- Department of Neurosurgery, Nagareyama Central Hospital, Chiba, Japan.
Correspondence Address:
Ryuzaburo Kanazawa, Department of Neurosurgery, Nagareyama Central Hospital, Chiba, Japan.
DOI:10.25259/SNI_656_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ryuzaburo Kanazawa, Takanori Uchida, Tetsuhiro Higashida, Saiko Watanabe, Takao Kono. Some technical options for successful PulseRider procedures. 17-Nov-2023;14:403
How to cite this URL: Ryuzaburo Kanazawa, Takanori Uchida, Tetsuhiro Higashida, Saiko Watanabe, Takao Kono. Some technical options for successful PulseRider procedures. 17-Nov-2023;14:403. Available from: https://surgicalneurologyint.com/surgicalint-articles/12637/
Abstract
Background: Unlike other conventional neck bridge stents, when using the PulseRider (PR), it is not necessary to introduce a microcatheter for stent delivery into the daughter branches from the neck, and it has less intraluminal metal. However, in some cases, securely introducing both leaflets into daughter vessels may be difficult, leading to coil herniation. This study aimed to present some technical issues in PR deployment.
Methods: Fourteen PR procedures were performed in our institution between August 2021 and June 2023, and T-type PRs were used in all procedures. Four technical points during PR procedures are presented from our experience, as “technical options (Options 1-4)”. All procedures were carried out with T-type PR implants.
