- Department of Surgery, Faculty of Medicine, Atma Jaya Catholic University of Indonesia, Jakarta, Indonesia
- Department of Neurosurgery, Loyola University Medical Center, Chicago, USA
- Department of Neurosurgery, Henan Provincial People's Hospital, Zhengzhou Shi, China
Correspondence Address:
Mardjono Tjahjadi
Department of Neurosurgery, Henan Provincial People's Hospital, Zhengzhou Shi, China
DOI:10.4103/sni.sni_311_17
Copyright: © 2018 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mardjono Tjahjadi, Joseph Serrone, Juha Hernesniemi. Should we still consider clips for basilar apex aneurysms? A critical appraisal of the literature. 21-Feb-2018;9:44
How to cite this URL: Mardjono Tjahjadi, Joseph Serrone, Juha Hernesniemi. Should we still consider clips for basilar apex aneurysms? A critical appraisal of the literature. 21-Feb-2018;9:44. Available from: http://surgicalneurologyint.com/surgicalint-articles/should-we-still-consider-clips-for-basilar-apex-aneurysms-a-critical-appraisal-of-the-literature/
Abstract
Background:Basilar apex aneurysms constitute 5–8% of all intracranial aneurysms, and their treatment remains challenging for both microsurgical and endovascular approaches. The perceived drawback of the microsurgical approach is its invasiveness leading to increased surgical morbidity. However, many high-volume centers have shown excellent clinical results with better occlusion rates compared to endovascular treatment. With endovascular therapy taking a larger role in the management of cerebral aneurysms, the future role of microsurgery for basilar apex aneurysm treatment is unclear.
Methods:We performed a literature search to review the microsurgical and endovascular outcomes for basilar apex aneurysms.
Results:Many studies have examined the efficacy of microsurgical and endovascular treatment for intracranial aneurysms, including large randomized trials such as ISAT and BRAT, prospective observational series such as ISUIA, and many single-center retrospective reviews. The recruitment number for posterior circulation aneurysms, specifically for basilar apex aneurysms, was limited in most prospective trials, thus failing to offer clear guidance on basilar apex aneurysm treatment. Recent single-center series report good clinical outcomes between 57–92% for surgical series and 73–96% in endovascular series. The durability of aneurysm occlusion remains superior in surgical cases. The techniques and devices in endovascular treatment have improved treatment aneurysm occlusion rates but more follow-up is needed to confirm long-term durability.
Conclusions:Both microsurgical and endovascular approaches should be complementing each other to treat basilar apex aneurysms. Although endovascular therapy has taken a larger role in the treatment of basilar apex aneurysms, many indications still exist for the use of microsurgery. Advancements in microsurgical techniques and good case selection will allow for acceptably low morbidity after surgical treatment while maintaining its superior durability.
