- Faculty of Medicine, Zagazig University, Zagazig University, Zagazig, Sharkia, Egypt,
- Faculty of Medicine, Al-Azhar University, Cairo, Egypt,
- Faculty of Medicine, South Valley University, Qena, Egypt,
- Omar Shahin Mental Hospital, Cairo, Egypt,
- Department of Neurological Sciences, University of Nebraska Medical Center, Omaha, Nebraska, United States,
- Department of Neurosurgery, National Bank Hospital, Cairo, Egypt,
- Faculty of Medicine, Al-Azhar University, New Damietta, Egypt,
- Department of Research, Association of Future African Neurosurgeons, Yaounde, Cameroon, Africa,
- Neurosurgery Division, Faculty of Health Sciences, University of Bamenda, Bambili, Cameroon, Africa,
- Department of Neurological Surgery, Oregon Health and Science University, Portland, Oregon, United States.
Correspondence Address:
Ahmed Negida, Faculty of Medicine, Zagazig University, Zagazig, Sharkia, Egypt.
DOI:10.25259/SNI_903_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahmed Negida1, Hazem S. Ghaith2, Mohamed Diaa Gabra3, Mohamed Abdelalem Aziz4, Mohamed Elfil5, Haider Al-Shami6, Eshak I. Bahbah7, Ulrick Sidney Kanmounye8, Ignatius Esene9, Ahmed M. Raslan10. Should the direct aspiration first pass technique be advocated over the stent-retriever technique for acute ischemic stroke? A systematic review and meta-analysis of 7692 patients. 08-Dec-2021;12:597
How to cite this URL: Ahmed Negida1, Hazem S. Ghaith2, Mohamed Diaa Gabra3, Mohamed Abdelalem Aziz4, Mohamed Elfil5, Haider Al-Shami6, Eshak I. Bahbah7, Ulrick Sidney Kanmounye8, Ignatius Esene9, Ahmed M. Raslan10. Should the direct aspiration first pass technique be advocated over the stent-retriever technique for acute ischemic stroke? A systematic review and meta-analysis of 7692 patients. 08-Dec-2021;12:597. Available from: https://surgicalneurologyint.com/surgicalint-articles/should-the-direct-aspiration-first-pass-technique-be-advocated-over-the-stent-retriever-technique-for-acute-ischemic-stroke-a-systematic-review-and-meta-analysis-of-7692-patients/
Abstract
Background: The present meta-analysis aimed to synthesize evidence from all published studies with head-to-head data on the outcomes of a direct aspiration first pass technique (ADAPT) and the stent-retriever (SR) in acute ischemic stroke (AIS) patients.
Methods: We searched PubMed, Scopus, Web of Science, and Cochrane Central Register of Controlled Trials from inception to March 2021 for relevant clinical trials and observational studies. Eligible studies were identified, and all relevant outcomes were pooled in the meta-analysis random-effects model of DerSimonian-Laird.
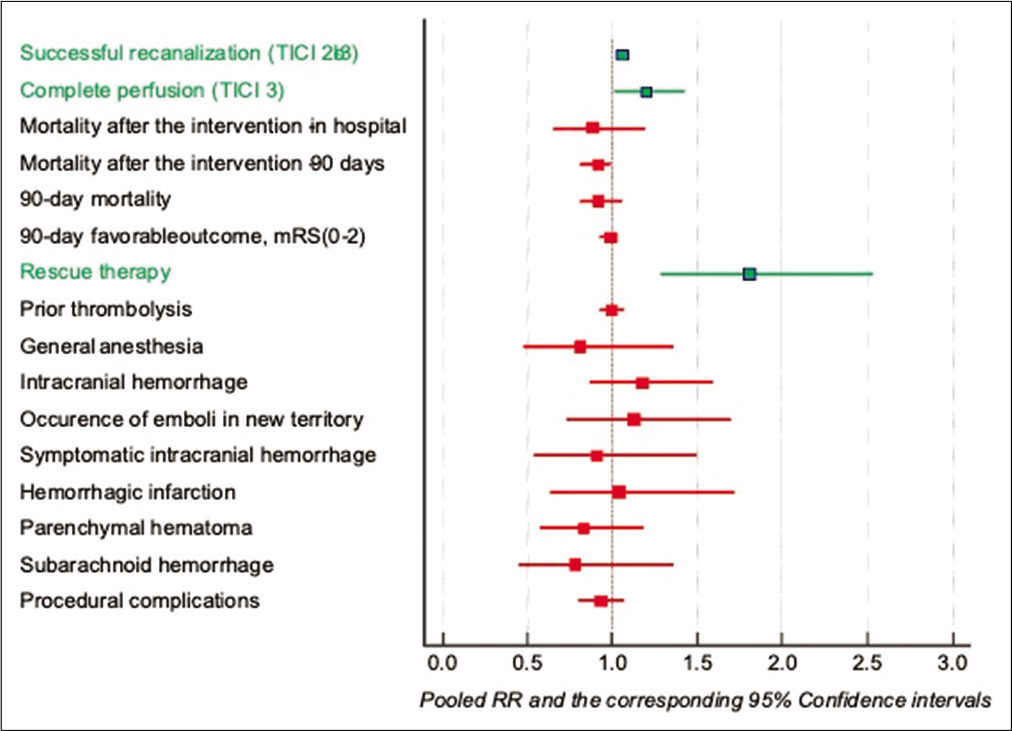
Results: Thirty studies were included in the meta-analysis with a total of 7868 patients. Compared with the SR, the ADAPT provides slightly higher rates of successful recanalization (RR 1.06, 95% CI [1.02 to 1.10]) and complete recanalization (RR 1.20, 95% CI [1.01 to 1.43]) but with more need for rescue therapy (RR 1.81, 95% CI [1.29 to 2.54]). There were no significant differences between the two techniques in terms of mortality at discharge, mortality at 90 days, change in the National Institutes of Health Stroke Scale score, the favorable outcome (modified Rankin scale (mRS) of 0-2), time to the groin puncture, or frequency of complications as intracerebral hemorrhage (ICH), symptomatic intracranial hemorrhage (sICH), embolus in a new territory (ENT), hemorrhagic infarction, parenchymal hematoma, subarachnoid hemorrhage, or procedural complications (all P > 0.05).