Results: The PR was successfully placed in all interventions; however, in seven cases (50%), some technique trials were necessary because the leaflets did not unfold in the optimal directions. In Option 1, an introduction procedure with transposition of the daughter artery using a microcatheter is presented. In Option 2, the method for correction of the unfolded leaflet angle is demonstrated. In Option 3, another method for correction of the leaflets is shown. In Option 4, an effective method for neck protection during PR procedures is shown.
Conclusion: Various options should be considered to achieve appropriate apposition of PR leaflets. These technical options may be safe and effective for successful PR deployment.
Keywords: Aneurysmal embolization, Leaflet, PulseRider
INTRODUCTION
The main advantage of the PulseRider (PR) implant (Cerenovus, Irvine, CA, USA) is that microcatheter introduction into the daughter artery is essentially unnecessary,[
In our view, PR deployment breakthrough is classified into three types of pattern. First is the case of breakthrough when extra-aneurysmal placement could not be achieved, such as when hybrid- or intra-aneurysmal deployment is possible but ineffective for safe coil embolization (demonstrated in option 1). Second is the case of a breakthrough with the inappropriate unfolding of the leaflets, which requires replacement (demonstrated in options 2 and 3). The third consists of circumstances that bring out the best performance of the PR during coil insertion and the first coil frame formation in particular (described in option 4).
METHODS
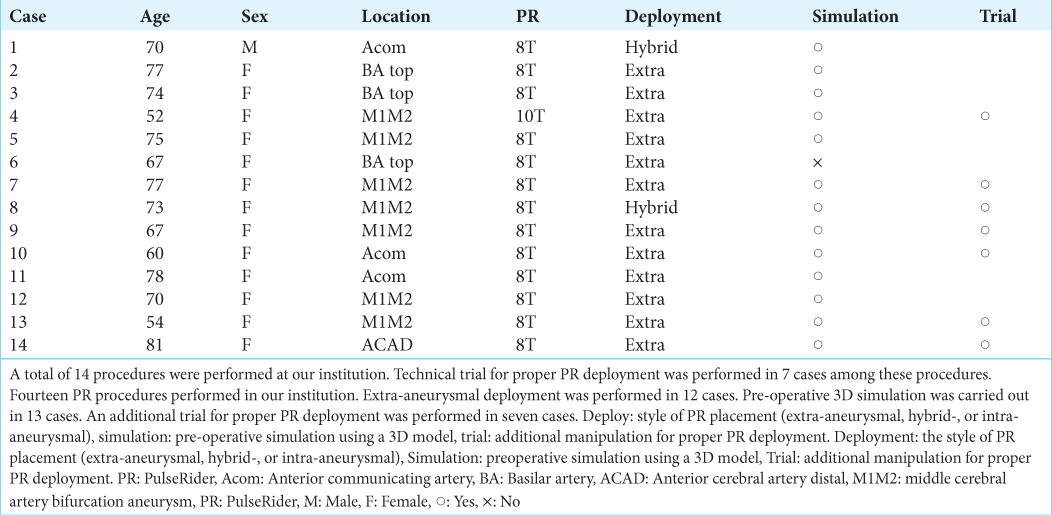
Fourteen PR procedures were performed in our institution between August 2021 and June 2023 [
TECHNICAL OPTIONS
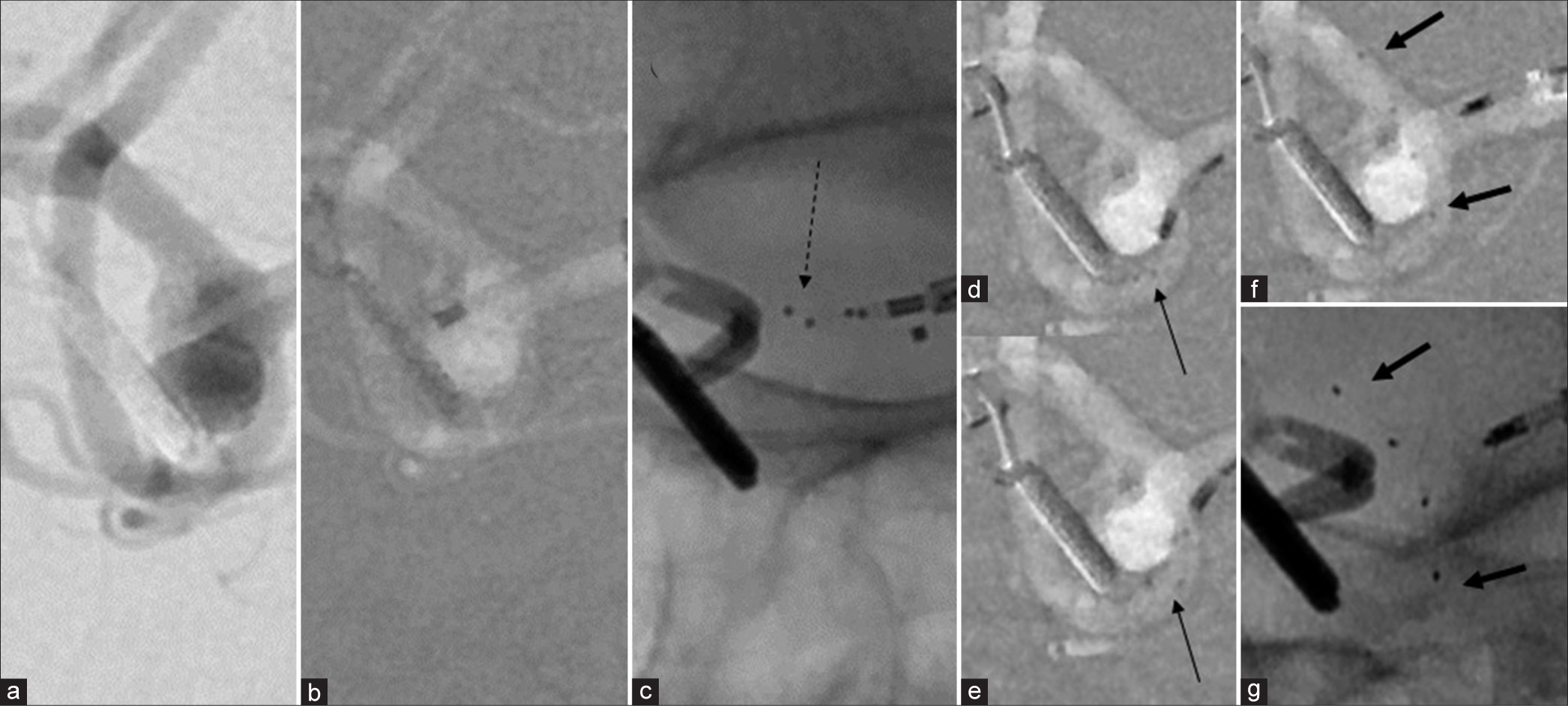
Option 1 (Case 5)
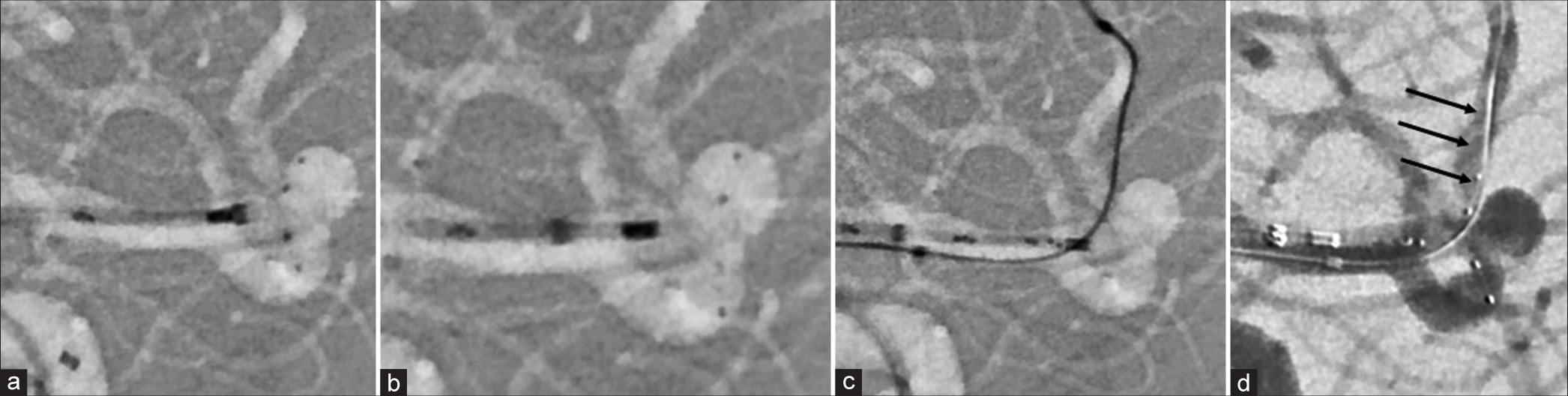
This option was employed in a case with a middle cerebral artery (MCA) aneurysm. The leaflets were unfolded in the proper directions, but one leaflet entered inside the aneurysm; hybrid placement was ineffective in this case. A microcatheter (Echelon 10 MicroCatheter, 90° angle; Medtronic, Dublin, Ireland) was introduced into the upper M2 trunk for transposition of the artery to reduce the acute angle of the branch, resulting in the successful introduction of the leaflet [
Figure 1:
(a and b) Hybrid placement of the pulse rider (PR). Both situations are ineffective for aneurysm treatment. (c) Microcatheter insertion into the upper branch of the middle cerebral artery (MCA) for transposition of the branch. (d) Successful navigation of the leaflet is achieved. Arrows, (d) Reduction of the angle of the daughter artery origin is noted.