Keywords: Basilar apex aneurysm, endovascular, microsurgical
INTRODUCTION
Basilar apex aneurysms constitute 5–8% of all intracranial aneurysms and about 50% of all posterior circulation aneurysms.[
Microsurgical and endovascular approaches are the two treatment options for basilar apex aneurysms. The perceived drawback of the microsurgical approach is its invasiveness leading to increased surgical morbidity. Many studies have evaluated treatment results of microsurgical and endovascular treatment. However, as basilar apex aneurysms are less frequent than other locations, their optimal management remains controversial.[
Historical perspectives for basilar apex aneurysm treatment
The first successful basilar apex aneurysm obliteration was performed in 1954 using a subtemporal approach by Herbert Olivecrona and his pupil Einar Bohm in Stockholm.[
In 1967, Dr. Gazi Yasargil introduced the operating microscope to neurosurgery. Following the introduction of the microscope, both Dr. Yasargil and Dr. Kenichiro Sugita popularized the pterional approach to basilar apex aneurysms.[
Additional alternative surgical techniques to reach the basilar apex now include the orbitozygomatic, pretemporal, epidural-transcavernous, anterior petrosal, and posterior petrosal approaches.[
To date, the best treatment for basilar apex aneurysms remains debatable.[
The Barrow Ruptured Aneurysm Trial (BRAT) was a single-center study that enrolled all subarachnoid hemorrhage patients resulting in good representation of posterior circulation (16.9%) and basilar apex aneurysms (4.7%). Even though their early results showed that posterior circulation aneurysms did better with endovascular care, there is a lack of anatomical parity of posterior circulation aneurysms between the two assigned cohorts. Posterior inferior cerebellar aneurysms, which incur a poorer outcome, were statistically over represented in the surgical cohort making analysis of outcomes for basilar apex aneurysms more difficult.[
There is less data comparing the surgical and endovascular management of unruptured cerebral aneurysms and even less data for posterior circulation aneurysms. The randomized trials comparing clipping versus coiling of unruptured aneurysms failed to obtain significant recruitment.[
