- Department of Surgery, University of Baghdad, College of Medicine, Baghdad, Iraq
- Department of Surgery, Iraqi Medical Association, Baghdad, Iraq
- Department of Surgery, Baghdad Teaching Hospital, Al Risafa, Baghdad, Iraq
Correspondence Address:
Moneer K. Faraj, Department of Surgery, University of Baghdad, College of Medicine, Al Risafa, Baghdad, Iraq.
DOI:10.25259/SNI_591_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Moneer K. Faraj1, Mohammed Bani Saad2, Mustafa Ismail3. Single bypass fixation for the treatment of lumbar spondylolisthesis: Anatomical insights and technical note. 20-Sep-2024;15:338
How to cite this URL: Moneer K. Faraj1, Mohammed Bani Saad2, Mustafa Ismail3. Single bypass fixation for the treatment of lumbar spondylolisthesis: Anatomical insights and technical note. 20-Sep-2024;15:338. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13108
Abstract
Background: Lumbar spondylolisthesis usually requires surgical management for the stabilization of the spine and to relieve patients of their symptoms. This study aims to provide anatomical insights and evaluate the efficacy of single bypass fixation in the surgical treatment of lumbar spondylolisthesis. This technique aims to stabilize the spine with minimal manipulation of the slipped vertebra, thereby reducing potential complications and improving clinical outcomes.
Methods: This is a retrospective study carried out at a neurosurgical hospital in Baghdad, Iraq, including 35 cases of lumbar spondylolisthesis subjected to single bypass fixation treatment between December 2012 and December 2019. The procedure involves stabilizing the lumbar spine by fixing the vertebrae above and below the affected segment using pedicle screws and rods, guided by fluoroscopy to ensure accurate placement and avoid neurovascular injury. Laminectomy was performed as needed to decompress the spinal cord and nerve roots. Autograft or allograft bone was used to promote fusion around the stabilized segment. Pre- and postoperative clinical and radiological assessments were conducted. Pre- and postoperative clinical and radiological assessments were done.
Results: There have been enormous gains in terms of pain relief, neurological status, and spinal stability, with the achievement of high fusion rates and low complication rates.
Conclusion: Single-level bypass fixation proves efficacy for lumbar stabilization in spondylolisthesis patients, with the best clinical result and less complication for patients.
Keywords: Lumbar spondylolisthesis, Neurological symptoms, Single bypass fixation, Spinal stabilization
INTRODUCTION
Lumbar spondylolisthesis is a type of condition where one vertebra slips over the one below it, causing back pain and possible neurological deficits. This leads to several manipulations of the spine and, hence, more trauma and complications in many of the old fixation techniques.
The single-level bypass fixation is an innovative alternative technique designed to provide stabilization above and below the affected segment, thereby bypassing the instability or fracture. Again, the essence of this procedure is to reduce the potential complications and to produce an improved clinical result.[
Thus, for example, the lumbar spine – again, remember its weight-bearing role and related angle of movement – forms a potential site for spondylolisthesis, in particular at levels L5– S1 and L4–L5. Bypass fixation ensures fixation using the strong structures of the pedicles and laminae so that direct handling occurs without affecting the structures of the slipped vertebra. Spinal alignment is preserved, and normal biomechanical behavior is therefore also restored. Further, this is performed with a relatively low chance of trauma to surrounding tissues and nerves, spinal repositioning problems, or implant failure, which would entail future surgical site operations to recover a postoperative stable spine[
The paper aims to provide anatomical insights and a technical note on single bypass fixation for lumbar spondylolisthesis, demonstrating its efficacy in stabilizing the spine with minimal manipulation of the slipped vertebra.
