- Department of Anesthesiology, Advocate Illinois Masonic Medical Center, Chicago, United States
- Ghaly Neurosurgical Associates, Aurora, Illinois, United States.
- Department of Anesthesiology, University of Illinois, Chicago, United States
Correspondence Address:
Ramsis F. Ghaly
Department of Anesthesiology, Advocate Illinois Masonic Medical Center, Chicago, United States
Department of Anesthesiology, University of Illinois, Chicago, United States
DOI:10.25259/SNI_58_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ramsis F. Ghaly, Ana Plesca, Kenneth D. Candido, Nebojsa Nick Knezevic. SNI case of the week: Initial concomitant use of gabapentin, clonidine, and prednisone may enhance suicidal ideation: A case report. 06-Mar-2020;11:41
How to cite this URL: Ramsis F. Ghaly, Ana Plesca, Kenneth D. Candido, Nebojsa Nick Knezevic. SNI case of the week: Initial concomitant use of gabapentin, clonidine, and prednisone may enhance suicidal ideation: A case report. 06-Mar-2020;11:41. Available from: https://surgicalneurologyint.com/surgicalint-articles/9889/
Abstract
Background: Suicide cases are the end product of a combination of biological, clinical, psychological, social, and cultural risk/protective factors, and attempts to remain unpredictable.
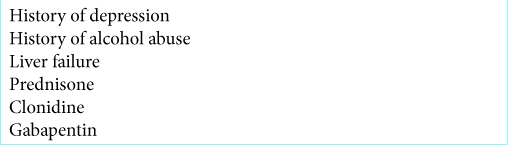
Case Description: A 43-year-old male presented to the hospital with jaundiced skin/eyes of 7 days’ duration. He had a history of a major depressive disorder and chronic alcohol consumption (e.g., 3–5 alcoholic drinks/day for the past 15 years). Studies documented acute hepatic disease (e.g., biopsy-documented hepatocellular alcoholic hepatitis), accompanied by a cholestatic disease. The patient was discharged on clonidine, iron multivitamin, folic acid, gabapentin, and prednisone. Eight days postdischarge from the hospital, he committed suicide (e.g., self- inflicted gunshot wound to the head).
Conclusion: Concomitant administration of gabapentin, prednisone, and clonidine, especially if used for the first time, may play a synergistic effect in increasing a patient’s suicide risk.
Keywords: Alcohol withdrawal syndrome, Clonidine, Gabapentin, Glucocorticoids, Suicide risk
INTRODUCTION
The World Health Organization states that suicide is a global phenomenon, with close to 800,000 people dying from suicide every year.[
The pathways to suicide are complex, with suicide being the outcome of a combination of biological, clinical, psychological, social, cultural risk, and protective factors. Therefore, despite the presence of risk factors, or lack thereof, the suicide cases are often unpredictable.
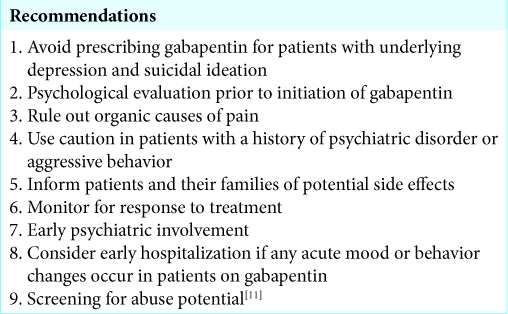
In this case report, we are coming back to the issue of prescribing gabapentin off label, this time being for alcohol withdrawal syndrome (AWS). This is also the first case report discussing a potential synergistic effect of concomitant use of gabapentin, prednisone, and clonidine leading to suicidal ideation, especially if these medications are used for the first time.
One could argue that any of the aforementioned medications could possibly aggravate the suicidal ideation considering the complex medical history of the patient; nevertheless, they should be considered as risk factors.
CASE REPORT
Clinical history
A 43-year-old male presented to the emergency room with the chief complaint of jaundiced skin and eyes, for 7 days. Vital signs were within normal limits except for a heart rate of 98 beats/min and high blood pressure of 166/98 mmHg; pain score was 0. At the time of admission, he had not taken any medications. During admission, he stated that he was feeling fatigued and noticed a slight distention of his abdomen. He had been using alcohol on a regular basis, and homeopathic pills 3 times per week; he was unable to recall the name and content of pills.
