- Department of Radiology, Aga Khan University, Karachi, Pakistan
- Department of Pathology and Laboratory Medicine, Aga Khan University Hospital, Karachi, Pakistan.
Correspondence Address:
Kumail Khandwala, Department of Radiology, Aga Khan University, Karachi, Pakistan.
DOI:10.25259/SNI_166_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Raima Zakaria1, Fatima Mubarak1, Kumail Khandwala1, Aisha Memon2. Skull base metastasis as initial presentation of hepatocellular carcinoma. 25-Aug-2023;14:297
How to cite this URL: Raima Zakaria1, Fatima Mubarak1, Kumail Khandwala1, Aisha Memon2. Skull base metastasis as initial presentation of hepatocellular carcinoma. 25-Aug-2023;14:297. Available from: https://surgicalneurologyint.com/surgicalint-articles/12516/
Abstract
Background: Intracranial metastatic deposits due to hepatocellular carcinoma (HCC) are rare. Only a few cases are reported in the literature. These may be more likely to come to clinical attention than extrahepatic metastases in other sites since they often produce symptoms that necessitate neurosurgical intervention.
Case Description: We report a case of a 53-year-old male with biopsy-proven intracranial skull base metastasis from HCC as an unusual initial presentation of the disease and review the relevant literature on this entity.
Conclusion: Intracranial metastasis of HCC should be included in the differential diagnosis of rapidly growing metastatic lesions in unusual locations, particularly in chronic liver disease and hepatitis B surface antigen-positive or hepatitis C patients.
Keywords: Brain, Hepatocellular carcinoma, Intracranial, Metastasis, Neuroradiology
INTRODUCTION
Hepatocellular carcinoma (HCC) is the third leading cause of cancer mortality. The highest incidence rates are reported in Southeast Asia and sub-Saharan Africa due to prevalent hepatitis B and C infections in these regions.[
Extrahepatic metastases of HCC are commonly seen in the lungs, lymph nodes, bone marrow, and adrenals.[
CASE PRESENTATION
A 53-year-old diabetic male presented with complaints of right-sided hearing loss for the past 4 days. The patient also had an abrupt onset of numbness, weakness, and tingling sensations on the right side of the face and developed a loss of taste sensation. The patient’s medical history was remarkable for chronic hepatitis C infection and was treated for it.
