- Department of Neurosurgery, Graduate School of Biomedical and Health Sciences, Hiroshima University, Hiroshima, Japan,
- Department of Neurosurgery, University of Iowa Hospitals and Clinics, Iowa City, Iowa.
Correspondence Address:
Kiyoharu Shimizu
Department of Neurosurgery, University of Iowa Hospitals and Clinics, Iowa City, Iowa.
DOI:10.25259/SNI_80_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kiyoharu Shimizu1, Takafumi Mitsuhara1, Masaaki Takeda1, Satoshi Yamaguchi2. Spinal arteriovenous fistula in the lipoma of the filum terminale: A report of two cases and literature review. 17-Mar-2021;12:103
How to cite this URL: Kiyoharu Shimizu1, Takafumi Mitsuhara1, Masaaki Takeda1, Satoshi Yamaguchi2. Spinal arteriovenous fistula in the lipoma of the filum terminale: A report of two cases and literature review. 17-Mar-2021;12:103. Available from: https://surgicalneurologyint.com/surgicalint-articles/10648/
Abstract
Background: Filum terminale arteriovenous fistulas (FTAVFs) are rare and their pathogenesis remains unknown. The authors report two cases of FTAVF that arose in the lipoma of the filum terminale.
Case Description: The two patients were 72 and 76 years of age, and both presented with a progressive paraparesis. The first patient had an arteriovenous fistula (AVF) located at L5 that was supplied by the anterior spinal artery originating from the left T10 intercostal artery. The second patient’s AVF at L3-4 was fed by the anterior spinal artery originating from the left T8 intercostal artery. Both patients underwent partial resection of the filum terminale at the location of the shunts. The pathological examinations revealed that both the AVFs were embedded in the adipose tissue of the filum terminale, revealing the fatty fila that were not visible in preoperative magnetic resonance images.