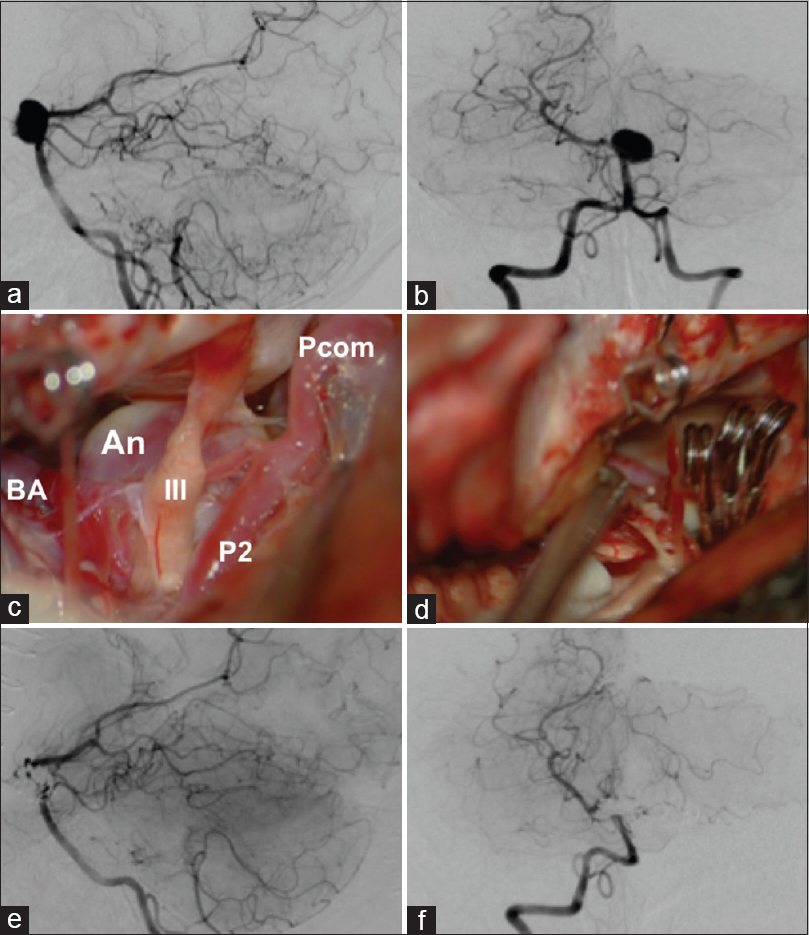
Microsurgical approach basilar apex aneurysm [ Figure 1 ]
Figure 1
(a and b) Anterior and lateral view of angiography showed an unruptured medium sized basilar tip aneurysm. (c and d) A left-sided presigmoid approach was selected to clip the aneurysm. The exposure of the aneurysm and its surrounding structures were excellent and all vital neurovascular structures were preserved. (e and f) Anterior and lateral view of angiography showed total occlusion of the aneurysm while preserving all parent and branches vessels. An = aneurysm; BA = basilar artery; III = third nerve; P2 = second segment of posterior cerebral artery; Pcomm = posterior communicating artery
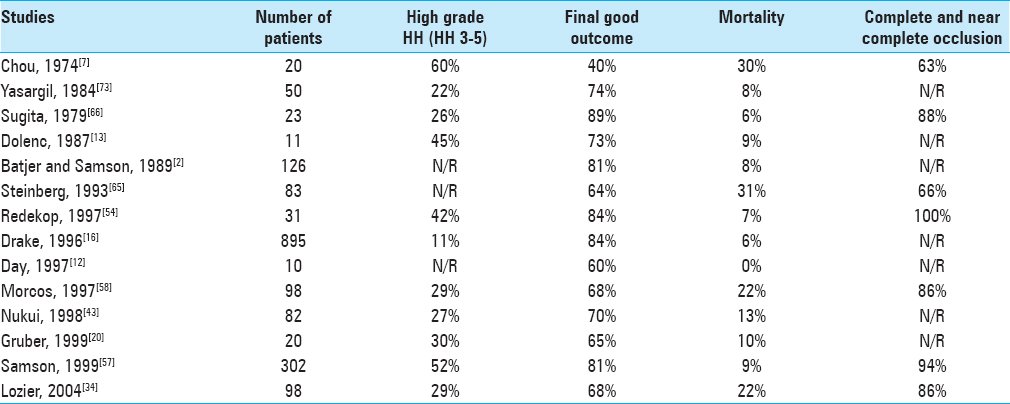
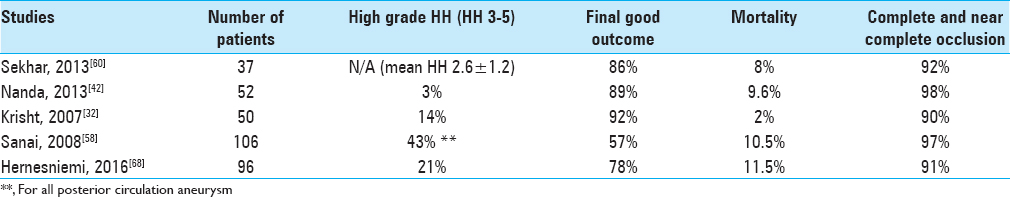
Before ISAT, there were many reports documenting the outcomes of basilar apex aneurysm surgery demonstrating good clinical outcomes of 40–87%. Mortality rates were reported between 0–31% and complete/near complete occlusion rates ranged 63–100% [
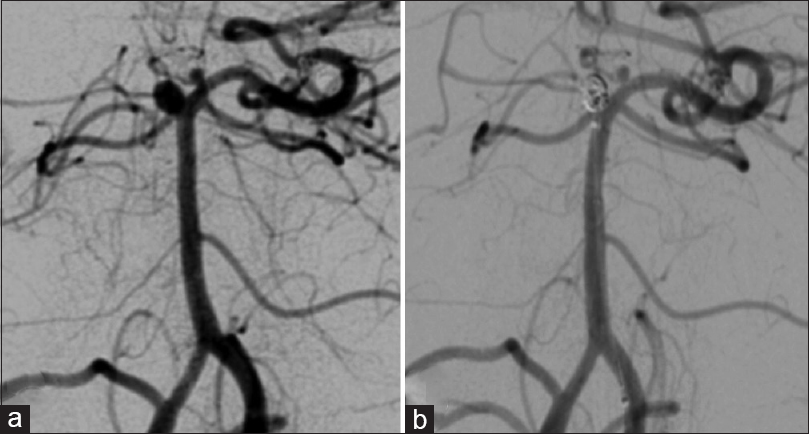
Endovascular approach to basilar apex aneurysm [ Figure 2 ]
The main advantage of endovascular over microsurgical treatment is less invasiveness, thus reducing procedural-related morbidity. However, studies with variable follow-up periods did not find significant differences in the final outcome between treatments.[
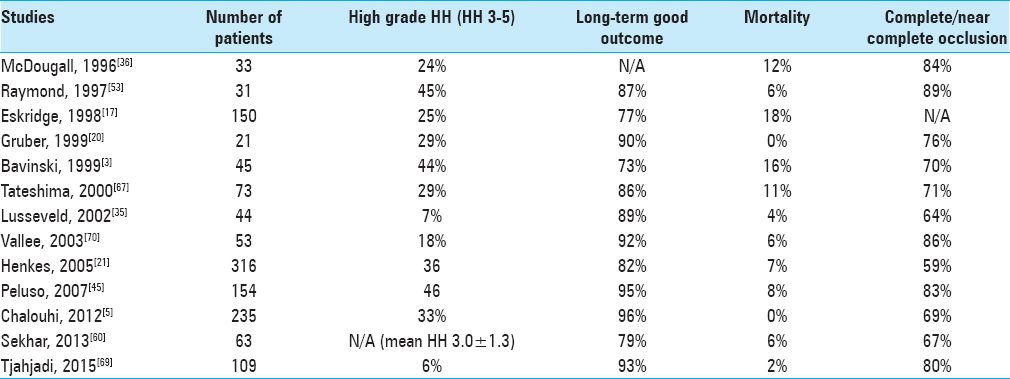
Good clinical outcome with the endovascular treatment of basilar apex aneurysms has been reported between 73% and 96% with mortality rates between 0% and 18% and complete/near complete occlusion rates of 64–89% [
Endovascular treatment of cerebral aneurysms is changing more rapidly than microsurgical treatment. To improve endovascular treatment durability, multiple new devices and techniques have been developed. They include multiple microcatheter techniques, balloon remodeling, various stent-reconstruction, flow-diverters, intrasaccular devices, and devices for neck reconstruction (e.g. PulseRider).[
Intracranial stents have revolutionized the endovascular treatment for cerebral aneurysms. Chalouhi et al. showed an initial occlusion-rate of 88.4% and 87.5% for conventional coiling method and stent-assisted technique, respectively. However, the long-term occlusion rate was improved with stenting (81% at a mean 17.3 months) compared to conventional coiling (61% at a mean follow-up of 27.7 months).[
