- Department of Neurosurgery, Università Politecnica delle Marche, Ancona, Italy.
Correspondence Address:
Riccardo Paracino, Department of Neurosurgery, Università Politecnica delle Marche, Ancona, Italy.
DOI:10.25259/SNI_1148_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Alessandro Di Rienzo1, Riccardo Paracino1, Valentina Liverotti1, Maurizio Gladi1, Mauro Dobran1. Skip hemilaminectomy for the treatment of holospinal epidural abscess: A single-center experience. 30-Dec-2021;12:625
How to cite this URL: Alessandro Di Rienzo1, Riccardo Paracino1, Valentina Liverotti1, Maurizio Gladi1, Mauro Dobran1. Skip hemilaminectomy for the treatment of holospinal epidural abscess: A single-center experience. 30-Dec-2021;12:625. Available from: https://surgicalneurologyint.com/surgicalint-articles/11315/
Abstract
Background: Holospinal epidural abscesses (HEAs) are rare with potentially devastating consequences. Urgent bony decompression and abscess evacuation with long-term antibiotic therapy are typically the treatment of choice.
Methods: We reviewed cases of holospinal HEAs operated on between 2009 and 2018. Variables studied included preoperative laboratories, CT/MR studies plus clinical and radiographic follow-up for between 34 and 60 postoperative months.
Results: We utilized skip hemilaminectomies to minimize the risks of segmental instability. Targeted antibiotic therapy was also started immediately and maintained for 6 postoperative weeks. MR/CT studies documented full radiographic and neurological recovery between 6 and 12-months later.
Conclusion: HEAs may be treated utilizing multilevel skip hemilaminectomies to help maintain spinal stability while offering adequate abscess decompression/resolution.