Conclusion: Two cases of FTAVF were successfully treated by obliterating the fistulas through partial resection of the affected fatty filum terminale. The literature review revealed 13 cases of FTAVF concomitant with the lipomas of the filum terminale. Resection and histological evaluation of the filum terminale should be performed to treat and elucidate the pathogenesis of FTAVF.
Keywords: Fatty filum terminale, Filum terminale arteriovenous fistula, Pathology
INTRODUCTION
Filum terminale arteriovenous fistulas (FTAVFs) represent 3.1% of all intradural AVFs and <5% of spinal intradural arteriovenous malformations.[
CASE REPORT
Case 1
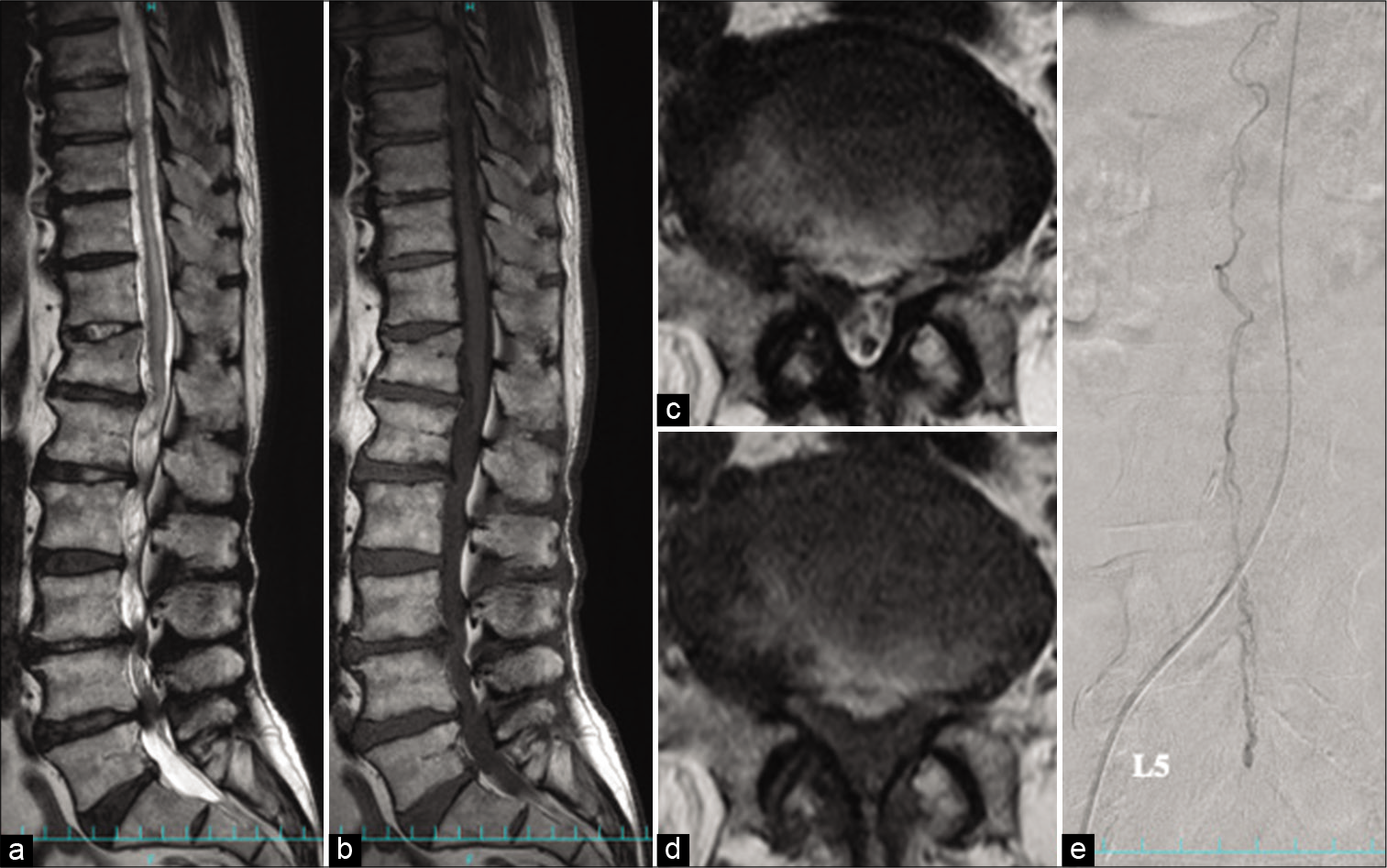
A 72-year-old male presented with a 5-year history of a progressive lower extremity paraparesis and hypesthesia below the L2 dermatome level. The preoperative T2-weighted magnetic resonance imaging (MRI) revealed edema plus flow voids in the lower spinal cord including the conus medullaris accompanying lumbar canal stenosis from L3 to L5 [
Figure 1:
Filum terminale arteriovenous fistula at L5 (Case 1). (a) Sagittal T2-weighted magnetic resonance image (MRI) shows the swollen spinal cord surrounded by flow voids. It also shows redundant cauda equina and spinal canal stenosis from L3 to L5. (b) Sagittal T1-weighted MRI does not show high signal intensity in the filum terminale. (c and d) Axial T1- and T2-weighted MRIs at L5 indicate thickened filum terminale due to edema, although the fatty component is not evident. (e) Selective catheter angiography from left T10 intercostal artery shows an arteriovenous fistula located at L5 that is fed by a caudally running artery in the filum terminale. The drainer is a vein in the filum terminale with an ascending flow.