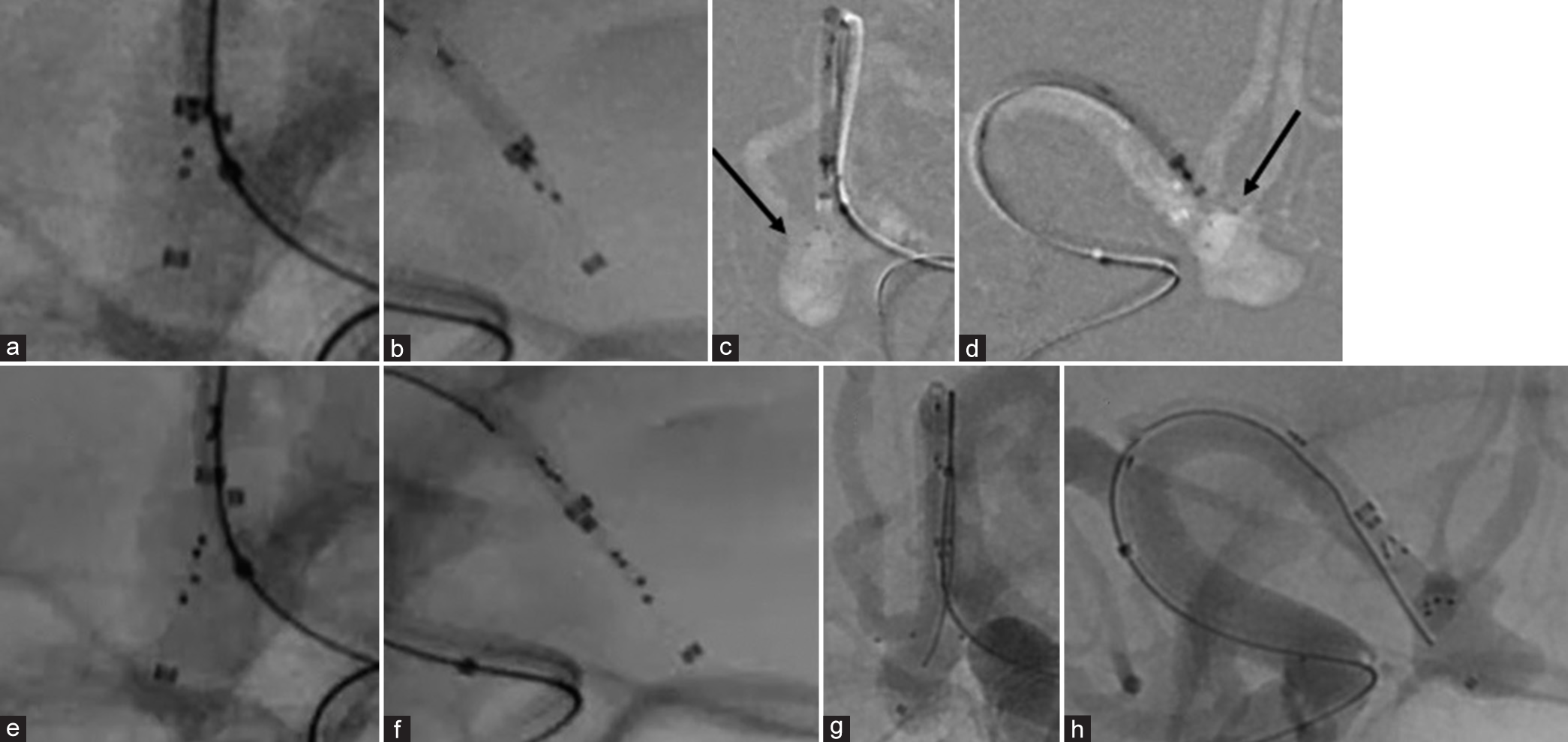
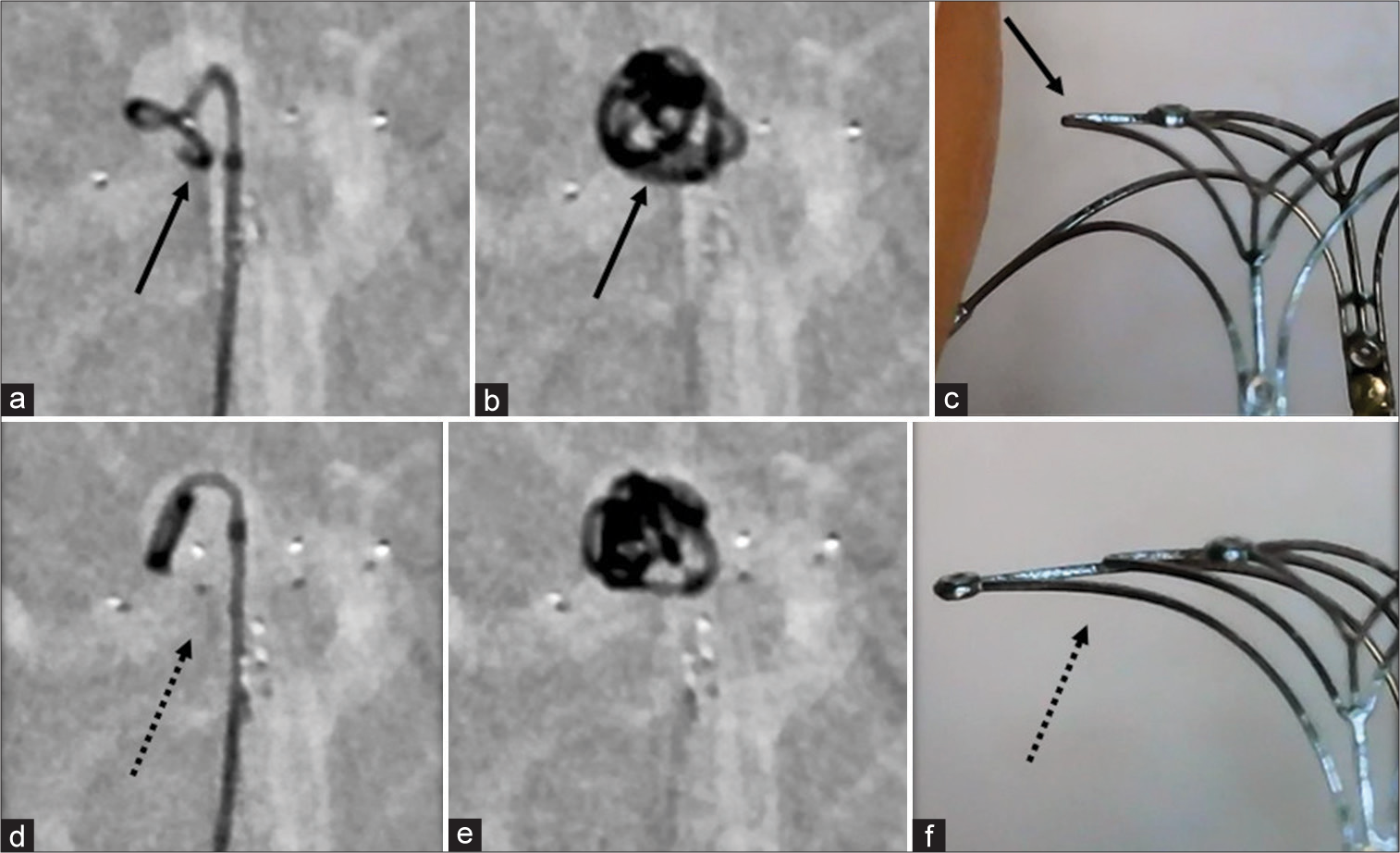
Option 2 (Case 10)
This option was employed in a case with an anterior communicating artery aneurysm. The leaflets were deployed with a tangent angle against the daughter arteries [
Figure 2:
(a and b) Fluoroscopic image before PulseRider unfolding. Arrow, (c and d) Deployment to the tangent angle against the daughter branches during the first trial. (e and f) After rotating the stent 90 degrees outside the microcatheter, the second trial of PR deployment is performed. (g and h) Resulting in successful positioning of the implant.
