- Department of Neurosurgery, King Abdulaziz University Hospital, Jeddah, Saudi Arabia
- Department of Neurosurgery, King Abdullah Medical City, Makkah, Saudi Arabia
- Department of Neurosurgery, King Abdulaziz Medical City, Ministry of the National Guard-Health Affairs, King Abdullah International Medical Research Center, Makkah, Saudi Arabia
- Department of Neuroradiology, King Abdullah Medical City, Makkah, Saudi Arabia.
Correspondence Address:
Abdulrahman Marzouq AlMutairi, Department of Neurosurgery, King Abdulaziz University Hospital, Jeddah, Saudi Arabia.
DOI:10.25259/SNI_933_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Abdulrahman Marzouq AlMutairi1, Mubasher Ahmed2, Abdulaziz Abdullah Basurrah2, Fayez Dhafer Alshehri3, Zaina Brinji4, Naseem Albargi4, Ahmed Adel Farag2. Spinal adhesive arachnoiditis after spinal anesthesia complicated by communicating hydrocephalus – A case report. 23-Feb-2024;15:54
How to cite this URL: Abdulrahman Marzouq AlMutairi1, Mubasher Ahmed2, Abdulaziz Abdullah Basurrah2, Fayez Dhafer Alshehri3, Zaina Brinji4, Naseem Albargi4, Ahmed Adel Farag2. Spinal adhesive arachnoiditis after spinal anesthesia complicated by communicating hydrocephalus – A case report. 23-Feb-2024;15:54. Available from: https://surgicalneurologyint.com/surgicalint-articles/12766/
Abstract
Background: Adhesive arachnoiditis (AA) is a debilitating condition characterized by chronic inflammation of the arachnoid membrane, leading to the formation of intrathecal scars and dural adhesions. The etiology of AA is multifactorial, including factors such as infections, trauma, and iatrogenic damage. We present a case of a female patient who developed communicating hydrocephalus after spinal anesthesia complicated by severe AA.
Case Description: A 33-year-old female underwent a cesarean section with epidural anesthesia. Five hours postoperatively, she experienced transient difficulty standing, which was resolved with assistance. Weeks later, she developed a severe holocephalic headache accompanied by nausea, vomiting, photophobia, and phonophobia. Imaging revealed hydrocephalus and pronounced AA. Lumbar puncture provided symptomatic improvement. The patient underwent ventriculoperitoneal shunt insertion, resulting in further symptom improvement and successful shunt function.
Conclusion: AA is a challenging condition associated with inflammation and scarring of the arachnoid membrane. The development of hydrocephalus following epidural anesthesia, in this case, highlights a rare manifestation of arachnoiditis. Further research and documentation are needed to understand better the underlying mechanisms and risk factors contributing to hydrocephalus in the context of AA following epidural anesthesia.
Keywords: Adhesive arachnoiditis, Complications, Epidural anesthesia, Hydrocephalus
INTRODUCTION
Adhesive arachnoiditis (AA) is an incapacitating pathological state distinguished by enduring inflammation of the arachnoid membrane, resulting in the formation of intrathecal scars and dural adhesions.[
CASE REPORT
We present the case of a 33-year-old female patient who underwent a cesarean section procedure under epidural anesthesia. Five hours after the surgery, she experienced transient difficulty standing, which was resolved with assistance. She was discharged from the hospital after two days without any other complaints. However, several weeks later, she developed a severe holocephalic headache that was unresponsive to analgesics and persisted throughout the day, significantly impacting her sleep. The headache was accompanied by symptoms such as nausea, vomiting, photophobia, and phonophobia, prompting her to seek medical attention.