Keywords: Epidural abscess, Holospinal epidural abscess, Mini-invasive spine surgery, Skip hemilaminectomy
INTRODUCTION
Holospinal epidural abscesses (HEAs) are rare with potentially devastating consequences. They typically occur in the sixth and seventh decades of life.[
MATERIALS AND METHODS
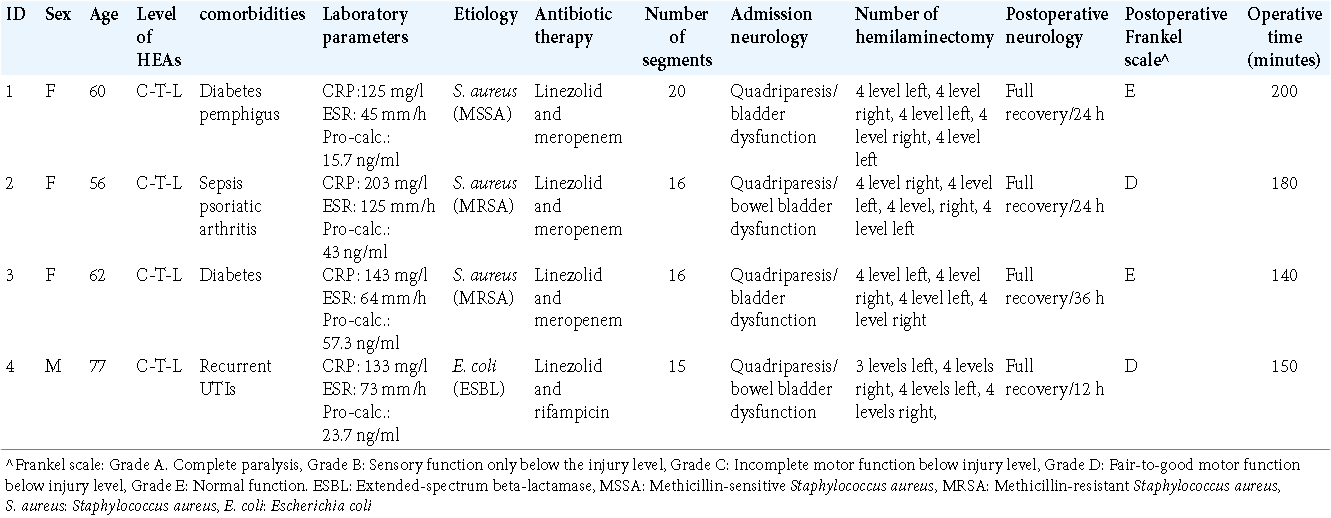
Four patients with HEAs had surgery between 2009 and 2018. The preoperative work-up included neurological evaluation and full laboratory studies (i.e., ESR, CRP, procalcitonin, and MR/CT assessment) [
Surgical technique
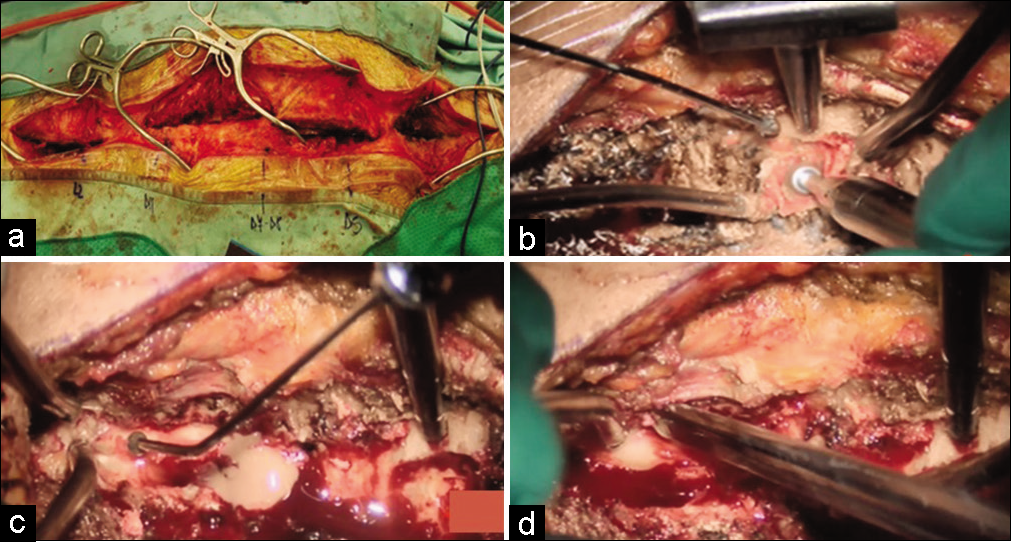
Surgery was performed, on average, within 6 h of admission. Although the incision spanned the entire abscess length, we utilized skip laminectomies to preserve spinal stability, avoiding performing full laminectomies at all levels. Four surgeons simultaneously operated at different levels; two initially started on the cervical region and then continued to the lower cervical/upper thoracic spine, while two other surgeons started on the contralateral side in the mid-lower thoracic region and proceeded to the lower lumbar levels [
Figure 1:
(a and b) Skin was incised along the midline and muscles were dissected subperiosteally and unilaterally. Hemilaminectomy never extended beyond four levels, leaving a residual bony bridge on each side. Care was taken to preserve the inter- and epi-spinous ligaments. (c) Collection removal was obtained by gentle suction of the fluid component and irrigation. (d) Sublaminar undercutting and contralateral flavectomy were added to allow contralateral abscess control.