Medical history was significant for obesity: body mass index 43.54 kg/m2, hyperlipidemia, and prediabetes. In addition, he was suffering from prolonged major depressive disorder and alcohol abuse problems. He admitted to consuming 3–5 alcoholic drinks per day for the past 15 years. Over the course of several years, he was treated with psychotherapy, electroconvulsive therapy, and venlafaxine 37.5 mg, one capsule daily, with only temporary relief. The patient had a history of soliciting help for his alcohol use disorder from AA group meetings.
Five years ago, he was admitted to the emergency department complaining of a self-inflicted stab wound to the right thigh. He denied any suicidal thoughts and/or past thoughts of self- harm and reports that he impulsively stabbed his thigh while playing with a knife in his car. Laboratory workup was within normal limits, except for ethanol blood level of 214 mg/dL.
During the current encounter, ultrasound investigation revealed no bile duct dilation, no gallstones, gallbladder with wall thickening, enlarged liver without focal mass, and likely thrombosed portal vein. Although the liver injury presented as a cholestatic picture, considering the significant direct hyperbilirubinemia possibly from portal vein thrombosis, he also had a hepatocellular pattern of liver dysfunction typical for alcoholic hepatitis due to >2:1 aspartate aminotransferase/alanine transaminase elevation. Other differential diagnoses were drug- induced: the use of unclear homeopathic supplements, and nonalcoholic steatohepatitis due to severe obesity. Deranged synthetic liver function as evidenced by thrombocytopenia and mild coagulopathy suggestive of hepatic insufficiency, likely due to acute alcoholic hepatitis. During the hospitalization, the patient showed signs of mild alcohol withdrawal with tremor, tachycardia (119 beats/min), and high blood pressure. The symptoms were managed by administering lorazepam 1 mg, once. Clonidine and gabapentin for ethanol withdrawal were also started, which helped in symptom resolution. The patient was also started on prednisone, per gastroenterologist indication. The recommendations at discharge were strict alcohol cessation, no acetaminophen intake, and hepatitis A and B vaccine when the patient was stable, outpatient gastrointestinal (GI) follow-up, liver function tests, and international normalized ratio follow-up, monitoring for alcohol withdrawal, and psychiatry referral. The medication list at discharge was as follows:
Clonidine 0.1 mg/24 h; he had two patches in place, one was supposed to be removed in 3 days and then removal of the last remaining patch on the 4th day Multivitamin – iron one tablet by mouth daily Folic acid – 1 mg tablet take one by mouth daily Gabapentin 300 mg: take one capsule by mouth 3 times a day, then one capsule by mouth twice a day, then two capsules by mouth daily at bedtime and discontinue Prednisone 20 mg: take 3 tablets orally every morning for 28 days, then taper off per instructions by GI doctor.