METHODS
Study participants
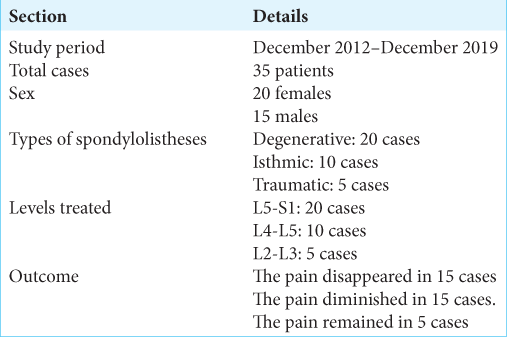
From December 2012 to December 2019, 35 patients with lumbar spondylolisthesis (20 females, 15 males) were treated using the single bypass fixation technique at a neuroscience hospital in Baghdad, Iraq. The patients included 20 cases of degenerative spondylolisthesis, 10 cases of isthmic spondylolisthesis, and five cases of traumatic spondylolisthesis. The affected levels were L5–S1 in 20 cases, L4–L5 in ten cases, and L2–L3 in five cases.
Surgical procedures involved L4–S1 fixation with L5 laminectomy for L5–S1 spondylolisthesis. L3–L5 fixation with L4 laminectomy for L4–L5 spondylolisthesis, and L2-L4 fixation with L3 laminectomy for L2–L3 spondylolisthesis were also performed, with the objective of decompressing the neural elements, reducing vertebral slippage, and stabilizing the affected spinal segments. L1–L5 fixation with L2–L3 laminectomies for cases with both L3 and L4 slipped forward. Postoperative mobilization began on the second postoperative day, with follow-up periods ranging from 12 months to 4.5 years, averaging 3.4 years.
The surgical technique
The one-bypass fixation technique stabilizes the lumbar spine by fixing the vertebrae above and below the affected segment [
Furthermore, pre-contoured rods are placed through the heads of the pedicle screws to stabilize the spine. The rods are secured with locking caps, ensuring a rigid construct. The screws and rods bypass the unstable segment, providing stability without directly manipulating the slipped vertebra. Autograft or allograft bone is placed around the stabilized segment to promote fusion. This may involve placing bone graft material in the interbody space, poster laterally, or both. The incision is then closed in layers, focusing on achieving a watertight closure to prevent postoperative infection.[
RESULTS
Preoperative symptoms included local pain, tenderness, and limited backward extension. Twenty patients experienced radiculopathy, while the remaining did not. Flexion-extension X-rays assessed the degree of vertebral slippage, ranging from 25% to more than 50% [as depicted in
Postoperatively, 15 patients reported complete relief from local pain and tenderness, 15 reported diminished symptoms, and five continued to experience local pain. Radiculopathy resolved in 90% of cases, though 10% of patients continued to experience sensory paresthesia and anesthesia[
Radiological assessments indicated significant improvements in vertebral alignment and stability. The average degree of slippage reduction was substantial, with most patients achieving near-complete realignment of the affected vertebrae.[
The overall fusion rate was high, with most patients showing successful integration of the fixation hardware and bone grafts. The incidence of hardware-related complications was minimal, with only a few cases of minor screw loosening that did not require further surgical intervention. In addition, no major complications, such as infection or significant neurological deficits, were reported, indicating the safety and reliability of the technique.[
The radiographical follow-up of the patients showed excellent fusion rates with maintained alignment and disc height. In general, the functional outcomes, assessed by standard clinical scales, found in a high percentage of patients an improvement in the quality of life. Only 2% of the latter patients had to be further intervened because they continued with symptoms or some complications from the intervention.