Clinical data
Three females and one male averaged 62 years of age were included in the study. Their comorbidities consisted of diabetes mellitus (2), pemphigus under steroids treatment (1), recurrent UTIs (1), sepsis (1), and psoriatic arthritis (1) [
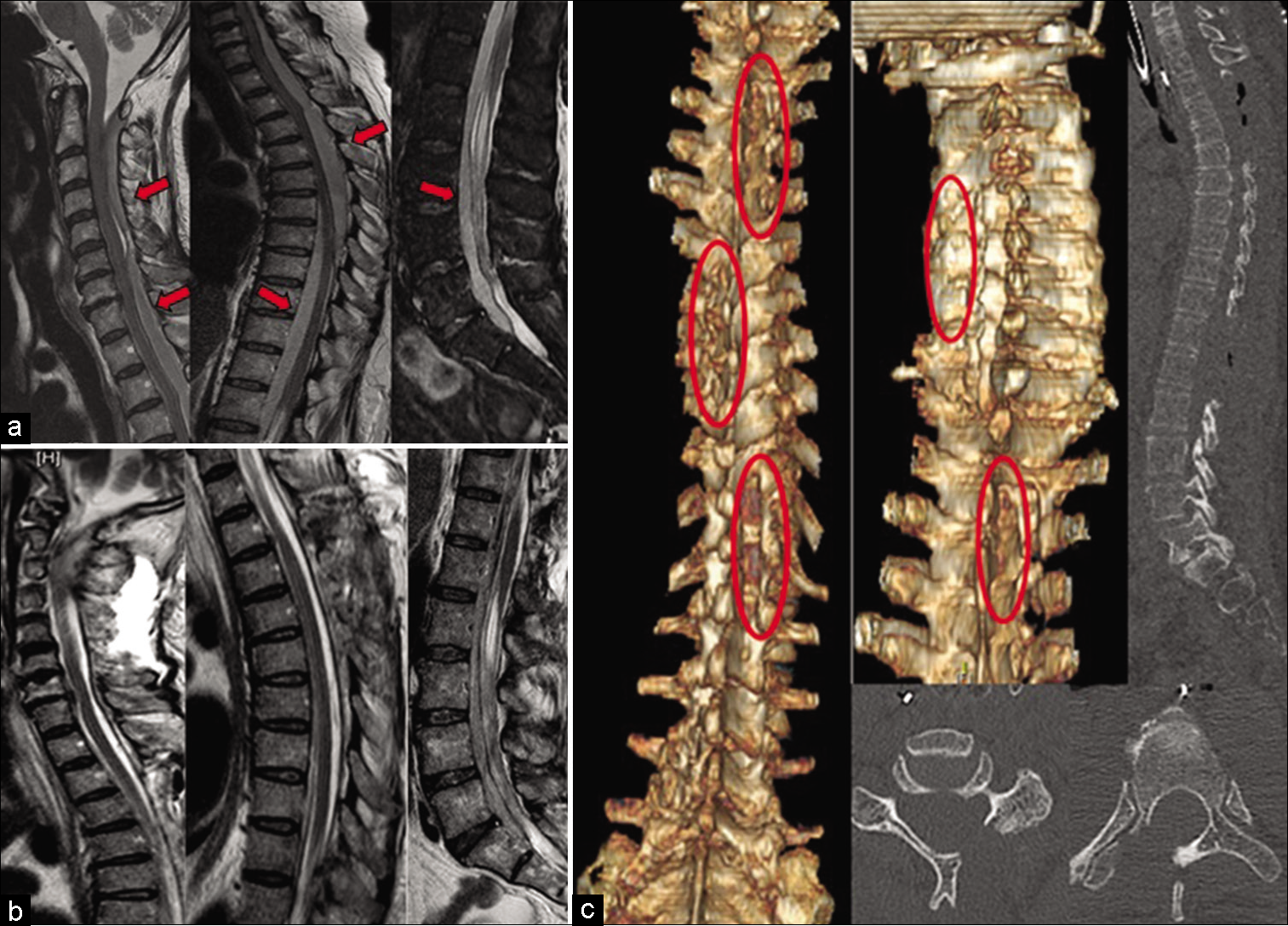
Figure 2:
(a) Contrast MRI T2 study documenting an extensive (C3-S1) purulent epidural collection, with severe cord components both at cervical and lumbar levels (red arrow). (b and c) A postoperative high-resolution computed tomography scan with coronal, sagittal, and 3D reconstructions (skip hemilaminectomy was marked by red circle) and a contrast MRI showed complete evacuation of HEA and spinal stability.