Conclusion: Current evidence supports the use of the ADAPT technique to achieve successful and complete recanalization while considering the higher need for rescue therapy in some patients.
Keywords: A direct aspiration first pass technique, Direct aspiration first pass technique, Endovascular therapy, Ischemic stroke, Meta-analysis, Stent retriever, Thrombectomy
INTRODUCTION
Acute ischaemic stroke (AIS) is considered to be one of the leading causes of the mortality worldwide.[
There are two major methods to treat AIS; mechanical thrombectomy and standard medical therapy, which can be considered if patients present to a thrombectomy-capable facility in a timely manner. Over the last decade, several randomized controlled trials (RCTs) showed the superiority of mechanical thrombectomy techniques over medical management in thrombectomy-eligible patients.[
The reference mechanical thrombectomy technique is the stent-retriever (SR) for selected patients, especially those with AIS due to vascular occlusion in the anterior circulation, according to the results of a recently published meta-analysis by Sivan-Hoffmann et al.,[
Recently, a direct aspiration first pass technique (ADAPT) was proposed by Turk et al.[
Therefore, the present meta-analysis aimed to synthesize evidence from all published studies with head-to-head data on the outcomes of ADAPT and SR in AIS patients.
MATERIALS AND METHODS
We followed the most recent version of the preferred reporting items for systematic reviews and meta-analysis (PRISMA statement 2020) guidelines during this systematic review and meta-analysis.[
Eligibility criteria
Studies satisfying the following criteria were included in this meta-analysis:
Population: studies on patients with AIS undergoing thrombectomy Intervention: studies where the exposed group received ADAPT Comparator: studies where the control group received SR Outcome: studies reporting recanalization outcomes, National Institutes of Health Stroke Scale (NIHSS) score at baseline, 24 h and/or 7 days after the stroke event, mRS at 90 days, complications of the procedure and/or procedure time Study design: studies with comparative designs, whether RCTs or observational studies comparing the outcomes of ADAPT and SR.
We excluded studies that were not in English language and studies on either ADAPT or SR without direct comparison between the two techniques.
Information sources
We performed a comprehensive search of four electronic databases (PubMed, Scopus, Web of Science, and Cochrane Central Register of Controlled Trials) from inception to March 1, 2021.
Search strategy
We used the following search query ([aspiration OR ADAPT] AND [SR OR Solitaire OR Trevo OR Merci] AND [stroke OR Large vessel occlusion OR LVO]) in the four databases with no filters or limitations.
Selection process
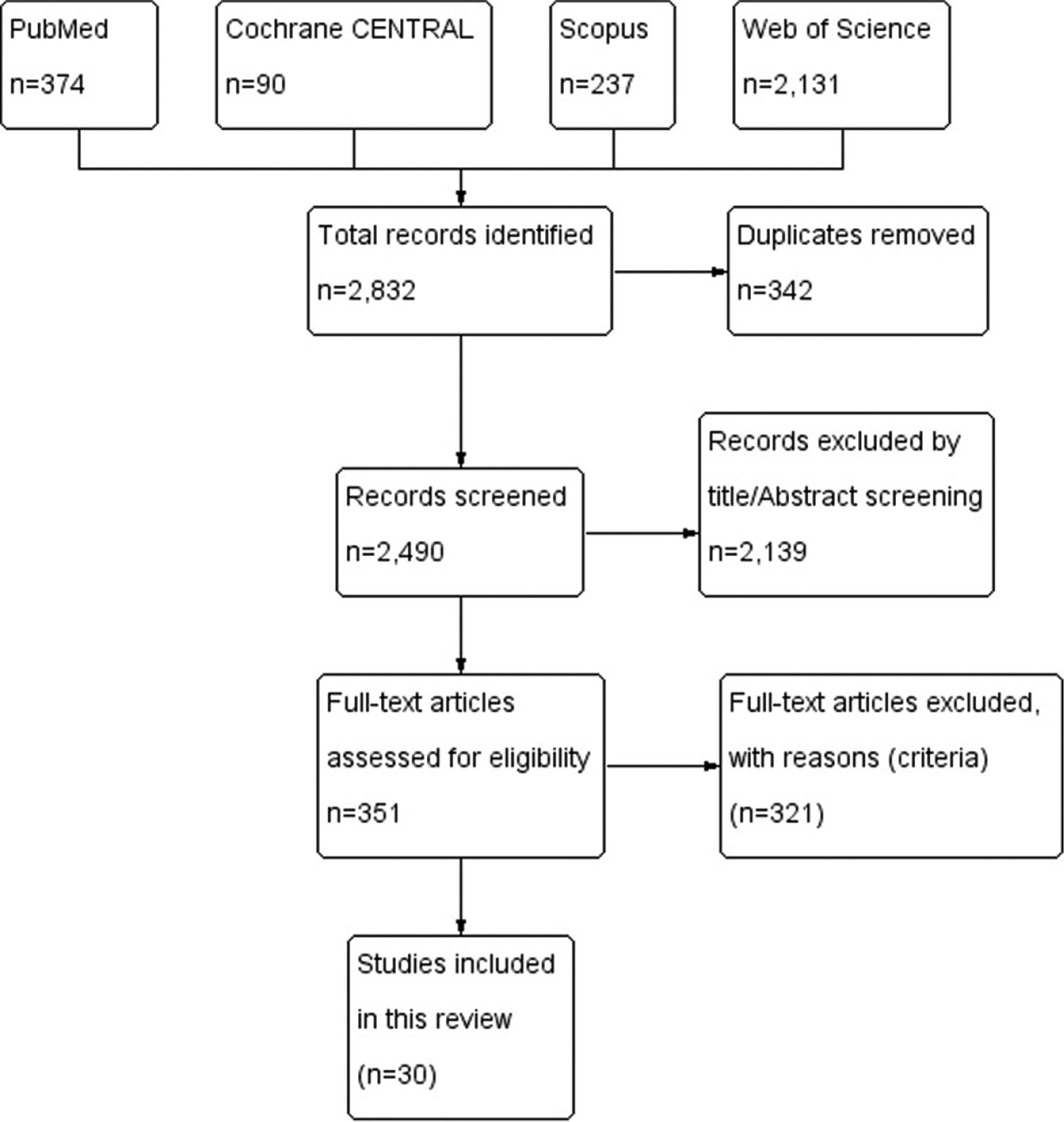
Retrieved records from the literature search were screened in two steps. In the first step, the title and abstracts of all articles were screened for eligibility. Then, the full-text articles of the eligible abstracts were retrieved and further screened for eligibility.