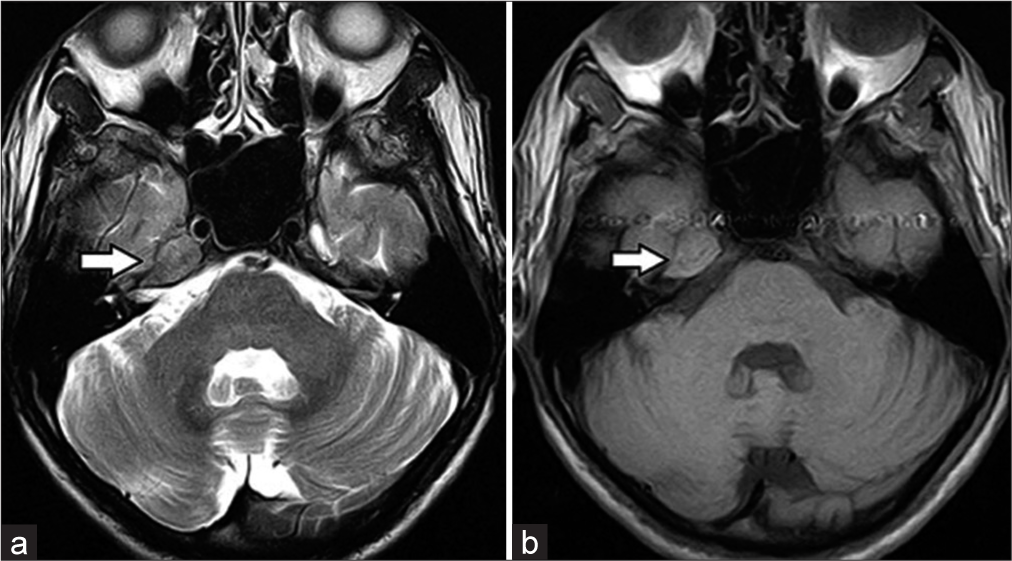
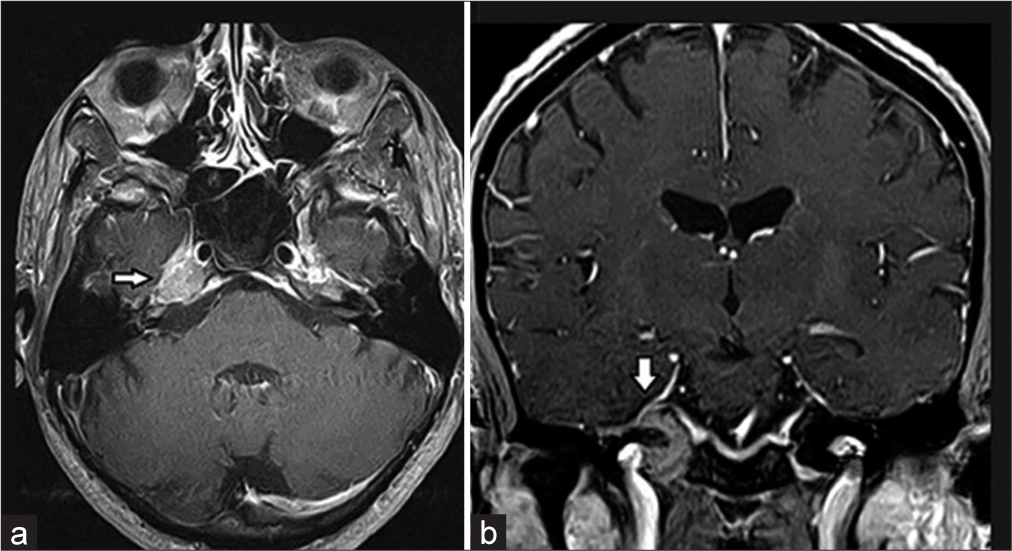
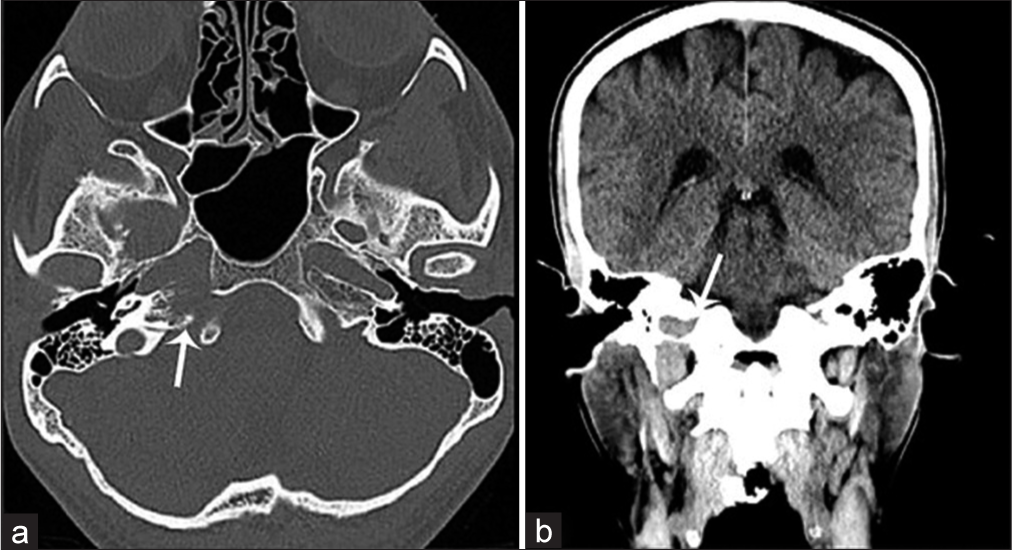
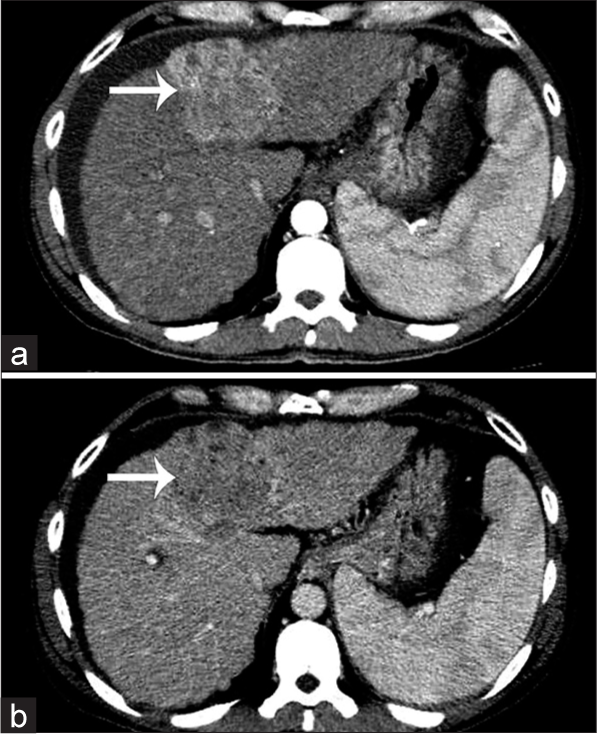
Magnetic resonance imaging of the brain and computed tomography (CT) scans revealed an extra-axial lesion involving the right petrous apex, the clivus, extending along the Meckel’s cave, indenting the temporal lobe [
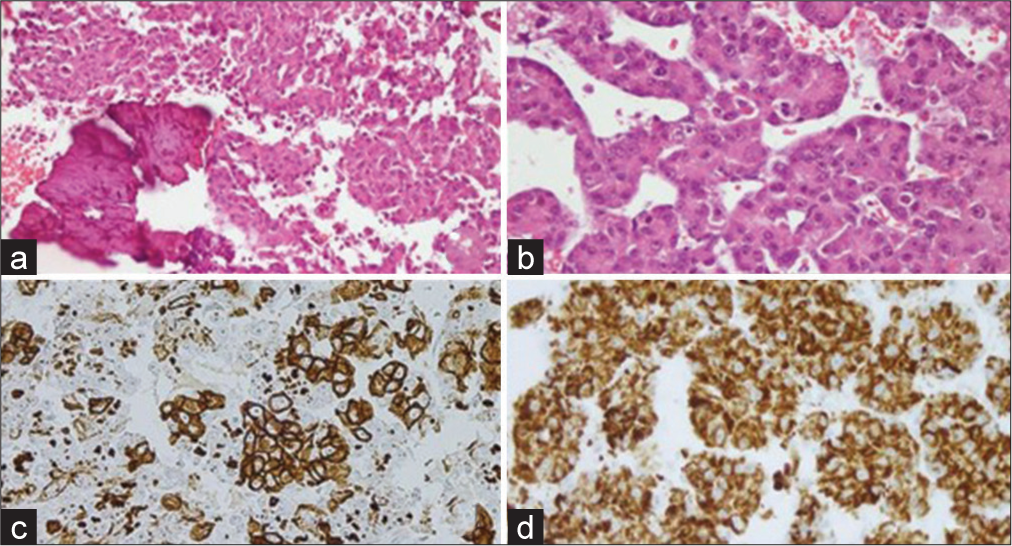
A right temporal craniotomy and biopsy was performed. Intraoperatively, the lesion was firmly attached along the petrous temporal bone. Histology sections examined revealed features of metastatic carcinoma, likely of primary hepatocellular origin [
Figure 4:
Histological slides (a) (H&E stain ×40): Bony tissue infiltrated by metastatic carcinoma. (b) (H&E ×40): Tumor cells with moderate eosinophilic cytoplasm, pleomorphic nuclei, prominent nucleoli, and trabecular pattern of growth. (c and d) Positive immunostaining for cytokeratin AE1/AE3 and HepPar1 in tumor cells.
