- Department of Neurosurgery, Post-graduate Institute of Medical Education and Research, Chandigarh, India
- Department of Pathology, Post-graduate Institute of Medical Education and Research, Chandigarh, India
- Department of Radiology, Post-graduate Institute of Medical Education and Research, Chandigarh, India
Correspondence Address:
Amey R. Savardekar
Department of Neurosurgery, Post-graduate Institute of Medical Education and Research, Chandigarh, India
DOI:10.4103/2152-7806.156570
Copyright: © 2015 Savardekar AR. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Savardekar AR, Patra D, Chatterjee D, Ahuja CK, Salunke P. Solid variant of aneurysmal bone cyst presenting as a giant cervical mass: A clinical, radiological, histopathological dilemma. Surg Neurol Int 07-May-2015;6:
How to cite this URL: Savardekar AR, Patra D, Chatterjee D, Ahuja CK, Salunke P. Solid variant of aneurysmal bone cyst presenting as a giant cervical mass: A clinical, radiological, histopathological dilemma. Surg Neurol Int 07-May-2015;6:. Available from: http://surgicalneurologyint.com/surgicalint_articles/solid-variant-aneurysmal-bone-cyst-presenting-giant/
Abstract
Background:Typical aneurysmal bone cysts (ABCs) are osteolytic, multicystic lesions with parietal sclerosis and blood-filled cysts. In rare instances, the cystic components may be completely absent. Such solid variants in ABC (s-ABC) exhibit a solid architecture; making the clinical, radiological, and histological differentiation from other solid bone tumors like osteosarcoma (especially giant cell rich osteosarcoma) and giant cell tumor, a difficult task.
Case Report:We report the case of a 45–year-old male presenting with a giant solid cervical spine lesion. Histopathology revealed solid variant of ABC, even though the radiological and fine needle aspiration cytology studies pointed toward a giant cell tumor.
Conclusion:We aim to discuss the clinical, radiological, and histological findings of solid ABC (a rare benign entity) vis-à-vis the common neoplastic entities of osteosarcoma and giant cell tumor. The histopathological nuisances in making the diagnosis of s-ABC are put forth, along with its impact on management of such giant bony spinal lesions.
Keywords: Bony tumors of the cervical spine, pathology of solid variant of aneurysmal bone cyst, solid variant of aneurysmal bone cyst, spinal aneurysmal bone cysts