History of the incident
Eight days later, the patient was brought by the ambulance to the emergency room with a gunshot wound to the head. The event occurred approximately 40 min before presentation, and resuscitation efforts continued. The patient was transferred to a trauma gurney, and cervical neck spinal precautions were maintained. Manual blood pressure was not obtained due to continuous, uninterrupted chest compressions. Prehospital vital signs were: Glasgow coma scale 3, PEA 20s than 70s in the field. The patient shot himself 1 time with a large caliber hand gun. Cardiopulmonary resuscitation has been ongoing for approximately 38 min per emergency medical services. The patient had received a total of 5 mg epinephrine and total resuscitation time 40 min. Cardiac monitoring leads and pulse oximeter were placed. FAST exam showed cardiac standstill. The patient’s spouse stated that the patient had been dealing with health issues and mental health issues for quite some time. However, the spouse expressed shock and surprise as she did not think he was capable of self- harm [
DISCUSSION
Gabapentin and AWS
After reviewing the previous case report published regarding the dangerous side effects of gabapentin,[
Gabapentin use in AWS stems from the convulsive and anxiety-relieving benefits that were reported in preclinical studies. Rebound insomnia, anxiety, and cravings often accompany the discontinuation of benzodiazepines and following the acute management of AWS, leading to an increased risk of relapse. Gabapentin is believed to provide a unique bridge therapy from AWS through early sobriety, to sustained alcohol remission. Gabapentin has also been shown to reduce withdrawal excitability in hippocampal slices.[
In a study conducted by Malcolm et al., lorazepam and gabapentin were compared in the treatment of AWS. It was found that gabapentin effectively diminished the symptoms of alcohol withdrawal, the most effective dose being 1200mg, and reduced the probability of drinking during withdrawal and in the immediate weeks following postwithdrawal.[
In his study, Bonnet et al. concluded that the initial dose of oral gabapentin 800 mg followed by 600 mg QID for 2 days – loaded up to a total of 3200 mg was helpful only in reducing less severe and less complicated acute AWS. The benefits occur in a dose-dependent manner.[
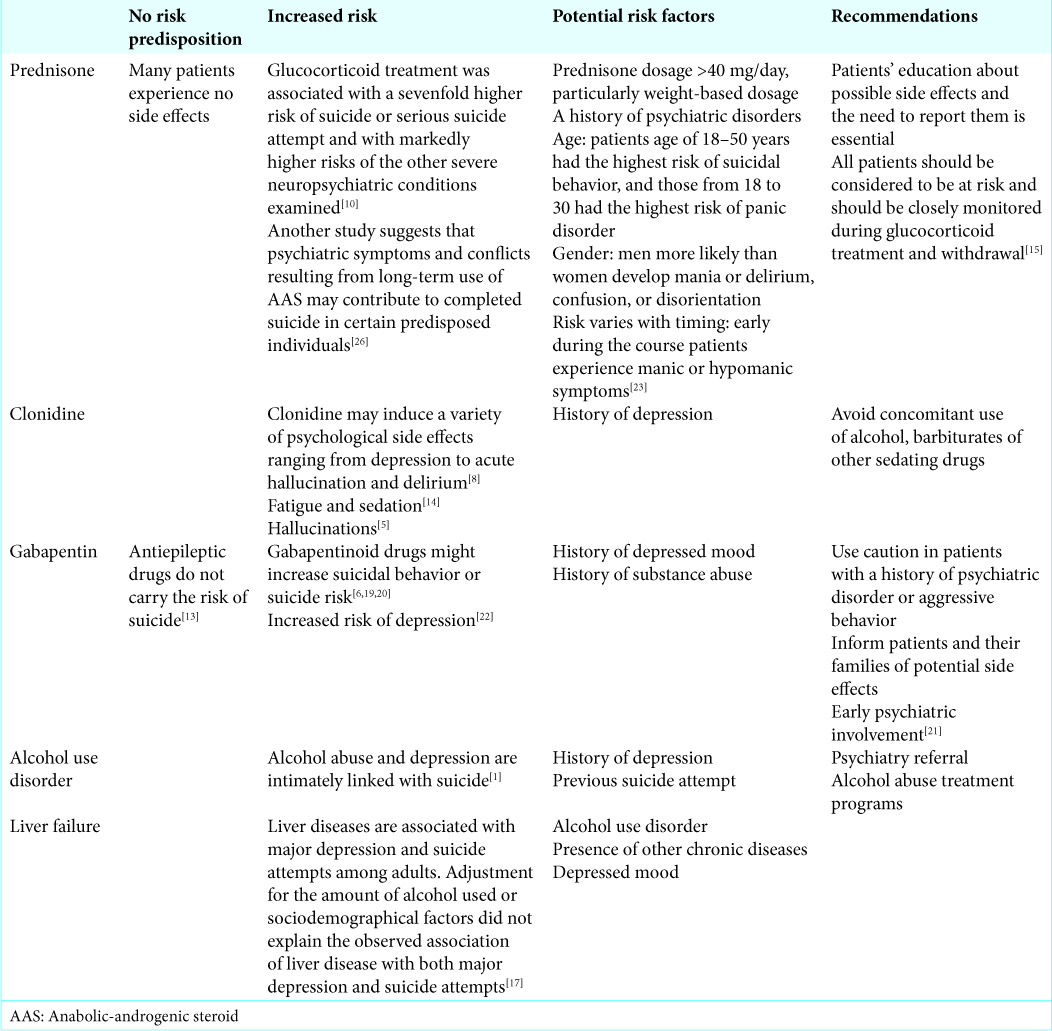
A study conducted in Sweden on 191,973 people that had been prescribed pregabalin or gabapentin in the 2006–2013 interval found that, compared to people that were not taking a gabapentinoid drug, their risk was 26% higher for suicidal behavior or suicide and 24% higher for accidental overdose.[
The side effect of depression and the associated suicidal ideation that accompanies anti-epileptic drugs have been attributed to a GABAergic-mediated decrease in serotonin secretion at the raphe nuclei.[
Glucocorticoid side effects
Glucocorticoids are the most commonly prescribed anti-inflammatory/ immunosuppressant medication worldwide.