DISCUSSION
Extrahepatic metastases of HCC are common; however, intracranial metastasis is the rarest form of presentation. Only a few sporadic clinical cases of intracranial metastasis from HCC have been reported in the literature [
CONCLUSION
Metastasis of HCC should be included in the differential diagnosis of rapidly growing lesions in unusual locations, particularly in chronic liver disease and hepatitis B surface antigen-positive or hepatitis C patients, even if a primary tumor cannot be radiologically identified.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Asahara T, Yano M, Fukuda S, Fukuda T, Nakahara H, Katayama K. Brain metastasis from hepatocellular carcinoma after radical hepatectomy. Hiroshima J Med Sci. 1999. 48: 91-4
2. Chang L, Chen YL, Kao MC. Intracranial metastasis of hepatocellular carcinoma: Review of 45 cases. Surg Neurol. 2004. 62: 172-7
3. Endo M, Hamano M, Watanabe K, Wakai S. Combined chronic subdural and acute epidural hematoma secondary to metastatic hepatocellular cancer: Case report. No Shinkei Geka. 1999. 27: 331-4
4. El-Serag HB. Hepatocellular carcinoma: An epidemiologic view. J Clin Gastroenterol. 2002. 35: S72-8
5. Friedman HD. Hepatocellular carcinoma with central nervous system metastasis: A case report and literature review. Med Pediatr Oncol. 1991. 19: 139-44
6. Han MS, Moon KS, Lee KH, Cho SB, Lim SH, Jang WY. Brain metastasis from hepatocellular carcinoma: The role of surgery as a prognostic factor. BMC Cancer. 2013. 13: 567
7. Jessica M, Caterina F, Alessandro F, Gianpiero F, Giuseppe A. Brain metastases from gastrointestinal tumours: Tailoring the approach to maximize the outcome. Crit Rev Oncol Hematol. 2013. 85: 32-44
8. Katyal S, Oliver JH, Peterson MS, Ferris JV, Carr BS, Baron RL. Extrahepatic metastases of hepatocellular carcinoma. Radiology. 2000. 216: 698-703
9. Kim M, Na DL, Park SH, Jeon BS, Roh JK. Nervous system involvement by metastatic hepatocellular carcinoma. J Neurooncol. 1998. 36: 85-90
10. Loo KT, Tsui WM, Chung KH, Ho LC, Tang SK, Tse CH. Hepatocellular carcinoma metastasizing to the brain and orbit: Report of three cases. Pathology. 1994. 26: 119-22
11. Moriya H, Ohtani Y, Tsukui M, Tanaka Y, Tajima T, Makuuchi H. A case report: tumorectomy for brain metastasis of hepatocellular carcinoma. Tokai J Exp Clin Med. 1999. 24: 105-10
12. Peres MF, Forones NM, Malheiros SM, Ferraz HB, Stávale JN, Gabbai AA. Hemorrhagic cerebral metastasis as a first manifestation of a hepatocellular carcinoma. Case report. Arq Neuropsiquiatr. 1998. 56: 658-60
13. Salvati M, Cimatti M, Frati A, Santoro A, Gagliardi FM. Brain metastases from hepatocellular carcinoma. A case report. J Neurosurg Sci. 2002. 46: 77-80
14. Shuangshoti S, Rungruxsirivorn S, Panyathanya R. Intracranial metastasis of hepatic carcinomas: A study of 9 cases within 28 years. J Med Assoc Thai. 1989. 72: 307-13
15. Tanabe H, Kondo A, Kinuta Y, Matsuura N, Hasegawa K, Chin M. Unusual presentation of brain metastasis from hepatocellular carcinoma--two case reports. Neurol Med Chir (Tokyo). 1994. 34: 748-53
16. Tunc B, Filik L, Tezer-Filik I, Sahin B. Brain metastasis of hepatocellular carcinoma: A case report and review of the literature. World J Gastroenterol. 2004. 10: 1688-9
17. Wang S, Wang A, Lin J, Xie Y, Wu L, Huang H. Brain metastases from hepatocellular carcinoma: Recent advances and future avenues. Oncotarget. 2017. 8: 25814-29
18. Yen FS, Wu JC, Lai CR, Sheng WY, Kuo BI, Chen TZ. Clinical and radiological pictures of hepatocellular carcinoma with intracranial metastasis. J Gastroenterol Hepatol. 1995. 10: 413-8