Data collection process and data items
Data were extracted to a uniform data extraction sheet. The extracted data included (1) Characteristics of the included studies, (2) Characteristics of the population of included studies, (3) Risk of bias domains, and (4) Outcome measures.
Study risk of bias assessment
For RCTs, we used the Cochrane Risk of Bias assessment tool (ROB 2.0) while for observational studies; we used the Newcastle Ottawa Scale (NOS scale).
Effect measures
In this meta-analysis, we considered the following outcome measures:
Successful recanalization (%): defined angiographically, according to the modified thrombolysis in cerebral infarction (mTICI) scale, as mTICI2b/3 at the end of the procedure Complete recanalization (%): defined angiographically, according to the mTICI scale, as mTICI-3 at the end of the procedure Favorable neurological outcome (%): defined as the number of patients with an mRS score of 0-2 at 90 days after the stroke event Complications (%): defined as any complication reported in the included studies with a frequency of more than 5%. This includes intracranial hemorrhage (ICH), symptomatic ICH (sICH), Subarachnoid haemorrhage (SAH), parenchymal hematoma, hemorrhagic infarction, and embolization to a new territory (ENT) Procedural time (%): defined as the time interval from groin puncture to reperfusion time.
Synthesis methods
For outcomes that constitute continuous data, the mean difference (MD) between the two groups from the baseline to the endpoint, with its confidence interval (CI), was pooled in the DerSimonian-Laird random-effect model. In the case of studies reporting data in multiple time points, we considered the last endpoint for the primary analysis. For outcomes that constitute dichotomous data, the frequency of events and the total number of patients in each group were pooled as relative risk between the two groups in the DerSimonian-Laird random-effect model.
Subgroup analysis
We conducted subgroup analysis according to the study design (RCTs only vs. observational studies) and according to the site of stroke (anterior circulation vs. posterior circulation).
Assessing the heterogeneity