In a study performed on 372,696 patients who were prescribed glucocorticoids, it was found that the incidence of suicide, suicide attempt, or severe neuropsychiatric disorders was 22.2/100 person-years at risk for first-course treatments. The hazard ratio for suicide or suicide attempt in exposed patients was 6.89 (95% confidence interval [CI] = 4.52–10.50), compared to people with the same underlying medical disease who were not treated with glucocorticoids, and 1.83 (95% CI = 1.72–1.94) for depression.[
Risks associated with clonidine
Alcohol withdrawal symptoms are extremely variable, but certain symptoms such as tachycardia, hypertension, and tremor may well be interpreted as reflective sympathetic nervous system hyperactivity, for which clonidine is considered a reasonable symptomatic treatment option.
The alpha 2-adrenoreceptor agonist clonidine may induce a variety of psychological side effects ranging from depression to acute hallucination and delirium.[
There is a case reported of a 54-year-old man who developed acute hallucinosis while being treated for hypertension with clonidine. The symptoms developed on two separate occasions, and they subsided after discontinuation of the drug.[
Currently, there are no clearly identifiable risk factors for the development of severe psychological side effects, including dose of medication, duration of treatment, or predisposing mental illness.
Alcohol and suicide risk
Alcohol use and suicide are intimately linked, but they are both complex phenomena, originating from several factors, to depression being considered a common significant risk factor.
Depression and/or alcoholism were comorbid in 85% of 100 cases of completed suicide. The risk of a suicide attempt was found to be increased with increasing psychiatric morbidity: subjects with two or more disorders had odds of serious suicide attempts that were 89.7 times higher than the odds of those with no psychiatric disorder.[
Throughout the course of his illness, the patient admitted to depressed mood on many occasions, but always denied any suicidal ideation. The absence of suicidal ideation, however, does not exclude the risk of suicide, and researchers believe that depression, hopelessness, most mental disorders, and even impulsivity predict ideation, but these factors struggle to distinguish those who have attempted suicide from those who have only considered suicide [
CONCLUSION
The additive effect of gabapentin and clonidine in causing depression may be due to their common effect on reducing the secretion of the stimulating hormones in the central nervous system: dopamine, serotonin, and norepinephrine. It is thought that antiepileptic drugs lead to disinhibition and impulsiveness, which can subsequently influence and promote suicidal acts instead of having a direct effect on behavior. Regarding glucocorticoid administration, preclinical studies showed that elevated levels are associated with functional impairments in the depressed brain, especially in the hippocampus, where it results in reduced neurogenesis and impaired neuroplasticity [
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Beautrais AL, Joyce PR, Mulder RT, Fergusson DM, Deavoll BJ, Nightingale SK. Prevalence and comorbidity of mental disorders in persons making serious suicide attempts: A case-control study. Am J Psychiatry. 1996. 153: 1009-14
2. Bertolote JM, Fleischmann A. Suicidal behavior prevention: WHO perspectives on research. Am J Med Genet C Semin Med Genet. 2005. 133C: 8-12