INTRODUCTION
The conventional aneurysmal bone cyst (ABC) is a nonneoplastic bony lesion, characterized by cavernous spaces with fibrous walls, intermixed with bone and giant cells.[
CASE REPORT
Clinical presentation
A 45-year-old male presented with a gradually progressive, painless, firm, lobulated swelling over the left side of neck, of one year duration; without any radiculopathy or myelopathy.
Investigations
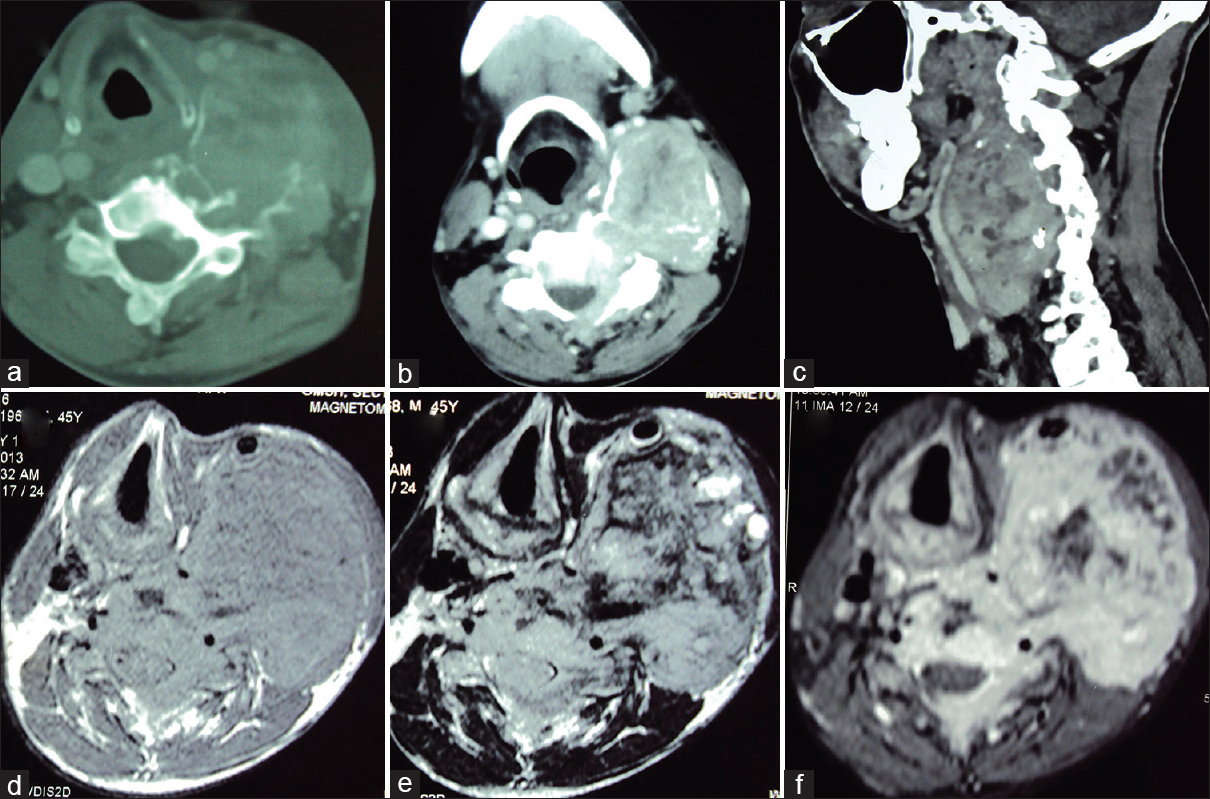
Computed tomography (CT) of neck showed a large expansile lytic lesion with epicentre in the left pedicle and body of C4 vertebrae, extending into the lamina and spinous process [Figure
Figure 1
Computed tomography axial bone window (a) and soft-tissue mediastinal window (b) sections show an expansile, osteolytic lesion arising from the left lateral arch elements of C4 vertebra having an enhancing soft tissue component. The cranio-caudal extent and displacement of vascular and soft tissue structures is appreciated on sagittal CT reconstruction (c) image. Axial T1-weighted precontrast (d), T2-weighted (e) and T1-weighted postcontrast (f) images better demonstrate the extent of the soft tissue component
Treatment
Through anterolateral approach, C4-C5 corpectomy and radical excision of the tumor along with excision of left side pedicle of C4 and C5 was performed by the senior author (PS). Grossly, tumor was solid, fibrous, and highly vascular. Spine was stabilized with C3 to C6 anterior cervical plating with interposed iliac bone graft. Postoperatively, the patient developed transient hoarseness of voice, which resolved over time.
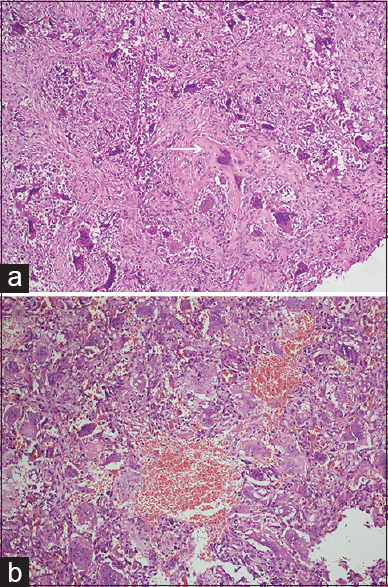
Histopathology
Histology revealed marked fibroblastic proliferation and scattered giant cells, with presence of focal osteoid production, which was not associated with malignant cells [
Figure 2
(a) Photomicrograph showing scattered multinucleated osteoclastic giant cells and focal osteoid production (arrow) in a background of fibroblastic proliferation (H and E ×10). (b) A few dilated blood filled spaces are seen lined by multinucleated osteoclastic giant cells (H and E ×10). The absence of atypia is key to diagnosis of s-ABC
Follow-up
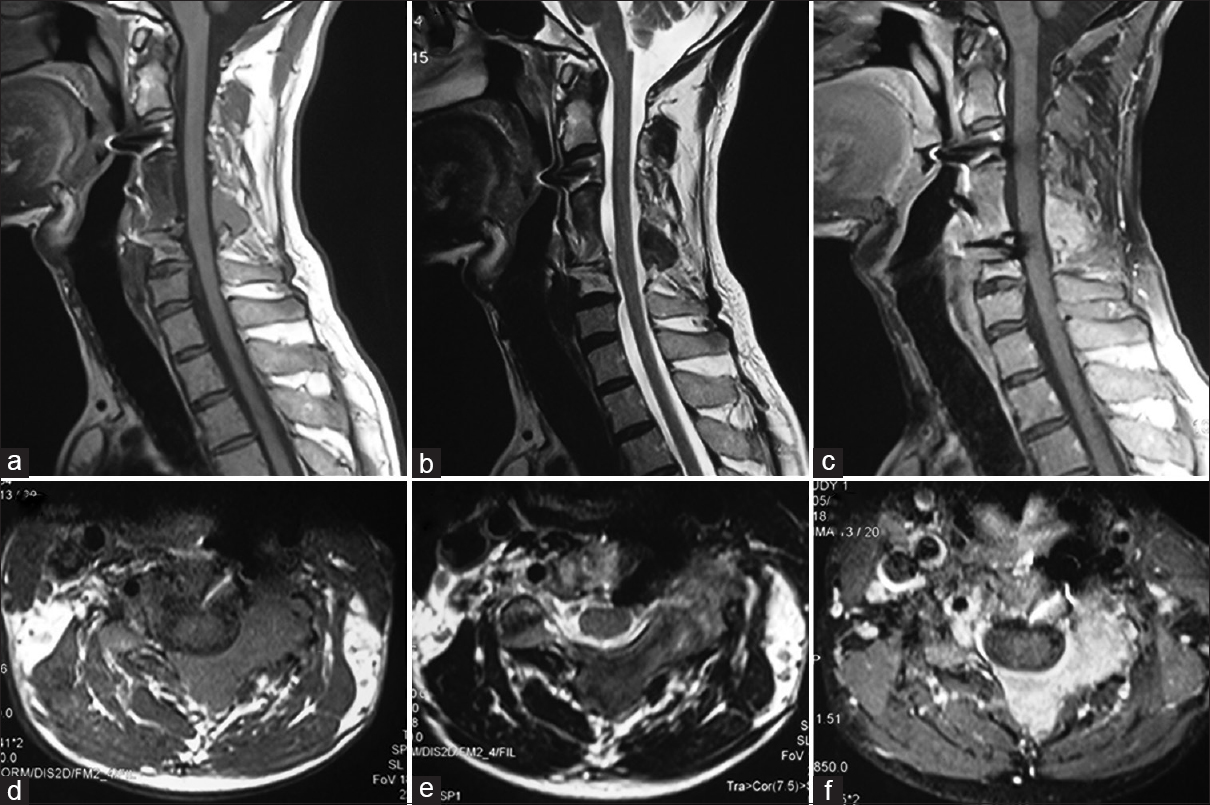