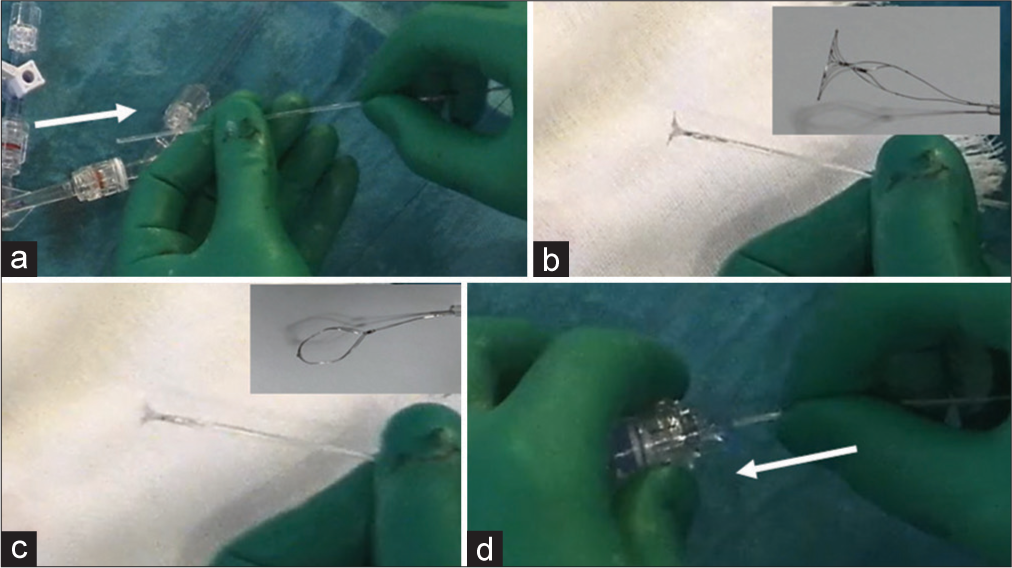
Figure 3:
(a) Pulling the stent back into the introducer sheath (white arrow); (b)Pushing the stent without any torque; (c) Unfolded leaflets being rotated in the appropriate degree under visual confirmation; (d) The stent being re-inserted carefully without any rotation of the system (white arrow). Each photo above to the right of b (before rotation) and c (after rotation) shown for reference.
Option 3 [Case 4]
This option was employed in a case of recurrence of an MCA aneurysm after clipping. The leaflets were not unfolded properly despite several attempts. The microcatheter was introduced into a daughter artery and then gently pulled back with the opening of the tips of the leaflets, which resulted in the successful placement of the PR. We also used this method in one other case (Case 8).
This method may pose a severe risk of vessel rupture, so this should be attempted only when the space around the aneurysm neck and the daughter vessel is relatively large [
Figure 4:
(a and b) Middle cerebral artery aneurysm recurrence 10 years after clipping. c: dotted arrow: The PR is not opened correctly. (d and e) thin arrow: Carefully and slowly pulling back the microcatheter being introduced to the daughter artery as the leaflets open slightly. (f and g) Bold arrows: Resulting in successful placement of the PR.