Future perspective of basilar apex aneurysm treatment
In 2001, Ausman et al. predicted in an editorial paper that there would be a major shift in the paradigm of aneurysm treatment from microsurgery to endovascular procedures.[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ausman JI. The death of cerebral aneurysm surgery. Surg Neurol. 2001. 56: 348-
2. Batjer HH, Samson DS. Causes of morbidity and mortality from surgery of aneurysms of the distal basilar artery. Neurosurgery. 1989. 25: 904-15
3. Bavinzski G, Killer M, Gruber A, Reinprecht A, Gross CE, Richling B. Treatment of basilar artery bifurcation aneurysms by using Guglielmi detachable coils: A 6-year experience. J Neurosurg. 1999. 90: 843-52
4. Brisman JL, Song JK, Newell DW. Cerebral aneurysms. N Engl J Med. 2006. 355: 928-39
5. Chalouhi N, Jabbour P, Gonzalez LF, Dumont AS, Rosenwasser R, Starke RM. Safety and efficacy of endovascular treatment of basilar tip aneurysms by coiling with and without stent assistance: A review of 235 cases. Neurosurgery. 2012. 71: 785-94
6. Cho YD, Rhim JK, Kang HS, Park JJ, Jeon JP, Kim JE. Use of Triple Microcatheters for Endovascular Treatment of Wide-Necked Intracranial Aneurysms: A Single Center Experience. Korean J Radiol. 2015. 16: 1109-18
7. Chou SN, Ortiz-Suarez HJ. Surgical treatment of arterial aneurysms of the vertebrobasilar circulation. J Neurosurg. 1974. 41: 671-80
8. Chow MM, Woo HH, Masaryk TJ, Rasmussen PA. A novel endovascular treatment of a wide-necked basilar apex aneurysm by using a Y-configuration, double-stent technique. AJNR Am J Neuroradiol. 2004. 25: 509-12
9. Cirillo L, Leonardi M, Dall’olio M, Princiotta C, Stafa A, Simonetti L. Complications in the treatment of intracranial aneurysms with silk stents: An analysis of 30 consecutive patients. Interv Neuroradiol. 2012. 18: 413-25
10. Colla R, Cirillo L, Princiotta C, Dall’olio M, Menetti F, Vallone S. Treatment of wide-neck basilar tip aneurysms using the Web II device. Neuroradiol J. 2013. 26: 669-77
11. Darsaut TE, Findlay JM, Magro E. Surgical clipping or endovascular coiling for unruptured intracranial aneurysms: A pragmatic randomised trial. 2017. p.