Postoperative Positron Emission Tomography (PET)-CT scan showed small, solitary, residual FDG (Fluorodeoxyglucose) avid lesion over the posterior elements of C4 and C5 vertebrae. Follow-up MRI at 10 months showed residual lesion centered at the left side lamina and spinous process of C4 and C5 vertebrae with no significant associated soft tissue component or recurrence [Figure
Figure 3
Follow-up MR imaging (at 10 months postsurgery): Sagittal T1-weighted (a), T2-weighted (b) and T1-weighted postcontrast (c) images depict spinal fixation with decompressed spinal cord. The T1-weighted (d), T2-weighted (e) and T1-weighted postcontrast (f) axial sections confirm the residual lesion along the left lateral arch of the vertebra with associated small soft tissue component
DISCUSSION
ABCs are expansile, benign, tumor-like lesions, commonly affecting long bones around the knee and occurring rarely in the vertebral column.[
In rare cases, the cystic components may be completely absent, and the tumor exhibits a solid architecture; making it impossible to differentiate from other solid bone tumors like osteosarcoma, GCT, etc.[
Clinical considerations
Solid variants of ABC are rare lesions, accounting for 3.4–7.5% of all ABCs, and most commonly affect long bones like femur and tibia.[
Radiological considerations
Routine radiography and CT shows an expansile, osteolytic lesion and both conventional and solid variant ABCs appear similar on it.[
Histopathological considerations
Among the differentials, giant-cell rich osteosarcoma, GCT, and s-ABC may show overlapping histological features. GCT shows many multinucleated, osteoclastic giant cells, admixed with round to slightly oval stromal cells showing similar nuclear character.[
Treatment strategy
For giant, solid, bony lesions involving the cervical spine (like the one described above), maximally safe resection followed by spinal stabilization should be the goal. The primary reason for this strategy is the fact that even after complete radiological evaluation, the pathology may vary within a wide spectrum, from benign (like s-ABC) to malignant (like giant-cell rich osteosarcoma). Hence, maximum benefit should be offered to the patient at first surgery. Adjuvant radiotherapy is not prescribed in view of benign nature of the lesion; and incidences of postradiation sarcoma and postradiation myelopathy. Long-term follow-up (up to 6 years) is available in literature, after treatment with resection or radiation; and it shows good prognosis, with no recurrence of lesions.[