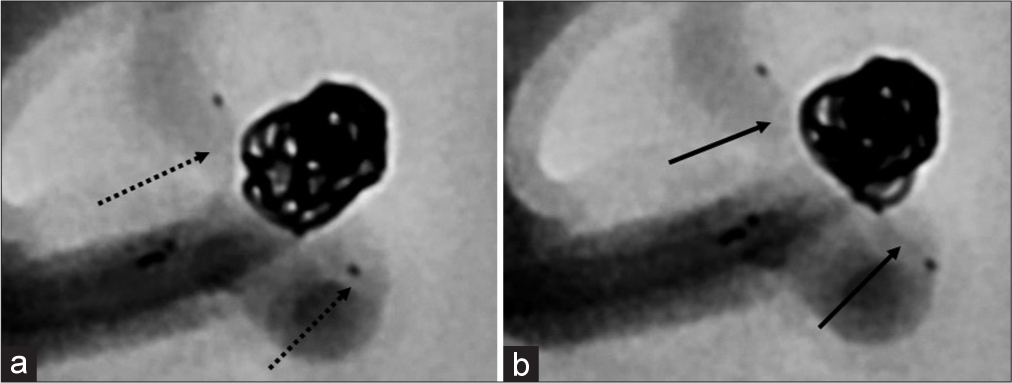
Option 4 (Case 5)
This option was employed in the case of a suspected MCA aneurysm. Inadequate neck protection can occur in PR procedures. Strict apposition of the PR to the neck during the first coil placement may result in coil herniation through the strut and entanglement of the coil and strut [
Figure 5:
(a and b) The first coil herniating through the leaflet during PR placement at the neck before coil insertion (arrow); (c) Because of the loose leaflets (arrow); (d) Pulling the stent back from the neck appropriately (dotted arrow); (e) Effective and optimal situation for the neck protection is achieved; (f) Because of efficacious implant positioning (dotted arrow).
RESULTS
In our experience, the PR was successfully placed in all interventions; however, in seven cases (50%), some technique trials were necessary because the leaflets did not unfold in the optimal directions. The most important issue in PR deployment is whether the leaflets can be optimally unfolded toward each daughter’s vessel. The leaflets unfolded successfully in Case 5 (Option 1). However, a leaflet could not initially be introduced into the M2 branch; inserting another microcatheter (Echelon-10) into the branch was performed to reduce the angle of the branch origin, resulting in successful navigation of the leaflet. This was an option when PR unfolding was optimal, but either leaflet was not in the daughter vessel. Echelon-10 was desirable for this situation because it is relatively stiff compared to other microcatheters. In Cases 9 and 10 (option 2), the leaflets were deployed at incorrect angles and needed to be adjusted. Pulling the delivery wire back with some torque and pushing the stent out again are recommended in such situations.[
DISCUSSION
It is unnecessary to navigate the microcatheter for stent delivery into the daughter vessel during PR procedures.[
The PR deployment success rate was 97.5% in the surveyed literature, whereas in the Japanese cases, it was lower (372/418 cases, 90%; as of September 30, 2022) (data provided courtesy of Cerenovus). It is not clear why the rate of successful placement was lower in Japan than elsewhere. In Japan, surgeons can run simulations before the procedure using a 3D model of the patient. The rate of successful placement was 94% in cases with preoperative simulation, whereas it was 84% without such simulation (data provided courtesy of Cerenovus). Using such simulations, it is possible to attempt many technical scenarios that may occur during actual procedures, including what was presented in the present paper. In our opinion, surgeons should engage in technique trials as much as possible to maximize their chances of successfully deploying the PR. Such simulations may contribute to surgeons’ ability to confirm the necessary technical manipulations and help them overcome difficulties encountered during procedures. In addition, the abovementioned technical ideas may contribute to successful PR procedures.
Options 1 and 2 may be worthwhile to obtain favorable PR leaflet placement. Option 1 is slightly complicated but maybe a breakthrough when the extra-aneurysmal placement is practical and essential. Option 2 presents a lower risk because whole steps are performed outside the patient’s body. These may be suitable alternative methods for the correction of PR leaflets. On the other hand, Option 3 should be a last resort because it may be risky if there is not enough space around the aneurysm neck and daughter artery. A pitfall during the first coil insertion in PR procedures was shown in Option 4. Strict apposition of the PR to the aneurysm neck before the first coil placement is not desirable because the PR strut may loosen, causing coil herniation or entanglement of the stent and coil. To prevent this, the PR should be positioned slightly proximal to the neck and gently pushed forward to the channel after the first coil placement.[
CONCLUSION
The advantages of the PR may be maximized if each PR leaflet is navigated in the optimal direction. This paper presented four technical options for PR deployment with minimal trials. Technique trials were conducted in preoperative simulations before each procedure and were effective. Some technical options shown in the present study and preoperative practice using 3D models may be important for improving the success rate of PR procedures.