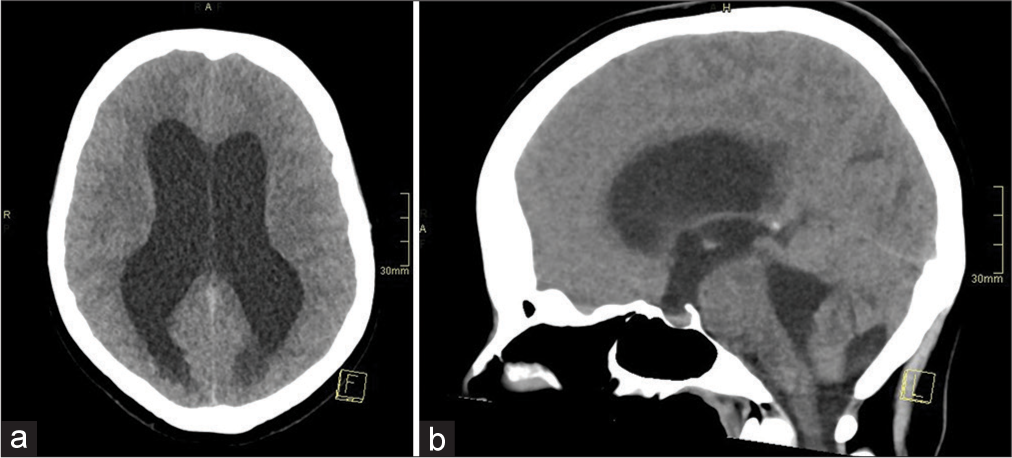
On admission for further evaluation, a computed tomography (CT) brain scan revealed the presence of acute hydrocephalus, as shown in
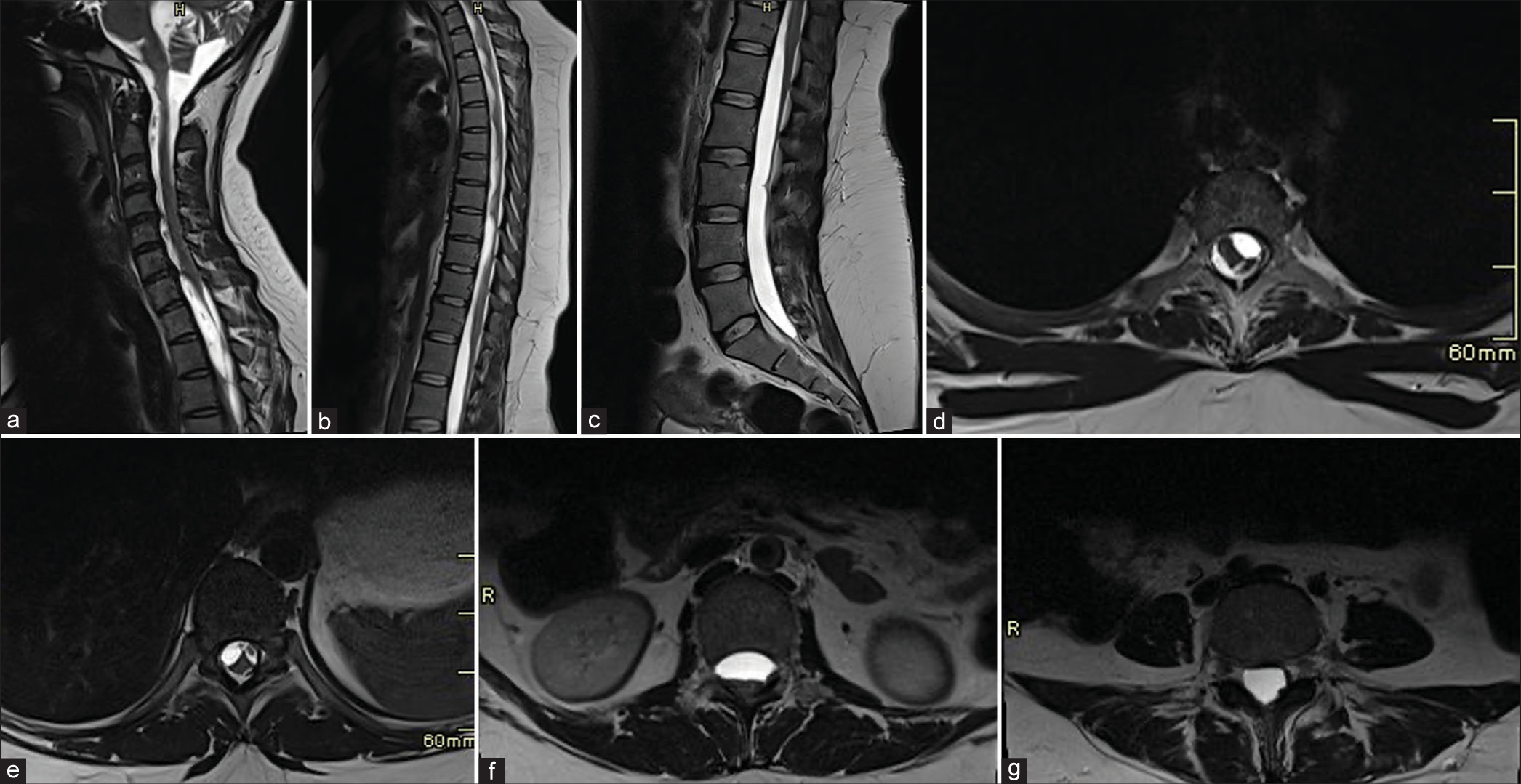
Figure 2:
(a-g) Findings suggestive of Adhesive Arachnoiditis. Sagittal and axial magnetic resonance imaging of the spine without contrast reveals adherent cauda equina nerve roots to the thecal sac, associated with extensive intradural cerebrospinal fluid-like multiloculations extending up to the lower cervical spine encasing the thoracic cord.