Heterogeneity (non-combinability) of the included studies and subgroups was examined by visual inspection of the forest plot and assessed by the Cochrane Q and I-square tests using RevMan version 5.3 for windows. For heterogeneity testing, a P < 0.1 and I-square >50% were considered for significant heterogeneity.
Calculating the missing data
When the MD from baseline to endpoint was not provided, we calculated it from the pre- and post-treatment means (MD = Posttreatment-pretreatment). Then, we calculated the MD between the ADAPT and SR groups as follows: (MD = MD experiemental-MD placebo).
When the standard error (SE) of MD was not provided, we calculated it from the standard deviation [SE=SD⁄(√n)], 95% CI ([upper limit-lower limit]⁄3.92), or 90% CI ([upper limit-lower limit]⁄3.29).
For studies and groups with a sample size of <60 patients, the numbers (3.92 and 3.29) were substituted by a value from the table of t distributions with degrees of freedom equal to the group sample size minus 1.
Reporting bias assessment
To explore the publication bias across studies, we constructed funnel plots to present the relationship between effect size and SE. Two methods assessed evidence of publication bias; (1) Egger’s regression test and (2) Begg and Mazumdar rank correlation test (Kendall’s tau).
Certainty assessment
To test the robustness of the evidence, we conducted a certainty assessment through sensitivity analysis (also called, leave-one-out meta-analysis). For every outcome in the meta-analysis, we run sensitivity analysis in multiple scenarios excluding one study in each scenario to make sure the overall effect size was not dependent on any single studies.
RESULTS
Study selection
Our literature search process retrieved 2,832 records. Following titles and abstract screening, 351 articles were eligible for full-text screening. From these 351 studies, 30 studies were included in the meta-analysis.[
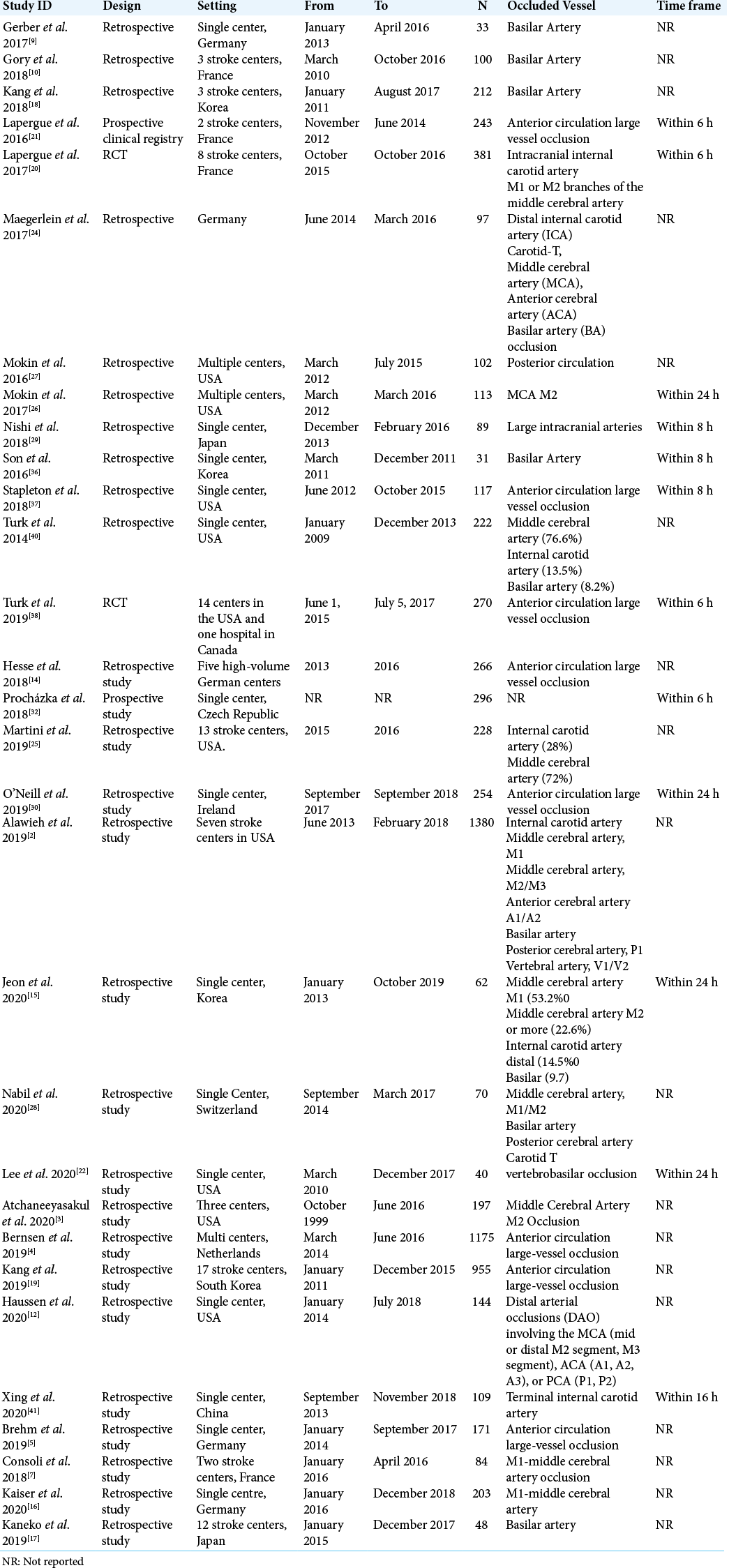
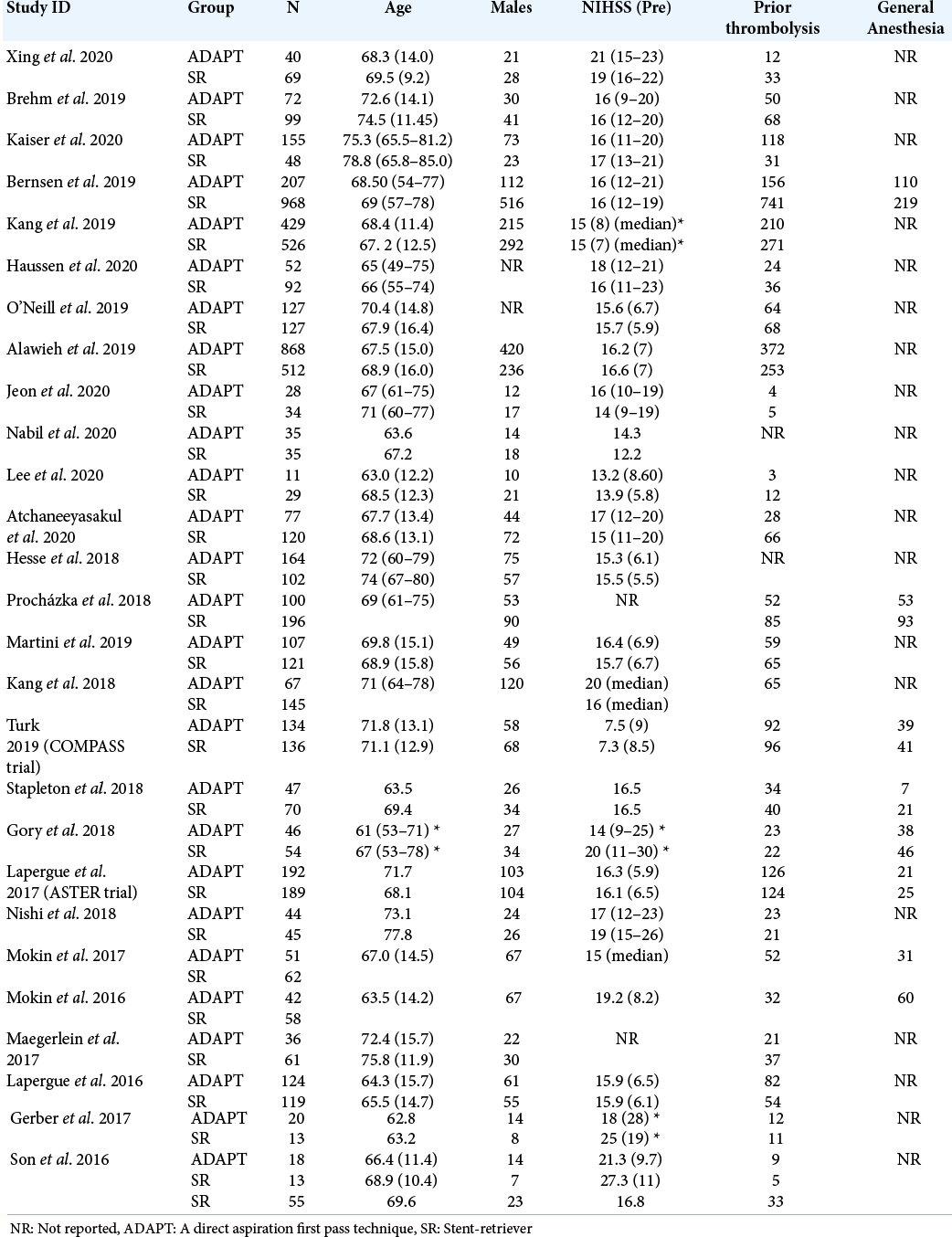
Study characteristics
The population of the studies was homogenous; all studies enrolled 7868 patients with AIS. Two studies were RCTs while 28 studies were observational studies. The characteristics of the included studies are summarized in [
Risk of bias within studies
The quality of included studies ranged from moderate to high quality according to the Cochrane Risk of Bias assessment tool for RCTs and the NOS for the observational studies.