Ethical approval
The author(s) declare they have taken the ethical approval from IIRB/IEC (NCH2023-4).
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgments
The authors would like to thank the radiologists at their hospital for their dedicated assistance during the procedures. The authors also wish to express their heartfelt thanks to Cerenovus staff for providing Japanese data.
References
1. Aguilar-Salinas P, Brasiliense LB, Walter CM, Hanel RA, Dumont TM. Current status of the PulseRider in the treatment of bifurcation aneurysms: A systematic review. World Neurosurg. 2018. 115: 288-94
2. Gory B, Spiotta AM, Di Paola F, Mangiafico S, Renieri L, Consoli A. PulseRider for treatment of wide-neck bifurcation intracranial aneurysms: 6-month results. World Neurosurg. 2017. 99: 605-9
3. Gory B, Spiotta AM, Mangiafico S, Consoli A, Biondi A, Pomero E. PulseRider stent-assisted coiling of wide-neck bifurcation aneurysms: Periprocedural results in an international series. AJNR Am J Neuroradiol. 2016. 37: 130-5
4. Khattak YJ, Sibaie AA, Anwar M, Sayani R. Stents and stent mimickers in endovascular management of wide-neck intracranial aneurysms. Cureus. 2018. 10: e3420
5. Limbucci N, Cirelli C, Valente I, Nappini S, Renieri L, Laiso A. Y-stenting versus PulseRider-assisted coiling in the treatment of wide-neck bifurcation aneurysms: Role of anatomical features on midterm results. Neurosurgery. 2020. 87: 329-37
6. Mukherjee S, Chandran A, Gopinathan A, Putharan M, Goddard T, Eldridge PR. PulseRider-assisted treatment of wide-necked intracranial bifurcation aneurysms: Safety and feasibility study. J Neurosurg. 2017. 127: 61-8
7. Pranata R, Yonas E, Vania R, Sidipratomo P, July J. Efficacy and safety of PulseRider for treatment of wide-necked intracranial aneurysm-A systematic review and meta-analysis. Interv Neuroradiol. 2021. 27: 60-7
8. Sakai N, Imamura H, Arimura K, Funatsu T, Beppu M, Suzuki K. PulseRider-assisted coil embolization for treatment of intracranial bifurcation aneurysms: A single-center case series with 24-month follow-up. World Neurosurg. 2019. 128: e461-7
9. Spiotta AM, Chaudry MI, Turner RD, Turk AS, Derdeyn CP, Mocco J. An update on the adjunctive neurovascular support of wide-neck aneurysm embolization and reconstruction trial: 1-year safety and angiographic results. AJNR Am J Neuroradiol. 2018. 39: 848-51
10. Spiotta AM, Derdeyn CP, Tateshima S, Mocco J, Crowley RW, Liu KC. Results of the ANSWER trial using the PulseRider for the treatment of broad-necked, bifurcation aneurysms. Neurosurgery. 2017. 81: 56-65
11. Spiotta AM, Sattur MG, Kan P, Crowley RW. Bifurcation aneurysm treatment with PulseRider: Technical nuances, device selection, positioning strategies, and overcoming geometric challenges. World Neurosurg. 2020. 142: 339-51
12. Srinivasan VM, Srivatsan A, Spiotta AM, Hendricks BK, Ducruet AF, Albuquerque FC. Early postmarket results with PulseRider for treatment of wide-necked intracranial aneurysms: A multicenter experience. J Neurosurg. 2019. 133: 1756-65
13. Suyama K, Nakahara I, Matsumoto S, Morioka J, Hasebe A, Tanabe J. Brainstem infarctions caused by a proximal marker of the PulseRider device obstructing the origin of a perforator. J Stroke Cerebrovasc Dis. 2022. 31: 106332