Our patient has shown a good recovery after surgery and the follow-up MRI at 10-month follow-up shows adequate spinal cord decompression, without any increase in size of small residual posterior lesion.
CONCLUSION
Misdiagnosis of spinal s-ABC with solid bony tumors like GCT and giant-cell rich osteosarcoma is common. Hence, s-ABC should always be considered as a differential diagnosis in solid bony spinal lesions. Radiologically, these lesions appear similar; thus, histology needs to be carefully reviewed to differentiate between them. Though the initial treatment strategy in the form of maximally safe radical resection is the same for all three, the long-term outcome and recurrence rate is definitely better with s-ABC.
References
1. Bertoni F, Bacchini P, Capanna R, Ruggieri P, Biagini R, Ferruzzi A. Solid variant of aneurysmal bone cyst. Cancer. 1993. 71: 729-34
2. Feng D, Yang X, Liu T, Xiao J, Wu Z, Huang Q. Osteosarcoma of the spine: Surgical treatment and outcomes. World J Surg Oncol. 2013. 11: 89-
3. Junming M, Cheng Y, Dong C, Jianru X, Xinghai Y, Quan H. Giant cell tumor of the cervical spine: A series of 22 cases and outcomes. Spine (Phila Pa 1976). 2008. 33: 280-8
4. Karampalis C, Lenthall R, Boszczyk B. Solid variant of aneurysmal bone cyst on the cervical spine of a child: Case report, differential diagnosis and treatment rationale. Eur Spine J. 2013. 22: 523-31
5. Kinra P, Valdamani S, Singh V, Dutta V. Diaphyseal giant cell-rich osteosarcoma: Unusual histological variant in an unusual site. Indian J Pathol Microbiol. 2012. 55: 600-2
6. Pennekamp W, Peters S, Schinkel C, Kuhnen C, Nicolas V, Muhr G, Frangen TM. Aneurysmal bone cyst of the cervical spine (2008:7b). Eur Radiol. 2008. 18: 2356-60
7. Sanerkin NG, Mott MG, Roylance J. An unusual intraosseous lesion with fibroblastic, osteoclastic, osteoblastic, aneurysmal and fibromyxoid elements: “Solid” variant of aneurysmal bone cyst. Cancer. 1983. 51: 2278-86
8. Sato K, Sugiura H, Yamamura S, Takahashi M, Nagasaka T, Fukatsu T. Solid variant of an aneurysmal bone cyst (giant cell reparative granuloma) of the 3 rd lumbar vertebra. Nagoya J Med Sci. 1996. 59: 159-65
9. Suzuki M, Satoh T, Nishida J, Kato S, Toba T, Honda T. Solid variant of aneurysmal bone cyst of the cervical spine. Spine (Phila Pa 1976). 2004. 29: E376-81