DISCUSSION
This technical note highlights the efficacy of the bypass fixation in providing stable and durable relief in patients with lumbar spondylolisthesis. The procedure also does not require much handling of the slipped vertebra, thus lowering the possibility of more trauma and related complications. In fact, the clinical follow-up shows remarkable improvement in pain and neurological symptoms, with high rates of patient satisfaction.[
The results of the study have substantiated the fact that bypass fixation not only eliminates symptoms but also maintains long-term spinal stability. Probably, the most important advantage of the technique is that it can result in minimum postoperative pain and early mobilization. Furthermore, the high rate of fusion and low incidence of complications help in further substantiating the use of the technique as the first preferred line of treatment in lumbar spondylolisthesis. This is further of the usage of the bypass fixation anatomical approach because the procedure saves the integrity of the spinal column without interfering with the surrounding soft tissues and nerve structures and because there is ensured no permanent neurological deficit that could arise with this condition. The patient also attains quick recovery.[
Those patients who have undergone treatment through this technique are reported to have good performance in terms of less blood loss, time in the operation room, and hospital stay without having their fusion and alignment rate affected. However, clinical and radiological long-term follow-up studies of these patients have shown progressive improvement. The technique is of great help per se for such conditions where the conventional method carries higher risk coupled with poor success rates.[
CONCLUSION
Fixation with bypass for lumbar spondylolisthesis is an emerging technique that offers effective stabilization symptom relief and minimizes complications. It exploits the lumbar spine’s strengths, resulting in high fusion rates and low complications. Further research is needed to establish this technique and apply it to all spinal pathologies, making it a useful addition to current surgical treatments.
Ethical approval
The Institutional review board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Aoki Y, Yamagata M, Ikeda Y, Nakajima F, Ohtori S, Nakagawa K. A prospective randomized controlled study comparing transforaminal lumbar interbody fusion techniques for degenerative spondylolisthesis: Unilateral pedicle screw and one cage versus bilateral pedicle screws and two cages. J Neurosurg Spine. 2012. 17: 300-6
2. Dai S, Zhang Z, Li Y, Yang Z, Zhang Y, Wang Q. Treatment of lumbar spondylolisthesis with spondylolisthesis reduction system internal fixation and decompression, posterior alone interbody cage fusion and bone grafting. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2008. 22: 1445-7
3. Guangrong K. Posterior single interbody cage combined with vertebral arch pedicle screw fixation for the treatment of lumbar spondylolisthesis. Lingnan Modern Clin Surg. 2006. 4: 34-8
4. Huilin Y. The basic research and long-term follow-up study of lumbar spondylolysis and isthmic spondylolisthesis treated with direct repair and fixation with single vertebra reduction and fixation system. Chin J Orthop. 2001. 21: 98-103
5. Khalil JG, Fischgrund J, Roberts RV. Surgical management of lumbar spondylolisthesis. Orthop Clin North Am. 2017. 48: 491-501
6. Kim JS, Choi W, Lee SH. Minimally invasive anterior lumbar interbody fusion followed by percutaneous pedicle screw fixation for isthmic spondylolisthesis: Minimum 5-year follow-up. Spine J. 2010. 10: 404-9
7. Lee SH, Choi W, Lim S, Kang HY, Shin SW. Minimally invasive anterior lumbar interbody fusion followed by percutaneous pedicle screw fixation for isthmic spondylolisthesis. Spine J. 2004. 4: 644-9
8. Lin Y, Li F, Chen W, Zeng H, Chen A, Xiong W. Single-level lumbar pyogenic spondylodiscitis treated with mini-open anterior debridement and fusion in combination with posterior percutaneous fixation via a modified anterior lumbar interbody fusion approach. J Neurosurg Spine. 2015. 23: 74-81
9. Qian Z, Tang T, Yang H. The direct repair of the defect and grafting with single segment reduction fixation system in treating lumbar spondylolysis and spondylolisthesis. Zhonghua Wai Ke Za Zhi. 1995. 33: 613-6
10. Shao SZ, Hou HT, Sun XC, Tan YC, Liu H, Fu S. Treatment of lumbar spondylolisthesis by posterior restoration and three-column fixation. Zhongguo Gu Shang. 2008. 21: 177-81
11. Takahashi T, Hanakita J, Watanabe M, Kawaoka T, Takebe N, Kitahara T. Lumbar alignment and clinical outcome after single level asymmetrical transforaminal lumbar interbody fusion for degenerative spondylolisthesis with local coronal imbalance. Neurol Med Chir. 2014. 54: 620-5
12. Walker CT, Farber SH, Gandhi SV, Godzik J, Turner JD, Uribe J. Single-position prone lateral interbody fusion improves segmental lordosis in lumbar spondylolisthesis. World Neurosurg. 2021. 150: e1043-9