To gain more insights into the underlying etiology, a lumbar puncture was performed, and CSF samples were obtained. The analysis of the CSF samples revealed normal results. Remarkably, following the lumbar puncture, the patient experienced symptomatic improvement.
After confirming the diagnosis, the patient underwent ventriculoperitoneal shunt insertion. Following the procedure, her symptoms continued to improve, and a postoperative CT scan confirmed the satisfactory function of the shunt. Consequently, the patient was discharged home in a stable clinical condition.
DISCUSSION
AA is an incapacitating pathological state distinguished by enduring inflammation of the arachnoid membrane, resulting in the formation of intrathecal scars and dural adhesions.[
Interestingly, our patient presented with hydrocephalus after 5 h of the epidural anesthesia. Hydrocephalus is defined as the abnormal accumulation of CSF within the brain, and it is an infrequent complication observed in the context of adhesive spinal arachnoiditis subsequent to epidural anesthesia. This occurrence represents a rare manifestation of arachnoiditis, highlighting the challenges associated with its prediction in patients presenting with lower-limb weakness following epidural anesthesia and complaints suggestive of increased intracranial pressure. Given the atypical nature of this presentation, further investigation and documentation of similar cases are warranted to enhance our understanding of the underlying mechanisms and potential risk factors contributing to the development of hydrocephalus in the context of adhesive spinal arachnoiditis following epidural anesthesia.
CONCLUSION
AA is a complex condition characterized by chronic inflammation and the formation of scar tissue in the arachnoid membrane. Its true incidence is uncertain and often underestimated. The condition is multifactorial, with various causes, including infections, trauma, and iatrogenic factors. It poses challenges in diagnosis and treatment due to the avascular nature of the arachnoid and the continuous circulation of CSF. Hydrocephalus, while rare, can occur as a complication in some cases. Further research is needed to understand the underlying mechanisms better, predict such complications, and improve patient outcomes.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Anderson TL, Morris JM, Wald JT, Kotsenas AL. Imaging appearance of advanced chronic adhesive arachnoiditis: A retrospective review. Am J Roentgenol. 2017. 209: 648-55
2. Bourne IH. Lumbo-sacral adhesive arachnoiditis: A review. J R Soc Med. 1990. 83: 262-5
3. Chattopadhyay I, Jha AK, Banerjee SS, Basu S. Post-procedure adhesive arachnoiditis following obstetric spinal anaesthesia. Indian J Anaesth. 2016. 60: 372
4. Delamarter RB, Ross JS, Masaryk TJ, Modic MT, Bohlman HH. Diagnosis of lumbar arachnoiditis by magnetic resonance imaging. Spine. 1990. 15: 304-10
5. Hernández-Albújar S, Arribas JR, Royo A, González-García JJ, Peña JM, Vázquez JJ. Tuberculous radiculomyelitis complicating tuberculous meningitis: Case report and review. Clin Infect Dis. 2000. 30: 915-21
6. Peng H, Conermann T, editors. Arachnoiditis. StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. p.
7. Rice I, Wee MY, Thomson K. Obstetric epidurals and chronic adhesive arachnoiditis. Br J Anaesth. 2004. 92: 109-20
8. Sharma A, Goyal M, Mishra NK, Gupta V, Gaikwad SB. MR imaging of tubercular spinal arachnoiditis. AJR Am J Roentgenol. 1997. 168: 807-12
9. Wright MH, Denney LC. A comprehensive review of spinal arachnoiditis. Orthop Nurs. 2003. 22: 215-9