12. Day JD, Fukushima T, Giannotta SL. Cranial base approaches to posterior circulation aneurysms. J Neurosurg. 1997. 87: 544-54
13. Dolenc VV, Skrap M, Sustersic J, Skrbec M, Morina A. A transcavernous-transsellar approach to the basilar tip aneurysms. Br J Neurosurg. 1987. 1: 251-9
14. Drake CGP SJ, Hernesniemi JA, Drake CGP, SJ, Hernesniemi JA.editors. Small Aneurysms at the Bifurcation of the Basilar Artery: 493 patients. Surgery of Vertebrobasilar Aneurysms: London, Ontario Experience on 1767 patients. Austria: Springer-Verlag; 1996. p. 17-41
15. Drake CG. Bleeding aneurysms of the basilar artery. Direct surgical management in four cases. J Neurosurg. 1961. 18: 230-8
16. Drake CG, Peerless SJ, Hernesniemi JA.editorsSurgery of Vertebrobasilar Aneurysm London, Ontario Experience on 1767 Patients. New York: Springer-Verlag; 1996. p.
17. Eskridge JM, Song JK. Endovascular embolization of 150 basilar tip aneurysms with Guglielmi detachable coils: Results of the Food and Drug Administration multicenter clinical trial. J Neurosurg. 1998. 89: 81-6
18. Fargen KM, Mocco J, Neal D, Dewan MC, Reavey-Cantwell J, Woo HH. A multicenter study of stent-assisted coiling of cerebral aneurysms with a Y configuration. Neurosurgery. 2013. 73: 466-72
19. Gonzalez LF, Amin-Hanjani S, Bambakidis NC, Spetzler RF. Skull base approaches to the basilar artery. Neurosurg Focus. 2005. 19: E3-
20. Gruber DP, Zimmerman GA, Tomsick TA, van Loveren HR, Link MJ, Tew JM, Jr . A comparison between endovascular and surgical management of basilar artery apex aneurysms. J Neurosurg. 1999. 90: 868-74
21. Henkes H, Fischer S, Mariushi W, Weber W, Liebig T, Miloslavski E. Angiographic and clinical results in 316 coil-treated basilar artery bifurcation aneurysms. J Neurosurg. 2005. 103: 990-9
22. Hernesniemi J, Vapalahti M, Niskanen M, Kari A. Management outcome for vertebrobasilar artery aneurysms by early surgery. Neurosurgery. 1992. 31: 857-61
23. Horowitz M, Levy E, Sauvageau E, Genevro J, Guterman LR, Hanel R. Intra/extra-aneurysmal stent placement for management of complex and wide-necked- bifurcation aneurysms: Eight cases using the waffle cone technique. Neurosurgery. 2006. 58: ONS-258-62-
24. Hsu FP, Clatterbuck RE, Spetzler RF. Orbitozygomatic approach to basilar apex aneurysms. Neurosurgery. 2005. 56: 172-7
25. Investigators UJ, Morita A, Kirino T, Hashi K, Aoki N, Fukuhara S. The natural course of unruptured cerebral aneurysms in a Japanese cohort. N Engl J Med. 2012. 366: 2474-82
26. Ishibashi T, Murayama Y, Urashima M, Saguchi T, Ebara M, Arakawa H. Unruptured intracranial aneurysms: Incidence of rupture and risk factors. Stroke. 2009. 40: 313-6
27. Iwamoto H, Kiyohara Y, Fujishima M, Kato I, Nakayama K, Sueishi K. Prevalence of intracranial saccular aneurysms in a Japanese community based on a consecutive autopsy series during a 30-year observation period. The Hisayama study. Stroke. 1999. 30: 1390-5
28. Kato Y, Sano H, Behari S, Kumar S, Nagahisa S, Iwata S. Surgical clipping of basilar aneurysms: Relationship between the different approaches and the surgical corridors. Minim Invasive Neurosurg. 2002. 45: 142-5
