imaging. (c) Left common carotid angiography shows stenosis at the origin of the internal carotid artery. (d) Contrast pooling in the left internal carotid artery distal to the web. (e) 3D reconstruction of the left internal carotid artery stenosis. (f) A shelf-like defect is also present in the posterior wall of the origin of the right internal carotid artery. (g) Carotid angiogram in late-phase shows pooling of contrast on the web distal.
Figure 3:
Magnetic resonance (MR) image at the second attack. (a and b) Diffusion-weighted imaging fluid-attenuated inversion recovery shows the high-intensity area from the left caudate nucleus to the insular cortex. (c) Occlusion from the origin of the left middle cerebral artery in MR angiography.
DISCUSSION
During a DSA procedure to investigate middle cerebral artery stenosis in a young woman without atherosclerosis risk factors, we failed to detect a carotid web obscured by a thrombus at the carotid artery origin. Notably, contrast pooling in the web and a contralateral carotid web, even if associated with a thrombus, are important findings in DSA.
The carotid web is frequently observed in young women who do not have the risk factors for atherosclerosis.[
Computed tomography angiography (CTA), DSA, and carotid ultrasound have been reported to diagnose carotid web [
In addition, the carotid web may exist on both sides in 28–58% of cases.[
These two findings typical of the carotid web were still present even with the thrombus on the web. DSA or CTA should be considered, particularly in young women with ischemic stroke in the absence of atherosclerotic factors due to the possibility of a carotid web. Early surgical intervention is necessary when thrombus adhesion is observed on the carotid web due to the possibility of recurrence in a short period.
CONCLUSION
The carotid web should be appropriately diagnosed due to high recurrence rates with conservative treatment and reduced recurrence rates with surgical intervention. Although the thrombus adherence obscures the shelf-like defect, contrast pooling in the carotid web and the presence of the contralateral carotid web are important for establishing a diagnosis based on DSA. When observing these findings, it is crucial to include additional modalities such as CTA. This will help prevent misdiagnosis and facilitate early treatment.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgment
We would like to thank Editage (www.editage.com) for English language editing.
References
1. Compagne KC, Dilba K, Postema EJ, van Es AC, Emmer BJ, Majoie CB. Flow patterns in carotid webs: A patient-based computational fluid dynamics study. AJNR Am J Neuroradiol. 2019. 40: 703-8
2. Coutinho JM, Derkatch S, Potvin AR, Tomlinson G, Casaubon LK, Silver FL. Carotid artery web and ischemic stroke: A case-control study. Neurology. 2017. 88: 65-9
3. Haussen DC, Grossberg JA, Bouslama M, Pradilla G, Belagaje S, Bianchi N. Carotid web (intimal fibromuscular dysplasia) has high stroke recurrence risk and is amenable to stenting. Stroke. 2017. 48: 3134-7
4. Kim SJ, Nogueira RG, Haussen DC. Current understanding and gaps in research of carotid webs in ischemic strokes: A review. JAMA Neurol. 2019. 76: 355-61
5. Liang S, Qin P, Xie L, Niu S, Luo J, Chen F. The carotid web: Current research status and imaging features. Front Neurosci. 2023. 17: 1104212
6. Luo X, Li Z. Ultrasonic risk stratification of carotid web. Echocardiography. 2019. 36: 2103-7
7. Madaelil TP, Grossberg JA, Nogueira RG, Anderson A, Barreira C, Frankel M. Multimodality imaging in carotid web. Front Neurol. 2019. 10: 220
8. Osehobo EM, Nogueira RG, Koneru S, Al-Bayati AR, de Camara CP, Nahab F. Carotid web: An under-recognized and misdiagnosed ischemic stroke etiology. J Neurointerv Surg. 2022. 14: 138-42
9. Ozaki D, Endo T, Suzuki H, Sugiyama SI, Endo K, Itabashi R. Carotid web leads to new thrombus formation: Computational fluid dynamic analysis coupled with histological evidence. Acta Neurochir (Wien). 2020. 162: 2583-8
10. Patel SD, Otite FO, Topiwala K, Saber H, Kaneko N, Sussman E. Interventional compared with medical management of symptomatic carotid web: A systematic review. J Stroke Cerebrovasc Dis. 2022. 31: 106682
11. Pereira BJ, Batista UC, Tosello RT, Ströher IN, Baeta AM, Piske RL. Web vessels: Literature review and neurointerventional management. World Neurosurg. 2018. 110: e907-16
12. Semerano A, Mamadou Z, Desilles JP, Sabben C, Bacigaluppi M, Piotin M. Carotid webs in large vessel occlusion stroke: Clinical, radiological and thrombus histopathological findings. J Neurol Sci. 2021. 427: 117550
13. Wang Y, Li HL, Xu XH, Ye JH, Li J. New asymptomatic thrombosis caused by carotid web during the acute period of cerebral infarction. BMC Neurol. 2023. 23: 264
14. Yu Y, Wang B, Zheng S, Kou J, Gu X, Liu T. Carotid web and ischemic stroke: A CT angiography study. Clin Imaging. 2020. 67: 86-90
15. Zhang AJ, Dhruv P, Choi P, Bakker C, Koffel J, Anderson D. A systematic literature review of patients with carotid web and acute ischemic stroke. Stroke. 2018. 49: 2872-6