RESULTS
Postoperative course
Following multilevel skip laminectomies, two patients experienced full symptoms regression within 48 h, and two others within 3 and 8 weeks postoperatively. MR imaging performed within 1 week after surgery uniformly confirmed complete evacuation of the collection [
Organisms
Intraoperative cultures revealed methicillin-sensitive Staphylococcus aureus (one patient), extended-spectrum beta-lactamase-positive Escherichia coli (one patient), and methicillin-resistant S. aureus (two patients). Broad-spectrum antibiotics were started immediately after surgery and replaced by targeted therapy in two cases once microbiological sampling was received [
Follow-up and duration of antibiotic therapy
Patients underwent 6–12 months of standing postoperative holospinal X-rays plus an MRI and CT at 12 months, none developed instability [
DISCUSSION
HEAs are relatively rare, and early diagnosis and treatment are critical to achieve the best functional outcomes. Neurological deficits are typically due to direct mechanical compression and/or indirect vascular occlusion (i.e., septic thrombophlebitis).[
Surgical options
Older reports described the use of extensive laminectomies or hemilaminectomies, but increased the risks of instability.[
Skip hemilaminectomy (SH)
SH has the following advantage: preserving the entire spinous processes and posterior spinous ligaments while leaving the facet joints alone. They offer satisfactory exposure with safe removal of HSAs. They also minimize intraoperative blood loss and reduce the risk of spreading the infection to surrounding unaffected structures. Furthermore, as show in this case, they can be performed by two teams of two spine surgeons/team addressing different contralateral levels.[
CONCLUSION
HEAs are rare, and multilevel skip hemilaminectomies provide adequate decompression/abscess resection, while avoiding subsequent instability.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abd-El-Barr MM, Bi WL, Bahluyen B, Rodriguez ST, Groff MW, Chi JH. Extensive spinal epidural abscess treated with “apical laminectomies” and irrigation of the epidural space: Report of 2 cases. J Neurosurg Spine. 2015. 22: 318-23
2. Börm W, Mohr K, Hassepass U, Richter HP, Kast E. Spinal hematoma unrelated to previous surgery: Analysis of 15 consecutive cases treated ina single institution within a 10-year period. Spine. 2004. 29: E555-61
3. Bridges KJ, Than KD. Holospinal epidural abscesses institutional experience. J Clin Neurosci. 2018. 48: 18-27
4. Di Rienzo A, Brunozzi D, Dobran M, Iacoangeli M, Colasanti R, Trivedi R. Skip hemilaminectomy for large, multilevel spinal epidural hematomas: Report of a series of 11 patients. World Neurosurg. 2018. 111: e933-40
5. Dobran M, Mancini F, Paracino R, Lattanzi S, di Somma L, Nasi D. Laminectomy versus open-door laminoplasty for cervical spondylotic myelopathy: A clinical outcome analysis. Surg Neurol Int. 2002. 11: 73
6. Killen MC, Hernandez M, Berg A, Bhatia C. Nonoperative management of a multi-regional epidural abscess with neurological dysfunction. Int J Spine Surg. 2015. 9: 47
7. Nussbaum ES, Rigamonti D, Standiford H, Numaguchi Y, Wolf AL, Robinson WL. Spinal epidural abscess: A report of 40 cases and review. Surg Neurol. 1998. 38: 225-31
8. Proietti L, Ricciardi L, Noia G, Barone G, Valenzi E, Perna A. Extensive spinal epidural abscesses resolved with minimally invasive surgery: Two case reports and review of the recent literature. Acta Neurochir Suppl. 2019. 125: 345-53
9. Siasios ID, Fotiadou A, Fountas K, Dimopoulos V. Holospinal epidural abscess in elderly patient: A case presentation and review. Surg Neurol Int. 2019. 10: 204
10. Smith GA, Kochar AS, Manjila S, Onwuzulike K, Geertman RT, Anderson JS. Holospinal epidural abscess of the spinal axis: Two illustrative cases with review of treatment strategies and surgical techniques. Neurosurg Focus. 2014. 37: E11