29. Kawase T, Toya S, Shiobara R, Mine T. Transpetrosal approach for aneurysms of the lower basilar artery. J Neurosurg. 1985. 63: 857-61
30. Koivisto T, Vanninen R, Hurskainen H, Saari T, Hernesniemi J, Vapalahti M. Outcomes of Early Endovascular Versus Surgical Treatment of Ruptured Cerebral Aneurysms: A Prospective Randomized Study. Stroke. 2000. 31: 2369-77
31. Krisht AF, Kadri PA. Surgical clipping of complex basilar apex aneurysms: A strategy for successful outcome using the pretemporal transzygomatic transcavernous approach. Neurosurgery. 2005. 56: 261-
32. Krisht AF, Krayenbuhl N, Sercl D, Bikmaz K, Kadri PA. Results of microsurgical clipping of 50 high complexity basilar apex aneurysms. Neurosurgery. 2007. 60: 242-50
33. Kwon OK, Kim SH, Kwon BJ, Kang HS, Kim JH, Oh CW. Endovascular treatment of wide-necked aneurysms by using two microcatheters: Techniques and outcomes in 25 patients. AJNR Am J Neuroradiol. 2005. 26: 894-900
34. Lozier AP, Kim GH, Sciacca RR, Connolly ES, Solomon RA. Microsurgical treatment of basilar apex aneurysms: Perioperative and long-term clinical outcome. Neurosurgery. 2004. 54: 286-96
35. Lusseveld E, Brilstra EH, Nijssen PC, van Rooij WJ, Sluzewski M, Tulleken CA. Endovascular coiling versus neurosurgical clipping in patients with a ruptured basilar tip aneurysm. J Neurol Neurosurg Psychiatry. 2002. 73: 591-3
36. McDougall CG, Halbach VV, Dowd CF, Higashida RT, Larsen DW, Hieshima GB. Endovascular treatment of basilar tip aneurysms using electrolytically detachable coils. J Neurosurg. 1996. 84: 393-9
37. McDougall CG, Spetzler RF, Zabramski JM, Partovi S, Hills NK, Nakaji P. The Barrow Ruptured Aneurysm Trial. J Neurosurg. 2012. 116: 135-44
38. Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: A randomized trial. J Stroke Cerebrovasc Dis. 2002. 11: 304-14
39. Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: A randomised trial. Lancet. 2002. 360: 1267-74
40. Molyneux AJ, Kerr RS, Birks J, Ramzi N, Yarnold J, Sneade M. Risk of recurrent subarachnoid haemorrhage, death, or dependence and standardised mortality ratios after clipping or coiling of an intracranial aneurysm in the International Subarachnoid Aneurysm Trial (ISAT): Long-term follow-up. Lancet Neurol. 2009. 8: 427-33
41. Nagashima H, Kobayashi S, Tanaka Y, Hongo K. Endovascular therapy versus surgical clipping for basilar artery bifurcation aneurysm: Retrospective analysis of 117 cases. J Clin Neurosci. 2004. 11: 475-9
42. Nanda A, Sonig A, Banerjee AD, Javalkar VK. Microsurgical Management of Basilar Artery Apex Aneurysms: A Single Surgeon's Experience from Louisiana State University, Shreveport. World Neurosurg. 2014. 82: 118-29
43. Nukui H, Mitsuka S, Hosaka T, Kakizawa T, Horikoshi T, Miyazawa N. Technical points to improve surgical results in cases with basilar tip aneurysms. Neurol Med Chir (Tokyo). 1998. 38: 74-8
44. Peerless SJ, Hernesniemi JA, Gutman FB, Drake CG. Early surgery for ruptured vertebrobasilar aneurysms. J Neurosurg. 1994. 80: 643-9
45. Peluso JP, van Rooij WJ, Sluzewski M, Beute GN. Coiling of basilar tip aneurysms: Results in 154 consecutive patients with emphasis on recurrent haemorrhage and re-treatment during mid- and long-term follow-up. J Neurol Neurosurg Psychiatry. 2008. 79: 706-11