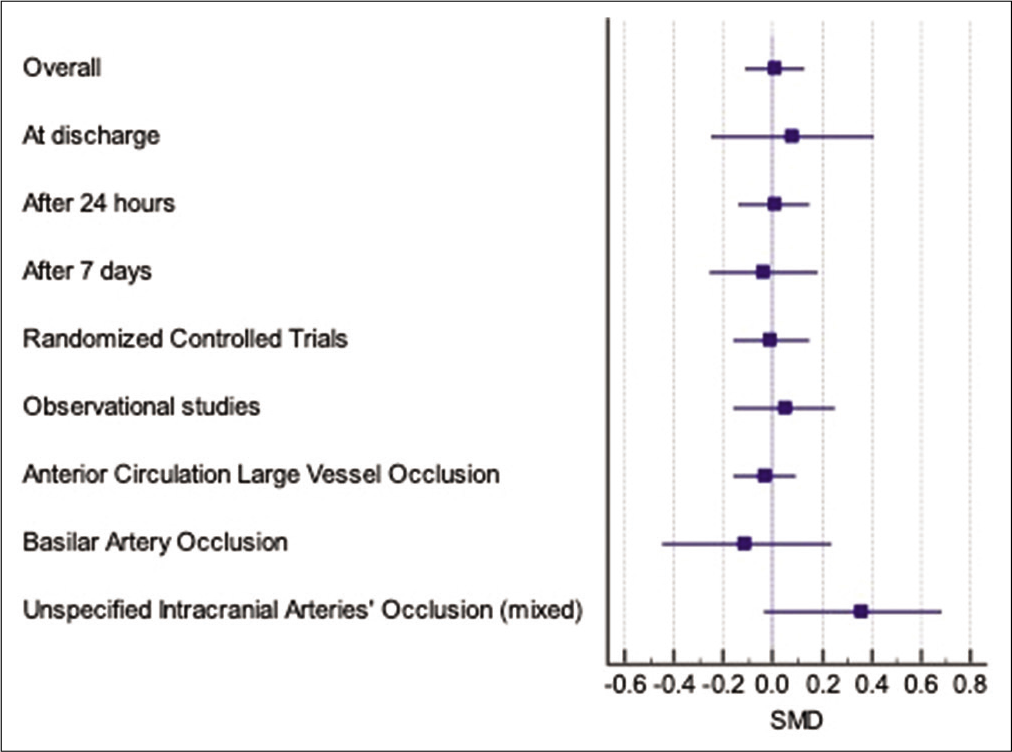
Improvement in NIHSS score
The overall standardized MD (SMD) of improvement in the NIHSS from baseline did not favor either of the two techniques (SMD 0.01, 95% CI [–0.11 to 0.13]). Subgroup analysis did not show any difference between the two techniques after 24 h (SMD 0.01, 95% CI [–0.14 to 0.15]), after 7 days (SMD –0.04, 95% CI [–0.26 to 0.18]) or at discharge (SMD 0.08, 95% CI [–0.25 to –0.41]), [
Figure 2:
Forest plot of the pooled SMD of change in National Institutes of Health Stroke Scale score overall and subgroup by different time points, study designs, and location of vascular occlusion; SMD = standardized mean difference of the change from baseline to endpoint between the A direct aspiration first pass technique and Stent-retriever groups.
Similarly, subgroup analysis of the improvement in the NIHSS according to the site of vascular occlusion did not show superiority of either of the two techniques for the 4 studies conducted on patients with AIS in the anterior circulation occlusion (SMD –0.03, 95% CI [–0.16 to 0.09]), the two studies conducted on patients with basilar artery occlusion (SMD –0.11, 95% CI [–0.45 to 0.24]) or the two studies with (unspecified) intracranial arterial occlusion (SMD 0.36, 95% CI [0.04 to 0.68]). The pooled effect estimates on all subgroups were homogenous (Chi-square P > 0.1) [
Time to groin puncture
The pooled analysis of the time to groin puncture reported by 18 studies (n = 5729 patients) did not favor either of the two techniques (SMD 0.81, 95% CI [–11.78 to 13.40]). The difference was not statistically significant in the subgroups of the RCTs or the observational studies [
Successful recanalization (TICI 2b-3)
Twenty-nine studies (n = 7560 patients) reported the frequency of achieving successful recanalization (TICI 2b-3) by both techniques. The pooled risk ratio (RR) of successful recanalization (TICI 2b-3) favored aspiration thrombectomy technique (RR 1.06, 95% CI [1.02 to 1.10]) [
Figure 3:
Forest plot summarizing the pooled RR of the dichotomous study outcomes between the A direct aspiration first pass technique and stent-retriever groups; outcomes in green are statistically significant. The green colour means a significant difference exists while the red colour means no significant difference exists.
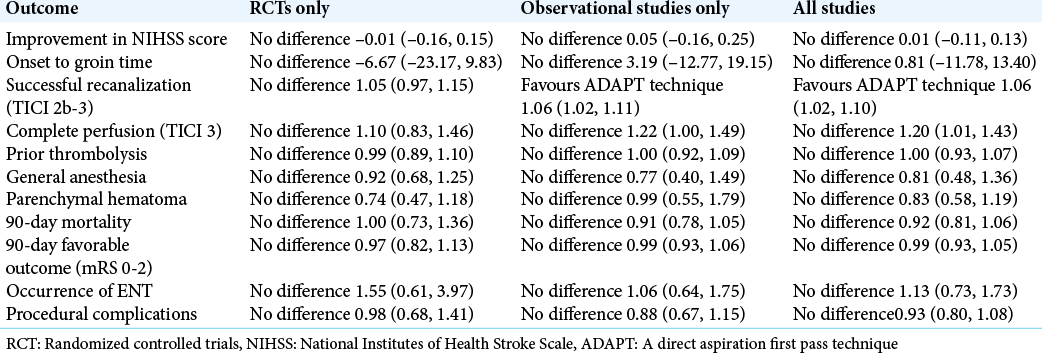
Subgroup analysis of the rates of successful recanalization (TICI 2b-3) according to the study design showed that the observational studies (1.06, 95% CI [1.02 to 1.11]) but not the RCTs (1.05, 95% CI [0.97 to 1.15]) had statistically significant pooled RR in favor of the ADAPT group.
Complete recanalization (TICI 3)
Seventeen studies (n=3824 patients) reported the frequency of achieving complete perfusion (mTICI 3) by both techniques, the pooled RR of complete perfusion (mTICI 3) favored the ADAPT technique (RR 1.20, 95% CI [1.01 to 1.43]) [
Subgroup analysis of the complete perfusion (mTICI 3) according to the study design showed that the pooled RR did not favor any of both techniques either in the RCTs (RR 1.10, 95% CI [0.83 to 1.46]) or in the observational studies (RR 1.22, 95% CI [1.0 to 1.49]).