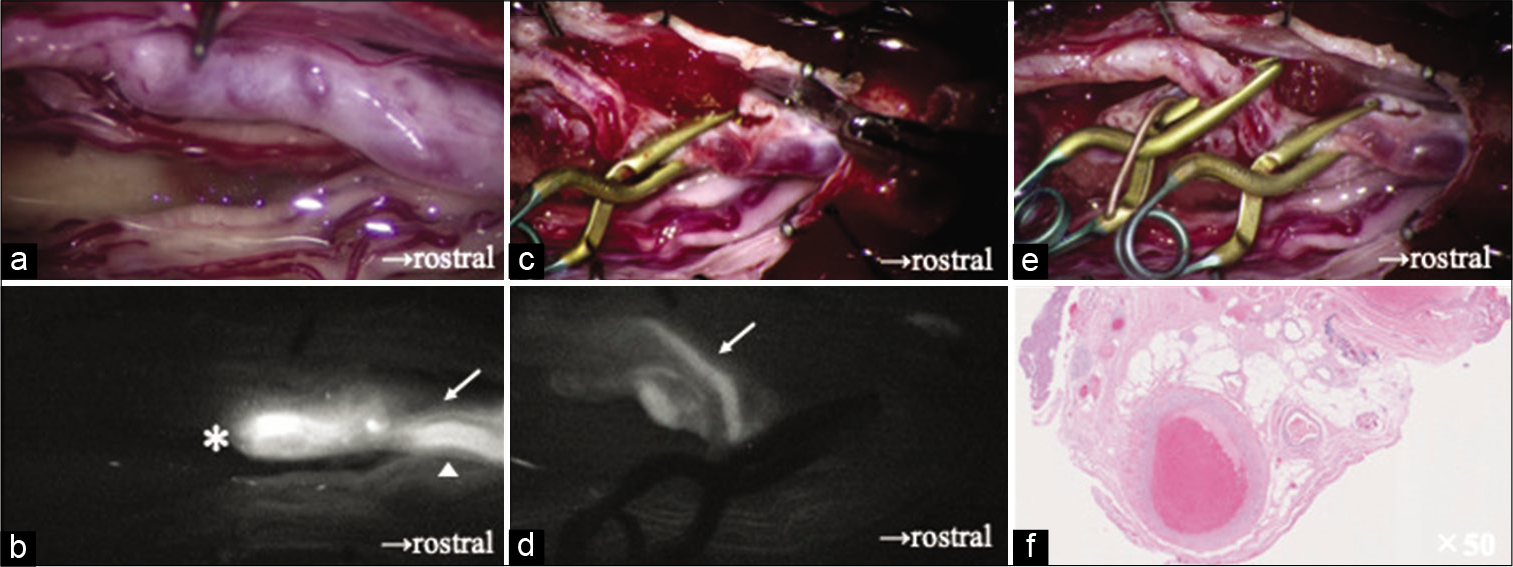
Figure 2:
Case 1 continued. (a) Intraoperative findings show edematous filum terminale with dilated arteries and veins, (b) Intravenous indocyanine green (ICG) video angiogram shows the artery of the filum terminale (AFT) with a caudal inflow (arrow), connecting directly with the vein in the filum terminale drained rostrally (arrowhead), The transitional point from the artery to the vein was considered as the arteriovenous fistula (AVF) (asterisk), (c) A temporary aneurysm clip is applied on the AFT immediately proximal to the shunting point, (d) intravenous ICG angiogram shows another minor feeding artery (arrow) joining the AVF with a caudal inflow, (e) one more temporary aneurysm clip is applied to the minor feeding artery, (f) the pathological finding of resected filum terminale shows an arterialized vein embedded in the adipose tissue (hematoxylin and eosin stain, ×50).
Case 2
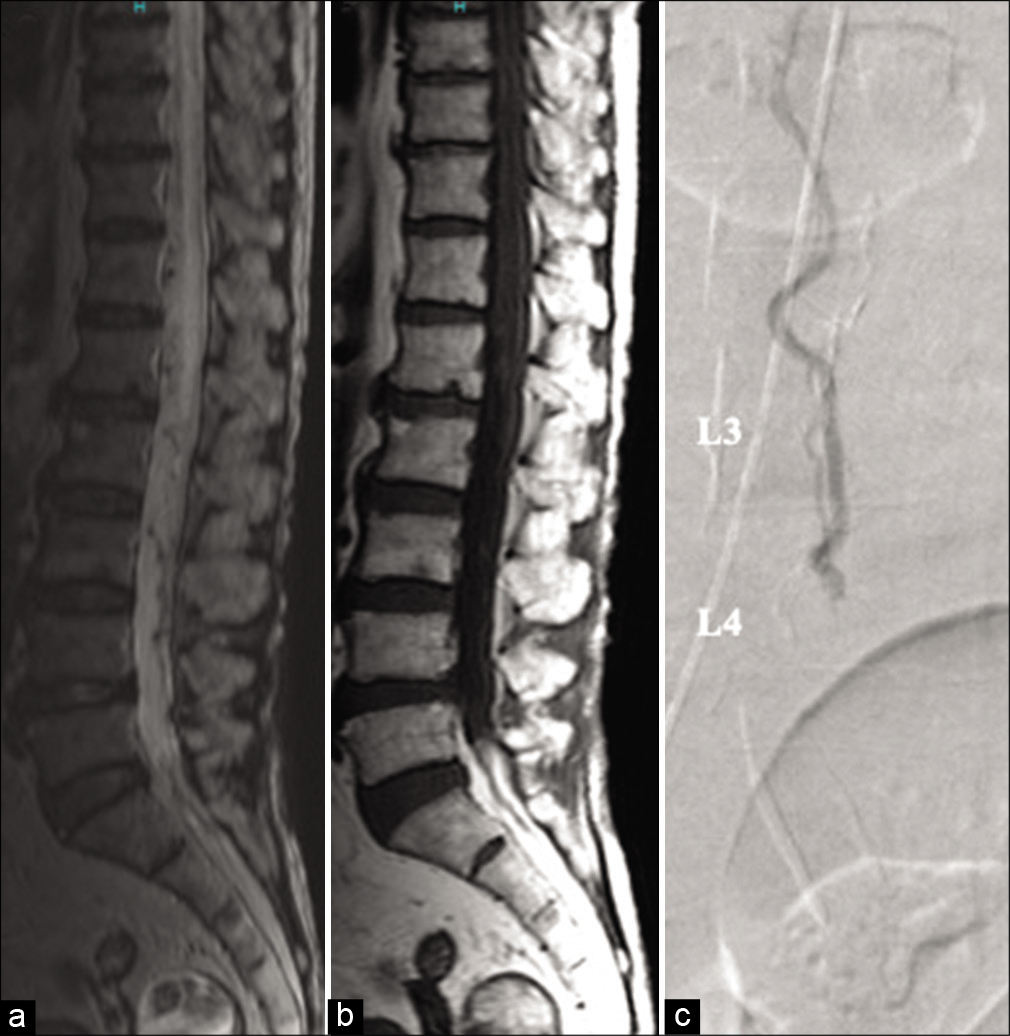