46. Phan K, Huo YR, Jia F, Phan S, Rao PJ, Mobbs RJ. Meta-analysis of stent-assisted coiling versus coiling-only for the treatment of intracranial aneurysms. J Clin Neurosci. 2016. 31: 15-22
47. Phillips TJ, Wenderoth JD, Phatouros CC, Rice H, Singh TP, Devilliers L. Safety of the pipeline embolization device in treatment of posterior circulation aneurysms. AJNR Am J Neuroradiol. 2012. 33: 1225-31
48. Piotin M, Blanc R, Spelle L, Mounayer C, Piantino R, Schmidt PJ. Stent-assisted coiling of intracranial aneurysms: Clinical and angiographic results in 216 consecutive aneurysms. Stroke. 2010. 41: 110-5
49. Pyysalo L, Luostarinen T, Keski-Nisula L, Ohman J. Long-term excess mortality of patients with treated and untreated unruptured intracranial aneurysms. J Neurol Neurosurg Psychiatry. 2013. 84: 888-92
50. Qureshi AI, Janardhan V, Hanel RA, Lanzino G. Comparison of endovascular and surgical treatments for intracranial aneurysms: An evidence-based review. Lancet Neurol. 2007. 6: 816-25
51. Rahal JP, Dandamudi VS, Safain MG, Malek AM. Double waffle-cone technique using twin Solitaire detachable stents for treatment of an ultra-wide necked aneurysm. J Clin Neurosci. 2014. 21: 1019-23
52. Raymond J, Darsaut TE, Molyneux AJ. A trial on unruptured intracranial aneurysms (the TEAM trial): Results, lessons from a failure and the necessity for clinical care trials. Trials. 2011. 12: 64-
53. Raymond J, Roy D, Bojanowski M, Moumdjian R, L’Esperance G. Endovascular treatment of acutely ruptured and unruptured aneurysms of the basilar bifurcation. J Neurosurg. 1997. 86: 211-9
54. Redekop GJ, Durity FA, Woodhurst WB. Management-related morbidity in unselected aneurysms of the upper basilar artery. J Neurosurg. 1997. 87: 836-42
55. Rezek I, Mousan G, Wang Z, Murad MH, Kallmes DF. Effect of core laboratory and multiple-reader interpretation of angiographic images on follow-up outcomes of coiled cerebral aneurysms: A systematic review and meta-analysis. AJNR Am J Neuroradiol. 2013. 34: 1380-4
56. Rinkel GJ, Djibuti M, Algra A, van Gijn J. Prevalence and risk of rupture of intracranial aneurysms: A systematic review. Stroke. 1998. 29: 251-6
57. Samson D, Batjer HH, Kopitnik TA, Jr . Current results of the surgical management of aneurysms of the basilar apex. Neurosurgery. 1999. 44: 697-702
58. Sanai N, Tarapore P, Lee AC, Lawton MT. The current role of microsurgery for posterior circulation aneurysms: A selective approach in the endovascular era. Neurosurgery. 2008. 62: 1236-49
59. Schievink WI, Wijdicks EF, Piepgras DG, Chu CP, O’Fallon WM, Whisnant JP. The poor prognosis of ruptured intracranial aneurysms of the posterior circulation. J Neurosurg. 1995. 82: 791-5
60. Sekhar LN, Tariq F, Morton RP, Ghodke B, Hallam DK, Barber J. Basilar tip aneurysms: A microsurgical and endovascular contemporary series of 100 patients. Neurosurgery. 2013. 72: 284-98
61. Sheth SA, Patel NS, Ismail AF, Freeman D, Duckwiler G, Tateshima S. Treatment of wide-necked basilar tip aneurysm not amenable to Y-stenting using the PulseRider device. BMJ Case Rep 2015. 2015. p.