3. Bonnet U, Hamzavi-Abedi R, Specka M, Wiltfang J, Lieb B, Scherbaum N. An open trial of gabapentin in acute alcohol withdrawal using an oral loading protocol. Alcohol Alcohol. 2010. 45: 143-5
4. Brown MJ, Salmon D, Rendell M. Clonidine hallucinations. Ann Intern Med. 1980. 93: 456-7
5. Campanella C, Salvini S, Casaldi S, Chiacchiararelli F, Serra A, Di Giacomo G. Clonidine hallucinations: Description of a clinical case. Clin Ter. 2000. 151: 45-7
6. Cantrell FL, Mena O, Gary RD, McIntyre IM. An acute gabapentin fatality: A case report with postmortem concentrations. Int J Legal Med. 2015. 129: 771-5
7. Clemens KJ, Vendruscolo LF. Anxious to drink: Gabapentin normalizes GABAergic transmission in the central amygdala and reduces symptoms of ethanol dependence. J Neurosci. 2008. 28: 9087-9
8. Delaney J, Spevack D, Doddamani S, Ostfeld R. Clonidine-induced delirium. Int J Cardiol. 2006. 113: 276-8
9. Enoch MD, Hammad GE. Acute hallucinosis due to clonidine. Curr Med Res Opin. 1977. 4: 670-1
10. Fardet L, Petersen I, Nazareth I. Suicidal behavior and severe neuropsychiatric disorders following glucocorticoid therapy in primary care. Am J Psychiatry. 2012. 169: 491-7
11. Ghaly RF, Plesca A, Rana S, Candido KD, Knezevic NN. Gabapentin-related suicide: Myth or fact?. Surg Neurol Int. 2018. 9: 210-
12. Gomes T, Juurlink DN, Antoniou T, Mamdani MM, Paterson JM, van den Brink W. Gabapentin, opioids, and the risk of opioid-related death: A population-based nested case-control study. PLoS Med. 2017. 14: e1002396-
13. Hesdorffer DC, Berg AT, Kanner AM. An update on antiepileptic drugs and suicide: Are there definitive answers yet?. Epilepsy Curr. 2010. 10: 137-45
14. Huffman JC, Stern TA. Neuropsychiatric consequences of cardiovascular medications. Dialogues Clin Neurosci. 2007. 9: 29-45
15. Judd LL, Schettler PJ, Brown ES, Wolkowitz OM, Sternberg EM, Bender BG. Adverse consequences of glucocorticoid medication: Psychological, cognitive, and behavioral effects. Am J Psychiatry. 2014. 171: 1045-51
16. Klonsky ED, May AM, Saffer BY. Suicide, suicide attempts, and suicidal ideation. Annu Rev Clin Psychol. 2016. 12: 307-30
17. Le Strat Y, Le Foll B, Dubertret C. Major depression and suicide attempts in patients with liver disease in the United States. Liver Int. 2015. 35: 1910-6
18. Leung JG, Hall-Flavin D, Nelson S, Schmidt KA, Schak KM. The role of gabapentin in the management of alcohol withdrawal and dependence. Ann Pharmacother. 2015. 49: 897-906
19. Middleton O. Suicide by gabapentin overdose. J Forensic Sci. 2011. 56: 1373-5
20. Molero Y, Larsson H, D’Onofrio BM, Sharp DJ, Fazel S. Associations between gabapentinoids and suicidal behaviour, unintentional overdoses, injuries, road traffic incidents, and violent crime: Population based cohort study in Sweden. BMJ. 2019. 365: l2147-
21. Myrick H, Malcolm R, Randall PK, Boyle E, Anton RF, Becker HC. A double-blind trial of gabapentin versus lorazepam in the treatment of alcohol withdrawal. Alcohol Clin Exp Res. 2009. 33: 1582-8
22. Petty F. GABA and mood disorders: A brief review and hypothesis. J Affect Disord. 1995. 34: 275-81
23. Ricoux A, Guitteny-Collas M, Sauvaget A, Delvot P, Pottier P, Hamidou M. Oral glucocorticoid-induced psychiatric side-effects: Focus on clinical specificities, incidence, risk factors and treatment. Rev Med Interne. 2013. 34: 293-302
24. . https://www.who.int/mental_health/prevention/suicide/suicideprevent/en [Last accessed on 2019 Aug 12].
25. . https://www.afsp.org/about-suicide/suicide-statistics [Last accessed on 2019 August 12].
26. Thiblin I, Runeson B, Rajs J. Anabolic androgenic steroids and suicide. Ann Clin Psychiatry. 1999. 11: 223-31