A 76-year-old female also presented with a progressive paraparesis and gradual onset of urinary retention. Sagittal T2-weighted MRI of the thoracic and lumbar spine revealed edema of the spinal cord with flow voids around it [
Figure 3:
Filum terminale arteriovenous fistula at L3-4 (case 2). (a) Sagittal T2-weighted magnetic resonance image (MRI) shows edematous spinal cord and perimedullary flow voids, (b) spinal lipoma is not recognized on sagittal T1-weighted MRI, (c) selective catheter angiography from left T8 intercostal artery shows an arteriovenous fistula located at the L5 level supplied by an artery that originated from the anterior spinal artery.
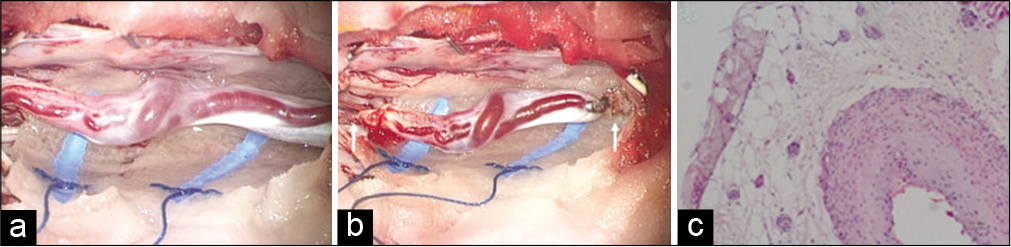
Figure 4:
Case 2 continued. (a) Intraoperative finding shows edematous filum terminale with dilated arteries and veins. (b) The filum terminale is resected with the arteriovenous fistula (arrow). (c) The histopathological study of the resected filum terminale shows an arterialized vein surrounded by the adipose tissue.