Mortality
Five studies (n = 729 patients) reported the in-hospital mortality while ten studies (n = 2901 patients) reported the 90-day mortality. Neither the pooled RR of the in-hospital mortality nor the 90-day mortality favored either of the two groups (RR 0.89 and RR 0.92; both P > 0.05) [
Favorable outcome (mRS of 0-2)
The frequency of patients with favorable outcome according to the mRS score (ranging from 0 to 2) was reported by 22 studies (n = 6244 patients), the pooled RR of favorable outcome (mRS 0-2) did not favor either of the two techniques (RR 0.99, 95% CI [0.93 to 1.05]) [
Rescue therapy
The frequency of the patients who required rescue therapy was reported by 15 studies (n = 3079 patients), the pooled RR of rescue therapy showed that more patients in the ADAPT group required rescue therapy compared with the SR group (RR 1.81, 95% CI [1.29 to 2.54]) [
Prior thrombolysis
The frequency of patients with prior thrombolysis was reported by 23 studies (n = 6763 patients), the pooled RR of prior thrombolysis did not favor either of the two techniques (RR 1.00, 95% CI [0.93 to 1.07]) [
General anesthesia
The frequency of patients who underwent general anesthesia was reported by 7 studies (n = 3561 patients), the pooled RR of the frequency of general anesthesia did not favor either of the two techniques (RR 0.81, 95% CI [0.48 to 1.36]) [
Intracerebral haemorrhage
The frequency of patients with ICH was reported by 8 studies (n = 2063 patients), the pooled RR of intracranial haemorrhage did not favor either of the two techniques (RR 1.22, 95% CI [0.90 to 1.66]) [
Occurrence of embolus in a new territory
The frequency of patients with ENT was reported by 11 studies (n = 1876 patients), the pooled RR of occurrence of an embolus in a new territory did not favor either of the two techniques (RR 1.13, 95% CI [0.73 to 1.73]) [
Symptomatic intracerebral haemorrhage
The frequency of patients with sICH was reported by 14 studies (n = 4504 patients), the pooled RR of symptomatic intracranial haemorrhage did not favor either of the two techniques (RR 0.91, 95% CI [0.54 to 1.54]) [
Haemorrhagic infarction
The frequency of the patients with haemorrhagic infarction was reported by 3 studies (n = 626 patients), the pooled RR of haemorrhagic infarction did not favor either of the two techniques (RR 1.04, 95% CI [0.63 to 1.72]) [
Parenchymal hematoma
The frequency of patients with parenchymal hematoma was reported by 9 studies (n = 1389 patients), the pooled RR of parenchymal hematoma did not favor either of the two techniques (RR 0.83, 95% CI [0.58 to 1.19]) [
SAH
The frequency of SAH in the two groups was reported by 9 studies (n = 1289 patients), the pooled RR of SAH did not favor either of the two techniques (RR 0.78, 95% CI [0.45 to 1.37]) [
Procedural complications
The frequency of patients with procedural complications was reported by 9 studies (n = 3916 patients), the pooled RR of procedural complications did not favor either of the two techniques (RR 0.93, 95% CI [0.80 to 1.08]) [
Subgroup analysis
We conducted subgroup analysis for the main outcomes according to the study design (RCTs only vs. observational studies vs. all studies). Data showed consistent results in both RCTs and observational studies except for the outcome of successful recanalization (TICI 2b-3) where RCTs showed no difference between the ADAPT, and the SR while observational studies reported significantly higher successful recanalization rates in ADAPT compared with the SR [
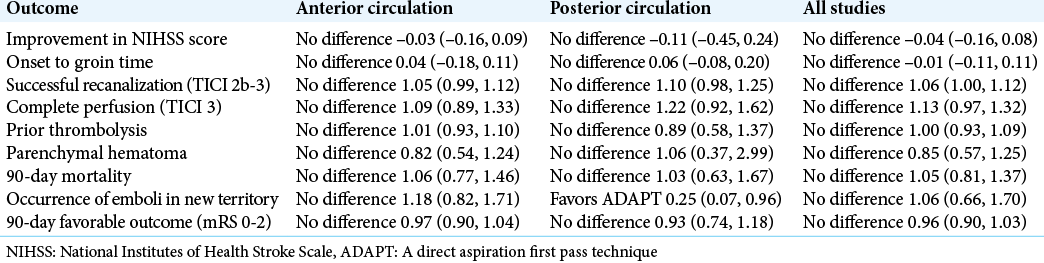
Further, we conducted subgroup analysis for the main outcomes according to the site of stroke (anterior circulation vs. posterior circulation). Data were consistent in the subgroups of anterior circulation and posterior circulation except that the risks of emboli in a new terrorist was significantly lower in the ADAPT compared with the SR in the subgroup of posterior circulation [
DISCUSSION
The development of mechanical thrombectomy technology has revolutionized the treatment of patients with AIS. The SR technique is the current gold-standard mechanical thrombectomy technique used in patients with AIS. However, despite the results of RCTs showing favorable outcomes of this technique, the rate of successful revascularization is still considered suboptimal. Therefore, using large-bore aspiration catheters during routine clinical practice has been widely debated in medical literature.
The ADAPT method was developed by Turk et al.[
Our meta-analysis provides evidence that the ADAPT technique achieves slightly higher rates of successful recanalization and complete recanalization than the conventional SR technique. However, the subgroup analysis showed that this significant effect size in successful recanalization was mainly driven by observational studies but not RCTs. On the contrary, the ADAPT method was associated with higher need for rescue therapy (defined as the use of another endovascular strategy after failure of the initially used technique [mTICI 0-2a]) as compared with the SR. There were no significant differences between the two techniques in terms of mortality at discharge, mortality after 90 days, change in NIHSS score, the favorable outcome (mRS of 0-2), time to the groin puncture, or frequency of complications as ICH, sICH, the occurrence of an embolus in a new territory, hemorrhagic infarction, parenchymal hematoma, SAH, and procedural complications.