62. Spetzler RF, McDougall CG, Albuquerque FC, Zabramski JM, Hills NK, Partovi S. The Barrow Ruptured Aneurysm Trial: 3-year results. J Neurosurg. 2013. 119: 146-57
63. Spetzler RF, McDougall CG, Zabramski JM, Albuquerque FC, Hills NK, Russin JJ. The Barrow Ruptured Aneurysm Trial: 6-year results. J Neurosurg. 2015. 123: 609-17
64. Spiotta AM, Derdeyn CP, Tateshima S, Mocco J, Crowley RW, Liu KC. Results of the ANSWER Trial Using the PulseRider for the Treatment of Broad-Necked, Bifurcation Aneurysms. Neurosurgery. 2017. 18: 56-65
65. Steinberg GK, Drake CG, Peerless SJ. Deliberate basilar or vertebral artery occlusion in the treatment of intracranial aneurysms. Immediate results and long-term outcome in 201 patients. J Neurosurg. 1993. 79: 161-73
66. Sugita K, Kobayashi S, Shintani A, Mutsuga N. Microneurosurgery for aneurysms of the basilar artery. J Neurosurg. 1979. 51: 615-20
67. Tateshima S, Murayama Y, Gobin YP, Duckwiler GR, Guglielmi G, Vinuela F. Endovascular treatment of basilar tip aneurysms using Guglielmi detachable coils: Anatomic and clinical outcomes in 73 patients from a single institution. Neurosurgery. 2000. 47: 1332-9
68. Tjahjadi M, Kivelev J, Serrone JC, Maekawa H, Kerro O, Jahromi BR. Factors Determining Surgical Approaches to Basilar Bifurcation Aneurysms and Its Surgical Outcomes. Neurosurgery. 2016. 78: 181-91
69. Tjahjadi M, Kim T, Ojar D, Byoun HS, Lee SU, Ban SP. Long-term review of selected basilar-tip aneurysm endovascular techniques in a single institution. Interdisciplinary Neurosurg. 2017. 8: 50-6
70. Vallee JN, Aymard A, Vicaut E, Reis M, Merland JJ. Endovascular treatment of basilar tip aneurysms with Guglielmi detachable coils: Predictors of immediate and long-term results with multivariate analysis 6-year experience. Radiology. 2003. 226: 867-79
71. Wermer MJ, van der Schaaf IC, Algra A, Rinkel GJ. Risk of rupture of unruptured intracranial aneurysms in relation to patient and aneurysm characteristics: An updated meta-analysis. Stroke. 2007. 38: 1404-10
72. Wiebers DO, Whisnant JP, Huston J, Meissner I, Brown RD, Piepgras DG. Unruptured intracranial aneurysms: Natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003. 362: 103-10
73. Yasargil M.editorsMicroneurosurgery. New York: Thieme Publishing Group; 1984. 1:
74. Yasargil MG, Yasargil MG.editors. Vertebrobasilar Aneurysms. Microneurosurgery: Clinical Considerations, Surgery of the Intracranial Aneurysms and Result. New York: Thieme; 1984. 2: 232-56
75. Yasargil MG, Antic J, Laciga R, Jain KK, Hodosh RM, Smith RD. Microsurgical pterional approach to aneurysms of the basilar bifurcation. Surg Neurol. 1976. 6: 83-91