DISCUSSION
Review of the literature regarding FTAVF concomitant with the lipomas of the filum terminale
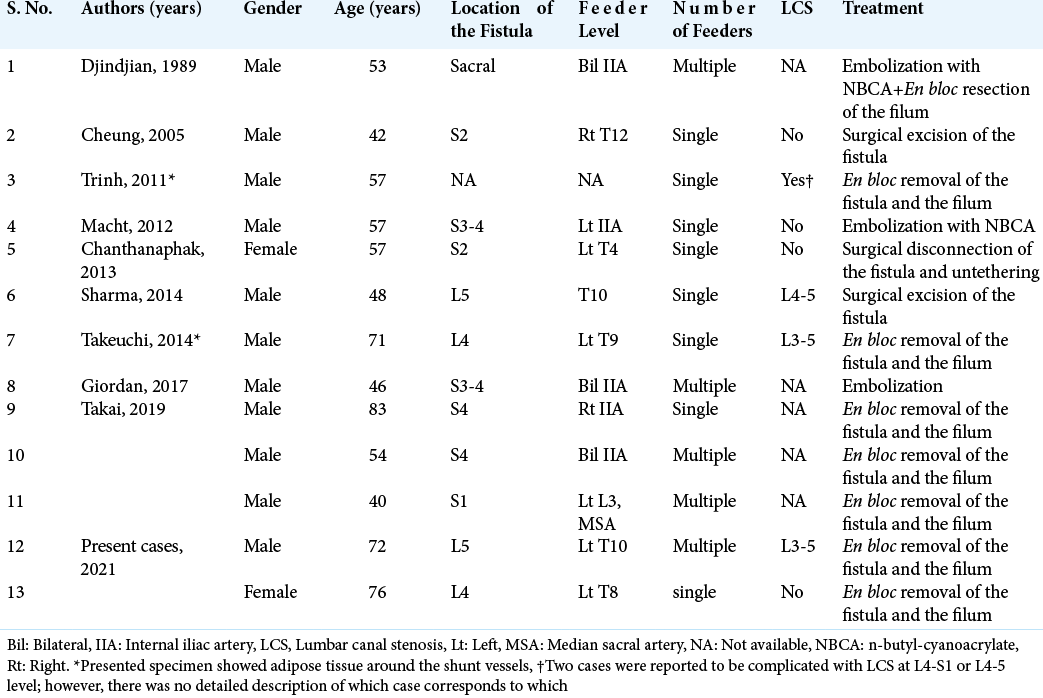
We reviewed a total of thirteen cases with concomitant FTAVF and fatty fila; this included our two cases reported above [
Etiology of FTAVF
Given that FTAVF itself occurs rarely, the number of 13 cases with two coexistent pathologies led us to believe that there might be an association between the two pathologies.[
The role of resection and histological evaluation of the filum terminale as a background of FTAVFs
Brown et al. found lipomas in the filum terminal with an incidence of 4% from randomly selected lumbosacral spine MRIs.[
CONCLUSION
This study provides indicate a possible association between FTAVF and fatty filum terminale. Resection is appropriate curative treatment, and histological evaluation of the filum terminale should be performed to elucidate the pathogenesis of AVF.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Brown E, Matthes JC, Bazan C, Jinkins JR. Prevalence of incidental intraspinal lipoma of the lumbosacral spine as determined by MRI. Spine (Phila Pa 1976). 1994. 19: 833-6
2. Cohrs G, Drucks B, Synowitz M, Held-Feindt J, KnerlichLukoschus F. Expression patterns of hypoxia-inducible factors, proinflammatory, and neuroprotective cytokines in neuroepithelial tissues of lumbar Spinal lipomas-a pilot study. World Neurosurg. 2020. 141: e633-44
3. Iampreechakul P, Tirakotai W, Wangtanaphat K, Lertbutsayanukul P, Siriwimonmas S. Filum terminale arteriovenous fistula in association with degenerative lumbosacral spinal canal stenosis: Report of 3 cases and review of the literature. World Neurosurg. 2020. 138: 231-41
4. Selçuki M, Vatansever S, Inan S, Erdemli E, Bağdatoğlu C, Polat A. Is a filum terminale with a normal appearance really normal?. Childs Nerv Syst. 2003. 19: 3-10
5. Sharma P, Ranjan A, Lath R. Arteriovenous fistula of the filum terminale misdiagnosed and previously operated as lower lumbar degenerative disease. Asian Spine J. 2014. 8: 365-70
6. Takai K, Komori T, Taniguchi M. Angioarchitecture of filum terminale arteriovenous fistulas: Relationship with a tethered spinal cord. World Neurosurg. 2019. 122: e795-804
7. Takeuchi M, Niwa A, Matsuo N, Joko M, Nakura T, Aoyama M. Pathomorphological description of the shunted portion of a filum terminale arteriovenous fistula. Spine J. 2014. 14: e7-10
8. Trinh VT, Duckworth EA. Surgical excision of filum terminale arteriovenous fistulae after lumbar fusion: Value of indocyanine green and theory on origins (a technical note and report of two cases). Surg Neurol Int. 2011. 2: 63