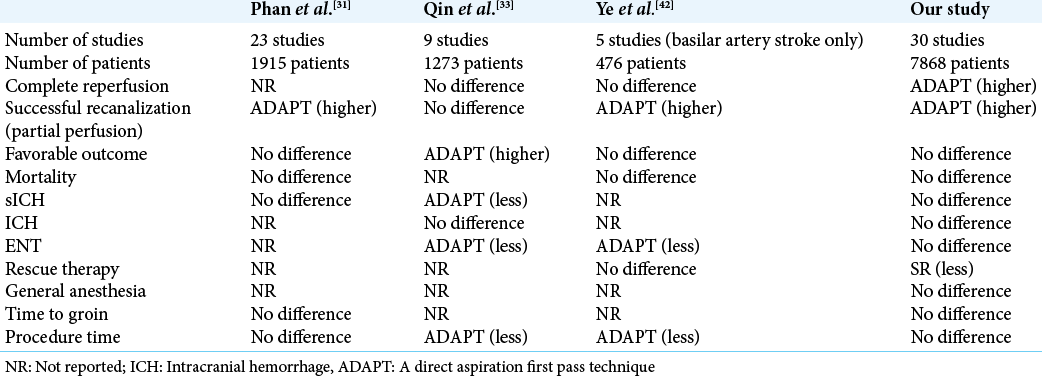
The main finding of our meta-analysis that ADAPT provides higher successful recanalization rates compared with the conventional SR is concordant with the findings of Phan et al.[
Our finding that the ADAPT provides a higher successful recanalization rate and a higher complete recanalization rate (mTICI 3) is reasonable and is supported by the previous literature. Phan et al.[
In terms of the need for rescue therapy, Gory et al.,[
In [
We conducted subgroup analysis according to the study design and site of stroke. These results were consistent across the strata except that the difference in the successful recanalization was significant in observational studies but not in the RCTs suggesting that this difference was mainly driven by observational studies which have less internal validity and higher risk of confounders compared with well-designed RCTs. Besides, in the subgroup of posterior circulation occlusion, the occurrence of ENT was significantly lower in the ADAPT group compared with the SR. These results are consistent with the findings of Ye et al.[
The strengths of our meta-analysis are the following: (1) we ran an extensive search on multiple medical electronic databases; (2) we included all observational studies and clinical trials comparing the two techniques; (3) we followed the guidelines of the Cochrane Handbook for Systematic Reviews of Interventions when conducting this systematic review and we reported this manuscript according to the PRISMA statement. The major limitation of our meta-analysis is that most of the included studies are observational; it is known that observational studies might suffer from confounding bias and are not reliable in establishing a causal relationship between the intervention and the clinical outcome. Only two studies were described as well-designed RCTs, and 28 studies were observational studies, which invites future research to compare both techniques in RCT design to confirm and update our findings.
CONCLUSION
Current evidence supports the use of the ADAPT technique to achieve successful and complete recanalization while considering the higher need for rescue therapy in some patients.
Availability of data, code, and other materials
Data of this study and the Review Manager file (.rm5 file) are available upon request.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Supplementary files available on:
References
1. Adams HP, Davis PH, Leira EC, Chang KC, Bendixen BH, Clarke WR. Baseline NIH stroke scale score strongly predicts outcome after stroke: A report of the trial of org 10172 in acute stroke treatment (TOAST). Neurology. 1999. 53: 126-31
2. Alawieh A, Chatterjee AR, Vargas J, Chaudry MI, Lena J, Turner R. Lessons learned over more than 500 stroke thrombectomies using ADAPT with increasing aspiration catheter size. Neurosurgery. 2020. 86: 61-70
3. Atchaneeyasakul K, Malik AM, Yavagal DR, Haussen DC, Jadhav AP, Bouslama M. Thrombectomy outcomes in acute ischemic stroke due to middle cerebral artery M2 occlusion with stent retriever versus aspiration: A multicenter experience. Interv Neurol. 2020. 8: 180-6
4. Bernsen ML, Goldhoorn RJ, van Oostenbrugge RJ, van Zwam WH, Uyttenboogaart M, Roos YB. Equal performance of aspiration and stent retriever thrombectomy in daily stroke treatment. J Neurointerv Surg. 2019. 11: 631-6
5. Brehm A, Maus V, Tsogkas I, Colla R, Hesse AC, Gera RG. Stent-retriever assisted vacuum-locked extraction (SAVE) versus a direct aspiration first pass technique (ADAPT) for acute stroke: Data from the real-world. BMC Neurol. 2019. 19: 65
6. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015. 372: 1009-18
7. Consoli A, Rosi A, Coskun O, Nappini S, Di Maria F, Renieri L. Thrombectomy for M1-middle cerebral artery occlusion: Angiographic aspect of the arterial occlusion and recanalization: A preliminary observation. Stroke. 2018. 49: 1286-9
8. Donkor ES. Stroke in the 21st century: A snapshot of the burden, epidemiology, and quality of life. Stroke Res Treat. 2018. 2018: 3238165
9. Gerber JC, Daubner D, Kaiser D, Engellandt K, Haedrich K, Mueller A. Efficacy and safety of direct aspiration first pass technique versus stent-retriever thrombectomy in acute basilar artery occlusion-a retrospective single center experience. Neuroradiology. 2017. 59: 297-304
10. Gory B, Mazighi M, Blanc R, Labreuche J, Piotin M, Turjman F. Mechanical thrombectomy in basilar artery occlusion: Influence of reperfusion on clinical outcome and impact of the first-line strategy (ADAPT vs stent retriever). J Neurosurg. 2018. 129: 1482-91
11. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015. 372: 1019-30
12. Haussen DC, Eby B, Al-Bayati AR, Grossberg JA, Rodrigues GM, Frankel MR. A comparative analysis of 3MAX aspiration versus 3 mm Trevo Retriever for distal occlusion thrombectomy in acute stroke. J Neurointerv Surg. 2020. 12: 279-82
13. Hemkens LG, Ewald H, Gloy VL, Arpagaus A, Olu KK, Nidorf M. Colchicine for prevention of cardiovascular events. Cochrane Database Syst Rev. 2016. 2016: CD011047
14. Hesse AC, Behme D, Kemmling A, Zapf A, Hokamp NG, Frischmuth I. Comparing different thrombectomy techniques in five large-volume centers: A “real world” observational study. J Neurointerv Surg. 2018. 10: 525-9
15. Jeon Y, Baik SH, Jung C, Kim JY, Kim BJ, Kang J. Mechanical thrombectomy in patients with acute cancer-related stroke: Is the stent retriever alone effective?. J Neurointerv Surg. 2021. 13: 318-23
16. Kaiser D, Laske K, Winzer R, Hädrich K, Wahl H, Krukowski P. Impact of thrombus surface on first pass reperfusion in contact aspiration and stent retriever thrombectomy. J Neurointerv Surg. 2021. 13: 221-5
17. Kaneko J, Ota T, Tagami T, Unemoto K, Shigeta K, Amano T. Endovascular treatment of acute basilar artery occlusion: Tama-REgistry of acute thrombectomy (TREAT) study. J Neurol Sci. 2019. 401: 29-33
18. Kang DH, Jung C, Yoon W, Kim SK, Baek BH, Kim JT. Endovascular thrombectomy for acute basilar artery occlusion: A multicenter retrospective observational study. J Am Heart Assoc. 2018. 7: e009419
19. Kang DH, Kim JW, Kim BM, Heo JH, Nam HS, Kim YD. Need for rescue treatment and its implication: Stent retriever versus contact aspiration thrombectomy. J Neurointerv Surg. 2019. 11: 979-83
20. Lapergue B, Blanc R, Gory B, Labreuche J, Duhamel A, Marnat G. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: The ASTER randomized clinical trial. JAMA. 2017. 318: 443-52
21. Lapergue B, Blanc R, Guedin P, Decroix JP, Labreuche J, Preda C. A direct aspiration, first pass technique (ADAPT) versus stent retrievers for acute stroke therapy: An observational comparative study. AJNR Am J Neuroradiol. 2016. 37: 1860-5
22. Lee DH, Kim SH, Lee H, Kim S Bin, Lee D. Thrombectomy in acute vertebrobasilar occlusion: A single-centre experience. Neuroradiology. 2020. 62: 723-31
23. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009. 6: e1000100
24. Maegerlein C, Prothmann S, Lucia KE, Zimmer C, Friedrich B, Kaesmacher J. Intraprocedural thrombus fragmentation during interventional stroke treatment: A comparison of direct thrombus aspiration and stent retriever thrombectomy. Cardiovasc Intervent Radiol. 2017. 40: 987-93
25. Martini M, Mocco J, Turk A, Siddiqui AH, Fiorella D, Hanel RA. “Real-world” comparison of first-line direct aspiration and stent retriever mechanical thrombectomy for the treatment of acute ischemic stroke in the anterior circulation: A multicenter international retrospective study. J Neurointerv Surg. 2019. 11: 957-63
26. Mokin M, Primiani CT, Ren Z, Kan P, Duckworth E, Turner RD. Endovascular treatment of middle cerebral artery M2 occlusion strokes: Clinical and procedural predictors of outcomes. Neurosurgery. 2017. 81: 795-802
27. Mokin M, Sonig A, Sivakanthan S, Ren Z, Elijovich L, Arthur A. Clinical and procedural predictors of outcomes from the endovascular treatment of posterior circulation strokes. Stroke. 2016. 47: 782-8
28. Nabil M, Chater G, Correia P, Wegener S, Baltsavias G. Thrombectomy-related emboli: Direct aspiration versus stent retriever thrombectomy for acute ischemic stroke: Our experience and literature review. World Neurosurg. 2020. 135: e588-97
29. Nishi H, Ishii A, Nakahara I, Matsumoto S, Sadamasa N, Kai Y. Different learning curves between stent retrieval and a direct aspiration first-pass technique for acute ischemic stroke. J Neurosurg. 2018. 129: 1456-63
30. O’Neill D, Griffin E, Doyle KM, Power S, Brennan P, Sheehan M. A standardized aspiration-first approach for thrombectomy to increase speed and improve recanalization rates. AJNR Am J Neuroradiol. 2019. 40: 1335-41
31. Phan K, Dmytriw AA, Teng I, Moore JM, Griessenauer C, Ogilvy C. A direct aspiration first pass technique vs standard endovascular therapy for acute stroke: A systematic review and meta-analysis. Clin Neurosurg. 2018. 83: 19-27
32. Procházka V, Jonszta T, Czerny D, Krajca J, Roubec M, Hurtikova E. Comparison of mechanical thrombectomy with contact aspiration, stent retriever, and combined procedures in patients with large-vessel occlusion in acute ischemic stroke. Med Sci Monit Int Med J Exp Clin Res. 2018. 24: 9342-53
33. Qin C, Shang K, Xu SB, Wang W, Zhang Q, Tian DS. Efficacy and safety of direct aspiration versus stent-retriever for recanalization in acute cerebral infarction. Medicine (Baltimore). 2018. 97: e12770
34. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM. Stent-retriever thrombectomy after intravenous t-PA vs t-PA alone in stroke. N Engl J Med. 2015. 372: 2285-95
35. Sivan-Hoffmann R, Gory B, Rabilloud M, Gherasim DN, Armoiry X, Riva R. Patient A meta-analysis and review of the literature. Isr Med Assoc J. 2016. 18: 561-6
36. Son S, Choi DS, Oh MK, Hong J, Kim SK, Kang H. Comparison of Solitaire thrombectomy and Penumbra suction thrombectomy in patients with acute ischemic stroke caused by basilar artery occlusion. J Neurointerv Surg. 2016. 8: 13-8
37. Stapleton CJ, Leslie-Mazwi TM, Torok CM, Hakimelahi R, Hirsch JA, Yoo AJ. A direct aspiration first-pass technique vs stentriever thrombectomy in emergent large vessel intracranial occlusions. J Neurosurg. 2018. 128: 567-74
38. Turk AS, Siddiqui A, Fifi JT, De Leacy RA, Fiorella DJ, Gu E. Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): A multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet (London England). 2019. 393: 998-1008
39. Turk AS, Frei D, Fiorella D, Mocco J, Baxter B, Siddiqui A. ADAPT FAST study: A direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg. 2014. 6: 260-4
40. Turk AS, Spiotta A, Frei D, Mocco J, Baxter B, Fiorella D. Initial clinical experience with the ADAPT technique: A direct aspiration first pass technique for stroke thrombectomy. J Neurointerv Surg. 2018. 10: i20-5
41. Xing PF, Yang PF, Li ZF, Zhang L, Shen HJ, Zhang YX. Comparison of aspiration versus stent retriever thrombectomy as the preferred strategy for patients with acute terminal internal carotid artery occlusion: A propensity score matching analysis. AJNR Am J Neuroradiol. 2020. 41: 469-76
42. Ye G, Lu J, Qi P, Yin X, Wang L, Wang D. Firstline a direct aspiration first pass technique versus firstline stent retriever for acute basilar artery occlusion: A systematic review and meta-analysis. J Neurointerv Surg. 2019. 11: 740-6